Polyarthritis
Table of Contents
What is polyarthritis?
The name polyarthritis is derived from two Greek words: “poly,” meaning “many, much” and “arthron,” meaning “joint”
Polyarthritis is a word used when at least five joints are affected by arthritis. Several different diseases ranging from rheumatoid arthritis to infectious conditions can lead to polyarthritis. Anamnesis, physical examination, laboratory findings, and imaging methods are important tools for diagnosis.
Polyarthritis refers to a joint disease that includes at least five joints. One or more signs of inflammation, involving pain, movement restriction, swelling, warmth, & redness, are seen in the involved joints. In the case that pain is the only symptom, it is difficult to distinguish polyarthritis from the causes of polyarticular joint pain (PJP), such as fibromyalgia or osteoarthritis. Imaging methods such as ultrasonography & magnetic resonance may be helpful in differentiating arthralgia from arthritis.
Polyarthritis can present as acute episodes or it might become chronic, lasting for more than six weeks. Polyarthritis can follow many viral infections. It might evolve into a specific type of autoimmune disease, such as rheumatoid arthritis, lupus, or Sjogren’s syndrome. Nevertheless, usually, it resolves and does not recur.
In some cases, polyarthritis can be severe enough to entail the admission of patients to emergency services, or it can be asymptomatic and might remain undiagnosed for months. Several diseases ranging from rheumatic arthritis to infectious diseases can cause polyarthritis. Anamnesis, physical examination, laboratory findings, & imaging methods are the tools that support an accurate diagnosis. Herein, we goal to underline the differential diagnosis of a patient with polyarthritis and in doing so, contribute to clinical practice.
Polyarthritis isn’t a specific type of arthritis — it’s a diagnosis healthcare provider will give the patient to say you’re experiencing arthritis in many joints at once.
What are the causes of polyarthritis?
Polyarthritis can be caused by several conditions. Some patients with polyarthritis have one type of arthritis that’s present
throughout their body. Other patients have a condition that triggers arthritis in their joints as a symptom or side effect.
Polyarthritis can be either seropositive or seronegative:
Seropositive: This means the patient has antibodies in their blood that may attack their body instead of infections, such as bacteria or viruses, so they might be more likely to develop polyarthritis.
Seronegative: This diagnosis indicates that these particular antibodies are not present in the patient’s blood.
Sometimes, polyarthritis is led by a prior infection or illness, & it can be accompanied by another condition. This parallel
occurrence frequently makes it hard for doctors to diagnose.
Arthritis that spreads to multiple joints If a patient has arthritis, they’re more likely to develop polyarthritis over time. Any type of arthritis can turn into polyarthritis, but the most common ones include:
- Rheumatoid arthritis.
- Psoriatic arthritis.
- Osteoarthritis.
- Gout.
- Calcium pyrophosphate deposition disease (CPPD, or pseudogout).
- Juvenile idiopathic arthritis.
- Autoimmune diseases
An autoimmune disease is the outcome of your immune system accidentally attacking your body instead of protecting it. It’s
unclear why the body’s immune system does this. These attacks can trigger certain types of arthritis or other conditions that lead to it.
Autoimmune diseases that cause polyarthritis include:
- gout
- Lupus.
- Sarcoidosis
- Scleroderma.
- Sjogren’s syndrome
- Rheumatoid arthritis.
- Psoriatic arthritis.
- Infections
Some viral and bacterial infections can trigger polyarthritis. A body’s immune response to the virus or bacteria can be too
strong or catch your joints in the crossfire of fighting the infection & triggering polyarthritis. Some infections that can lead to polyarthritis include:
- Ross River virus
- Viral hepatitis.
- Lyme disease.
- Rheumatic fever.
- Mononucleosis (mono).
- Parvovirus.
- Whipple disease.
- Human immunodeficiency virus (HIV).
Extra-rheumatic causes of polyarthritis
Whether acute or chronic, polyarthritis can have many causes other than rheumatic diseases. These possibilities make the internal medicine perspective even more important in the assessment of patients with polyarthritis.
