Sarcoidosis
Table of Contents
What is sarcoidosis?
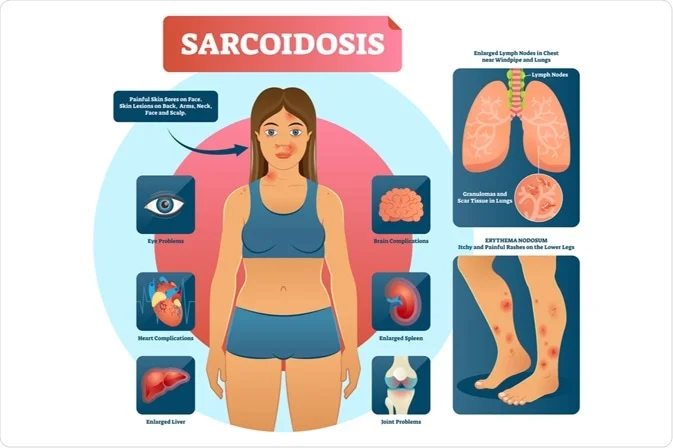
Sarcoidosis is also known as Besnier-Boeck-Schaumann disease. it is a disease involving abnormal collections of inflammatory cells characterized by the growth of tiny collections of inflammatory cells called granulomas in part of your body most commonly the lungs and lymph nodes. Less commonly affected are the liver, heart eyes, and brain. However, any organ can be affected. The signs and symptoms depend on often which organ is involved, no, or only minor, symptoms are seen.
When it affects the lungs, coughing, shortness of breath, wheezing, or chest pain may occur. Some may have Löfgren syndrome with fever, large lymph nodes, arthritis, and a rash known as erythema nodosum.
Sarcoidosis is a rare condition that causes small patches of red and swollen tissue mainly affects young adults worldwide and presents with noncaseating granulomas in various organs. Characteristically it presents with bilateral hilar lymphadenopathy & reticular opacities in the lungs.
The parts of the body commonly affected by sarcoidosis include:
- lymph nodes
- lungs
- eyes
- skin
- liver
- heart
- spleen
- brain
The cause of sarcoidosis is unknown. Some believe it may be because of an immune reaction to a trigger such as an infection or chemicals in those who are genetically predisposed. Population with affected family members are at greater risk.
Diagnosis is partly based on signs & symptoms, which may be supported by biopsy. Appropriate findings include large lymph nodes at the root of both the lungs, high calcium levels in blood with a normal