Infectious diseases various different bacteria, viruses, fungi, & parasites can cause polyarthritis. Infections might lead to polyarthritis over three different mechanisms;
Direct invasion: A microbiological agent straight infects the synovial tissue. This causes monoarthritis but may lead to polyarthritis in rare cases (e.g. Syphilis, leprosy).
Immune-mediated inflammation: Antimicrobial antibodies lead to polyarthritis because of the similarities between microbiological antigens and autoantigens (e.g. ARF, Lyme disease).
Reactive arthritis: Urogenital or gastrointestinal system infections can lead to inflammatory joint diseases like spondyloarthritis, but the microbiological agent is not detected in the synovial fluid.
It is not needed to perform a serological examination for overall potential microbiological agents in every patient with polyarthritis. Nevertheless, as was mentioned above, culture & antibiogram testing or serological examination is performed if the assessment of accompanying symptoms suggests a case of infectious polyarthritis. For this reason, a good rheumatologist requires to know the clinical manifestations of infectious diseases and request an infectious diseases consultation whenever necessary.
Malignancies & polyarthritis Polyarthritis can usually happen concurrently with malignancies as a paraneoplastic syndrome. Tumor antigen-related circulating immune complex-mediated antibodies or cross antibodies are alleged causes for the pathogenesis, nevertheless, the exact pathogenesis stays unknown. Paraneoplastic polyarthritis is more usual in males & peaks between the ages of 50 & 60 years. About one-third of the whole cases had a hematolymphoid malignancy, whereas adenocarcinomas of the lung & breast were the most prevalent solid tumors. This type of arthritis is generally of sudden onset with high levels of inflammatory markers, such as CRP & ESR. Of all patients with paraneoplastic arthritis, only 27.2% are positive for RF & 19.0% are positive for antinuclear antibodies. Less often, anti-CCP antibodies can be positive. It does not need to screen all patients presenting with polyarthritis for malignancy, but more analysis should be performed in the presence of weight loss, lymphadenopathy, etc.
Remitting seronegative symmetrical synovitis with pitting edema is a form of polyarthritis that occurs in the elderly. It is characterized by the symmetrical inclusion of small joints & marked pitting edema on the dorsum of the hands & foot, a sudden inflammatory onset, RF negativity, & an overall excellent prognosis. The prevalence of malignancy is increased in Remitting seronegative symmetrical synovitis with pitting edema, thus, the patients diagnosed with Remitting seronegative symmetrical synovitis with pitting edema need to be evaluated for malignancy.
Drugs & polyarthritis: Polyarthritis patients should be asked in detail about the medications they have been receiving. There has been an increasing amount of data in recent years advocating that immune checkpoint inhibitors targeting PD-1 (nivolumab, pembrolizumab), PD-L1 (durvalumab), & CTLA-4 (ipilimumab, tremelimumab), which have been increasingly become popular in recent years, can cause polyarthritis. There are examination reports that show that antibiotics such as clindamycin, & other medications such as anti-thyroid drugs, can lead to polyarthritis.
What are the symptoms of polyarthritis?
Polyarthritis symptoms tend to be the same as those of rheumatoid arthritis & other autoimmune diseases that affect the joints. They can occur suddenly or over many months.
Signs of joint inflammation:
Signs of joint inflammation typically involve swelling, warmth, pain, & decreased range of motion.
Morning stiffness & pain that improves with activity & worsens with rest are classic symptoms of inflammatory arthritis.
Autoimmune diseases tend to trigger an all-body response because they’re systemic conditions with varying symptoms. Therefore, joint involvement usually does not appear in isolation as it might with osteoarthritis. Instead, there are many other symptoms, like a rash.
Other symptoms include:
- joint pain
- Lack of appetite
- Rash
- Sweating
- swelling or redness in the affected area
- Swollen lymph nodes
- A temperature of 100.4 degrees or above
- Tiredness or a lack of energy
- Unexpected weight loss
In rare cases, the inflammatory disease that causes polyarthritis can also lead to scarring in the lungs, dry eyes, skin rash, & pericarditis is inflammation in the sac surrounding the heart.
Polyarthritis, which is inflammation of multiple joints, is different than polyarthralgia, which is the pain of multiple joints without associated joint inflammation, such as what happens in OA, a wear & tear type of arthritis.
It might be associated with bilateral edema in lower limbs, pain, & joint swelling. Sometimes there is a past history of inflammatory joint issues & bilateral edema of lower limbs.
Alphavirus Polyarthritis Syndrome has an incubation duration of 3–21 days, depending on the specific virus, with either a gradual or sudden onset of fever, arthralgias, headache, lymphadenitis, & conjunctivitis in some forms. A maculopapular rash may present 4–8 days post-symptom onset and might be accompanied by an increase in fever. Joint pains associated with this condition might recur for many months after the initial disease for up to a year.
Inflammatory vs. noninflammatory polyarthritis
Depending on what’s causing the polyarthritis, the healthcare providers will classify it as inflammatory or noninflammatory. Inflammatory polyarthritis causes inflammation in your affected joints. It will make you have symptoms like swelling, discoloration & warmth near your joints. It’s more likely to be led by an autoimmune disease or infection.
Noninflammatory polyarthritis won’t cause swelling in joints. It’s more likely to be led by osteoarthritis or other types of “wear & tear” that happens when the cartilage that cushions joints breaks down over time.
What are the types of polyarthritis?
According to the United States Centres for Disease Control & Prevention (CDC), around 54.4 million adults trusted Source annually were diagnosed with a form of arthritis, fibromyalgia, gout, or lupus between 2013 & 2015.
There are numerous different forms of polyarthritis, including the following:
Polyarticular JIA:
When polyarthritis presents in young people, from an early age to late teens, it is categorized as juvenile idiopathic arthritis or JIA. It can cause very painful swelling in small & large joints from ankles, wrists, and hands to hips and knees. It might even occur in the neck and jaw areas. Doctors do not always know what causes JIA. In many cases, it is a condition that can improve over time & with good treatment.
Lupus:
As well as affecting a person’s joints, this form of polyarthritis often impacts the skin, kidneys, and central nervous system.
Psoriatic arthritis:
Psoriatic arthritis, as its name suggests, can be present in patients who have the skin condition psoriasis. Sometimes, arthritis develops first. Symptoms to look out for can be a scaly, red rash, & the fingers and toes swelling into a “sausage shape” on one side of the body only.
What are the risk factors of polyarthritis?
The risk factors for polyarthritis are of two types: those that can be changed & those that cannot.
Factors that can be changed include:
Lifestyle: Smoking, alcohol consumption, and caffeine intake can make someone more entrusted Source to developing polyarthritis.
Early life experience: If a child is exposed to factors, such as having parents who smoke, it might increase their risk of developing polyarthritis later in life.
Factors that cannot be changed include:
- Age: Patients become more prone to developing polyarthritis as they age. together with degenerative arthritis, autoimmune disease, & gouty arthritis — this will increase with age.
- Gender: The rate of diagnosis of recent cases is more in women than men. Girls have a higher chance than men to develop autoimmune disease, whereas most of those that have gouty arthritis, another form of inflammatory disease, are men.
- Inheritance: Specific genes can make a patient more likely to develop polyarthritis. Some types of inflammatory diseases run in families. Thus, patients will undoubtedly develop the inflammatory disease if their elders or siblings have the disorder.
- Previous Joint Injury – Those that have battle-scarred a joint, maybe while enjoying a sport, are a bit doubtless to eventually develop the inflammatory disease in this joint. Polyarthritis can occur as a result of genetic factors. Some patients naturally have disease-destroying proteins in their bodies called antibodies that make it easier for the condition to thrive.
What are the complications of polyarthritis?
If polyarthritis is not managed or controlled well, other organs & parts of the body can be severely affected. Effects on other involved parts of the body:
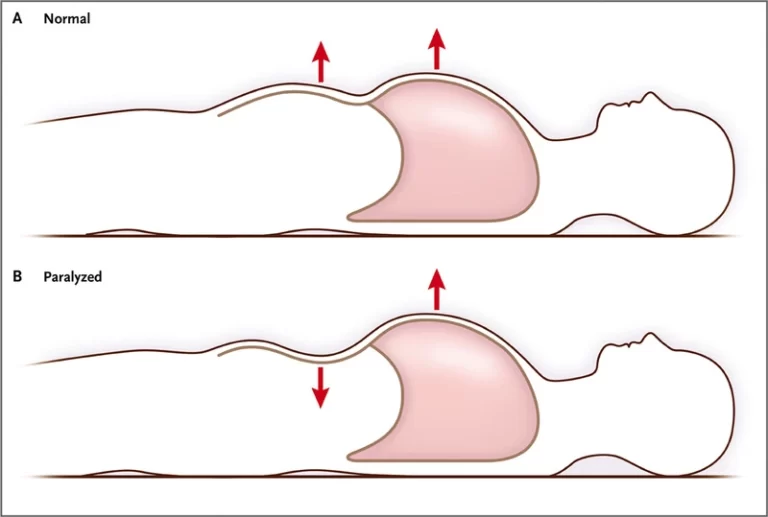
Lungs: Scarring on the lungs can cause complications, such as shortness of breath & a chronic cough.
Eyes: Dry eyes or swelling of the whites of the eyes.
Skin: A rash or lumps of tissue occurring under the skin.
Heart: The lining around the heart can become inflamed, leads chest pain. Heart attacks & strokes might also be more likely.
There is more likelihood of certain conditions occurring if the polyarthritis has been present for a while. These involve carpal tunnel, permanent joint damage, & problems with joints at the top of the spine.
How to prevent polyarthritis?
The patient can lower their chances of developing polyarthritis by:
Avoiding tobacco products.
Doing low-impact, non-weight-bearing exercise.
Following a diet & exercise plan that’s healthy for the patient.
Wearing the proper safety equipment during any physical activity reduces the risk of joint injuries.
What are the associated conditions with polyarthritis?
Polyarthritis is not a specific condition, & people with it may present to their doctor, initially, with something else of concern. For instance, early polyarthritis might cause someone to feel very tired or have flu-like symptoms.
There are some diseases that can accompany polyarthritis or be a sign that there is another problem. These include:
Dupuytren’s contracture: When the connective tissue in the hand contracts to become tighter, any one of the person’s fingers might curl into the palm.
Fibromyalgia: This is a condition that affects the whole body, causing pain & fatigue in numerous areas, including the muscles.
Hemochromatosis: If the body stores too much iron rather than using it, the buildup can cause polyarthritis to develop.
Inflammatory bowel disease: IBD, such as ulcerative colitis & Crohn’s disease, causes inflammation in a person’s small intestine and colon.
Raynaud’s disease: This condition is marked by poor blood circulation in the hands & feet. Fingers can sometimes go white at the distal part, or very red or purple.
What is the diagnostic procedure for polyarthritis?
Physical examination
Physical examination would give support to the diagnosis as per the following basic points:
Classification of polyarthritis In light of information obtained by anamnesis; the classification of polyarthritis is completed by physical examination. Accompanying extra-articular musculoskeletal system inclusion such as enthesitis & tenosynovitis
can be determined as well. It can be said that enthesitis & tenosynovitis are seen more prominently than the SpA group or
seronegative diseases.
Any limitation in the range of motion & detection of specific deformities is critical. For example, irreducible swan neck deformity is always a sign of rheumatoid arthritis. Accompanying findings Detecting the systemic symptoms accompanying polyarthritis during physical examination & evaluating them accurately is important.
Meanwhile, detail about the diseases that might be the extra-rheumatic causes of polyarthritis can be obtained as follows;
Weakness, weight loss, fever Severe polyarthritis might cause weakness & weight loss due to intensive inflammation. In the presence of accompanying weakness & weight loss, systemic rheumatic diseases such as systemic lupus erythematosus and systemic vasculitis, which may possibly involve the visceral organs, should be at the top of the list of differential diagnoses.
Fever might occur along with this inflammation. Only the presence of fever would require often questioning, primarily to rule out infectious diseases, lymphoproliferative diseases, & malignancy. Skin and mucosa Presence of specific skin lesions such as malar rash, vasculitis rash, & psoriasis is important in making the diagnosis. Raynaud’s phenomenon can be found during physical examination. There might be specific cutaneous features the infectious diseases, primarily viral infections. the skin rash in a syphilis patient with polyarthritis. Inspection of the mucosa should be a role of physical examination. For instance, the existence of an ulcer in the oral mucosa of a young female with polyarthritis might support the diagnosis of systemic lupus erythematosus. Genital aphthae that accompany recurrently aphthous lesions might be enough proof to make a diagnosis of Behçet’s Disease.
The eye It is important to find the characteristics of uveitis determined during the ophthalmological examination. While anterior uveitis with SpA group diseases, pan uveitis, or posterior uveitis can be the signs of Behçet’s Disease. Uveitis with granulomatous sign is significant in tuberculosis & sarcoidosis. The infectious cause is likely to be more important if retinitis is determined. It is less likely for episcleritis to accompany a systemic condition, whereas scleritis can be a sign found concurrently with polyarthritis in patients with systemic vasculitis. Dry eye is one of the diagnostic norms of Sjogren’s syndrome and is among the causes of polyarthritis.
Reticuloendothelial system Peripheral lymphadenopathy can be easily found via physical examination. In such cases, the possibility of a lymphoma must be excluded. SLE, ASD, & Sjogren’s syndrome are rheumatic diseases that cause lymphadenopathy. Hepatosplenomegaly can be found in ASD or SLE; nevertheless, it is more likely to be an indicator of lymphoproliferative disorders than lymphadenopathy.
The lungs In a patient with polyarthritis, pulmonary findings can either be in the form of pulmonary inclusion or systemic rheumatic disease, related to infectious disease or related to malignancy. Pulmonary features likely to be seen in rheumatic diseases, such as pleuritis, pleural effusion, lung nodules, interstitial lung disease, airway disease, pulmonary hypertension, & pulmonary hemorrhage, must be examined in detail both in the physical examination & in the anamnesis. Detection of lung nodules might require a histopathological examination to exclude malignancy from the differential diagnosis.
Cardiovascular system ARF can be encountered in adulthood even though it is not a common cause of polyarthritis in this age group. In such a case, a cardiac murmur that is identified on physical examination can be a sign of cardiac valve involvement. Examination of peripheral pulses is important to doubt aortitis. Polyarthritis could be encountered rarely in Takayasu arteritis or in giant-cell arteritis. Infective endocarditis must be contemplated in the differential diagnosis of a polyarthritis case with new-onset fever & cardiac murmur. Syphilis can be the cause of polyarthritis in a patient with advanced-stage aortic insufficiency. Aortic dilatation & related aortic insufficiency may develop in AS. Pericardial effusion and myocarditis, the signs that might accompany rheumatic diseases are found during physical examination.
Gastrointestinal system Dysphagia might be suggestive of scleroderma or polymyositis. Infectious diarrhea is one of the very important causes of reactive arthritis. Peritonitis could be a sign of SLE or FMF. Diarrhea or perianal condition might be advocative of inflammatory bowel disease. Signs of mesenteric ischemia can be associated with systemic vasculitis, particularly in emergency clinics. Abdominal collaterals might be the signs of Budd Chiari syndrome in a patient with Behçet’s Disease.
Urogenital system In a polyarthritis patient with accompanying kidney failure, SLE & systemic vasculitis would be at the top of the list of differential diagnoses. Identification of proteinuria and hematuria, which indicate glomerular involvement, is important. Urogenital infections can be the cause of reactive arthritis. Epididymitis & orchitis, which might be the features of systemic vasculitis can be detected on physical examination.
Nervous system Motor or sensorial loss can occur because of peripheral nerve involvement. Observing a drop foot due to mono neuritis multiplex as the patient walks into the examination room and advocates systemic vasculitis. Signs such as side weakness, increased deep tendon reflex, ataxia, & dysphagia because of central nervous system involvement can be detected on physical examination. Neurological examination, in detail, if required, should be a part of the general rheumatologic examination.
Laboratory findings
Laboratory findings are the third most important component of differential diagnosis after a deep anamnesis & physical examination. Even simple laboratory tests might give clues in making a differential diagnosis.
Complete blood count Cytopenia is a supportive finding for Systemic lupus erythematosus. Nevertheless, polyarthritis can be one of the components of the clinical manifestation of leukemia & lymphoma that causes cytopenia. Lymphocytosis is a valuable feature of chronic lymphoproliferative disorders. Polycythemia & thrombosis raise doubts about myeloproliferative disease as well. The presence of eosinophilia can be a sign of Churg-Strauss vasculitis & hypereosinophilic syndrome with polyarthritis.
Urinalysis A simple urinalysis can be useful for making several differential diagnoses. The presence of pyuria might show polyarthritis reactive to a urinary system infection. The presence of proteinuria & hematuria is quite valuable for SLE and systemic vasculitis, which has the potential to involve glomeruli and might require a renal biopsy to make the diagnosis.
Acute phase reactants (APR) These are the proteins whose serum concentrations increase because of inflammation and tissue injury. C-reactive protein is one of the very usual APRs. Erythrocyte sedimentation rate (ESR) is an indirect method to measure APR & is often used in clinical practice. Serum amyloid A, complement components, alpha-1 antitrypsin, fibrinogen, hepcidin, ferritin, & haptoglobin are the other APRs. Raised APR is not always a sign of rheumatic disease. Infectious diseases & malignancies (rarely) can increase APRs. The inflammation in SLE is not expected to raise CRP, except in some exceptional cases. Although APRs are generally elevated in patients with rheumatic disease-related polyarthritis, they sometimes are within normal limits. Normal APRs do not keep out the diagnosis of polyarthritis or rheumatic disease. Very high ferritin levels might be a supportive sign of ASD, but ferritin is not elevated in a small proportion of ASD patients.
Other biochemical tests of Uric acid should be analyzed in every patient with suspected crystal arthropathy. Uric acid concentration can be normal in a little proportion of patients with gout arthritis or with an acute attack of gout. Liver & kidney function tests should be contemplated in every patient with polyarthritis. Systemic lupus erythematosus & systemic vasculitis patients can present with acute kidney failure. Acute hepatitis or other viral agents can bargain hepatic function tests. Increased lactate dehydrogenase (LDH) is suggestive of autoimmune hemolytic anemia, ASD, myositis, & malignancy. Elevated creatinine kinase should be assessed in every patient with polyarthritis and might be a potential indicator of myositis.
Autoantibodies are crucial in the diagnosis of RA, SLE, other connective tissue diseases, & systemic vasculitis. Rheumatoid factor (RF), anti-CCP antibody, & antinuclear antibody (ANA) should be analyzed in each patient with polyarthritis. Based on accompanying symptoms, an endonuclease antibody (ENA) panel and anti-neutrophil antibody (ANCA) can also be studied. RF might be positive in RA, SLE, or other connective tissue diseases, & in systemic vasculitis. RF might be positive in patients with infectious diseases & malignancies.
It is important to establish anti-CCP positivity to make a diagnosis of rheumatoid arthritis. High-titer positivity has high specificity in diagnosing rheumatoid arthritis. Accurate interpretation of the result of ANA testing is also important, where attention requires to be paid to the titer and pattern. Low-titer ANA positivity can be seen in about 30 percent of healthy females. ANA could also be positive in other autoimmune conditions or malignancies. If ANA is positive, an ENA panel, anti-DNA antibody, & complement testing can be performed. The sensitivity of anti-DNA ranged from 27.7% to 100%, and its specificity ranged from 13% to 89.1%. In a polyarthritis case with negative ANA testing, there is generally no need to study further tests including the ENA panel, anti-DNA antibody, & its complement.
Viral & bacterial serology It is not a routine examination in polyarthritis patients but can be analyzed to support the diagnosis in case of clinical suspicion.
Synovial fluid analysis
Synovial fluid analysis, which is crucial in diagnosing monoarthritis, has a limited role in the differential diagnosis of polyarthritis. Identifying crystals in the synovial fluid of patients with crystal arthropathy is a diagnostic feature. Microscopic examination & synovial fluid culture be require if polyarthritis is caused by the direct invasion of an infectious agent, such as tuberculosis & leprosy.
Radiological methods
Radiography can make a substantial part of the diagnosis of polyarthritis. Hand radiography is important in making a diagnosis of RA & PsA. Erosion & lytic lesions can be diagnostic for rheumatoid arthritis. The presence of sacroiliitis can be demonstrated radiologically by a suprapubic sacroiliac radiograph. Sacroiliac magnetic resonance imaging (MRI) is performed in case of suspected sacroiliitis in spite of the availability of a normal X-ray. Linear calcifications of cartilage identified in the knee radiography can support the diagnosis of pseudogout. No doubt, lung radiography must be used in patients with respiratory system symptoms. Ultrasound, MRI, X-ray, CT, & PET-CT are potential radiological methods of diagnosis.
Ultrasonography (US) can be used to evaluate the severity & make a differential diagnosis of arthritis. Detecting enthesopathy & tendinopathy via the US is significant for SpA. A starry sky image in the joints of patients with crystal arthropathy is useful in making the diagnosis. The use of the US is also a valuable modality in clinical follow-up to monitor treatment efficacy. Temporal artery doppler ultrasonography findings can help with differential diagnosis in case of clinical suspicion.
The contribution of computed tomography (CT) & MRI to the diagnosis of polyarthritis is limited, except for SpA. Nevertheless, they can be utilized for the differential diagnosis of accompanying system involvements. For example, thoracic CT findings are quite important in interstitial lung disease. In addition, if arthritis is suspected, an MRI might be useful in demonstrating synovitis.
PET-CT is used in making a diagnosis in cases with suspected malignancy. Recently, it was understood that PET-CT takes part in the differential diagnosis of big vessel vasculitis. Large vessel vasculitis is a rare etiology of polyarthritis.
Histopathology
Synovial histopathology is infrequently needed in polyarthritis. A polyarthritis case diagnosed with primary amyloidosis by synovial biopsy. Histopathology is rather important for making the differential diagnosis of accompanying features or in assessing visceral organ involvement.
What is the treatment protocol for polyarthritis?
How a patient’s case of polyarthritis is treated depends on a few factors:
What’s causing it? Which type of arthritis does the patient have? How severe your symptoms are?
The patient’s healthcare provider will tell you which treatments you need based on your specific symptoms. Polyarthritis is usually treated with:
Medical treatment of polyarthritis:
Treatment for polyarthritis involves managing symptoms & reducing inflammation. the doctor might recommend the following medications to reduce pain:
Nonsteroidal anti-inflammatory drugs: Commonly referred to as NSAIDs, these drugs decrease inflammation & relieve pain by blocking enzymes and proteins that contribute to inflammation.
Corticosteroids: These drugs decrease inflammation by suppressing the immune response. Corticosteroids are particularly useful if patients have polyarthritis as a result of an autoimmune disease.
Hydroxychloroquine: This is a mild immune modulator drug that reduces swelling and inflammation.
Disease-modifying antirheumatic drugs: compressed as DMARDs, these drugs also suppress the immune system. DMARDs would be utilized to treat rheumatoid arthritis if subsequently diagnosed.
Anti-TNF drugs: These drugs suppress inflammation & would be used if DMARDs alone were not effective in treating pain from rheumatoid arthritis or Still’s disease.
Over-the-counter medications: Topical medications can help relieve symptoms and can be purchased at your local drugstore. These include:
- diclofenac sodium (Voltaren)
- diclofenac (Pennsaud)
- Aspercreme
- Arnica
- capsaicin supplements
Injections: Some patients require injections of corticosteroids or viscosupplementation directly into their joints.
Biological therapies: These slow the progress of polyarthritis. They use the body’s immune system to attack the condition. Common examples of these drugs include infliximab & etanercept.
Steroids: Injections, drips into a vein, or tablets containing steroids can lower inflammation & help control pain. Steroids are only utilized in the short term as side effects can occur with long-term use.
According to the British National Rheumatoid Arthritis Society, a daily 7.5 milligram (mg) dose of a steroid starts taking effect within a few days of starting treatment. A one-off injection of a large dose of 25 mg is known as a pulse.
Arthroplasty: You might need joint replacement surgery. The patient’s healthcare provider or surgeon will tell you what to expect & how long it will take to recover.
At-home Therapies
Warming therapies can temporarily relieve symptoms.
These include:
- Warm baths
- Warming mitts
- Over-the-counter (OTC) topical creams such as Aspercreme
- In addition, don’t underestimate the importance of exercise in managing polyarthritis. Low-impact activities like swimming, yoga, & stretching, can help keep joints healthy.
Physiotherapy treatment of polyarthritis:
Physiotherapists generally perform a physical assessment test before starting the treatment. The assessment majorly includes evaluation of the gait, daily life activities, range of joint motion, muscle strength test, posture, & respiratory function. Afterward, they utilize the arthritis impact measurement scale I & II and the health assessment questionnaire for a precise assessment.
Physiotherapy Modalities in treating Arthritis
This form of treatment approach majorly includes the below-mentioned techniques:
Hot/cold applications-
Hot/Cold therapy is used in both acute & chronic conditions of polyarthritis. Cold packs are usually applied in patients suffering from acute conditions, & hot therapy is applied at the chronic stage of arthritis. Hot packs are generally applied for 10-20 mins once or twice daily. For cold therapy, application modalities are cold packs, ice, nitrogen spray, & cryotherapy.
Electrical Stimulation-
Transcutaneous electrical nerve stimulation (TENS) therapy is the most common form of electrotherapy used to treat arthritis. Studies have reported that patients experience comparatively less pain after receiving TENS therapy once a week for approximately a month.
Hydrotherapy-
Patients get relief from arthritis if hydrotherapy is performed at regular intervals. This technique gives palliative treatment in case of acute and chronic conditions.
Rehabilitation techniques in treating arthritis majorly involve:
- splinting of the affected joints,
- use of compression gloves,
- manual therapy,
- therapeutic exercises,
- strengthening exercises
- patient education.
What is the outlook for polyarthritis?
When it comes to polyarthritis, determining the cause is key to getting proper treatment and reducing symptoms. Diagnosing an infectious cause or autoimmune condition & excluding any possibility of underlying cancer is important, as well. Because this symptom can be the result of a number of causes, it’s important to work with your healthcare professional to understand the underlying cause of your joint pain.
The patient might have acute polyarthritis that only occurs temporarily or while they’re recovering from an infection. If a patient has polyarthritis that lasts for a long time or comes back in the future (recurs) patient has what’s known as chronic polyarthritis.
Since there’s no cure for arthritis, most people require to manage arthritis for the rest of their lives. Your healthcare provider will help you find the right combination of treatments to reduce your symptoms.
FAQ (frequently asked questions)
How common is polyarthritis?
Arthritis is a very common condition. Experts estimate that one-third of adults under 64 have some form of arthritis. Half of the men and people assigned male at birth older than 65 have arthritis. Two-thirds of women & people assigned female at birth older than 65 have it.
It’s hard to estimate how common polyarthritis is because many people don’t know they have it & don’t get it diagnosed. This is especially true because the treatment for one joint with arthritis might help decrease symptoms in other joints that aren’t as painful or stiff.What is the difference between polyarthritis and rheumatoid arthritis?
Polyarthritis means a patient has arthritis in five or more joints at the same time. It’s not a specific disease on its own. It’s a diagnosis that means a patient experiencing arthritis in many joints at once.
Rheumatoid arthritis is a specific type of arthritis. If you have rheumatoid arthritis, the body’s immune system attacks the tissue lining the joints on both sides of the body. It can affect any number of joints, & it’s possible for rheumatoid arthritis to affect enough of your joints to be classified as polyarthritis.What is seronegative polyarthritis?
Seronegative arthritis is a type of rheumatoid arthritis. It’s possible for it to affect five or more joints & become polyarthritis. Talk to your healthcare provider or rheumatologist if you have questions or if you’ve been diagnosed with rheumatoid arthritis & notice new or changing symptoms.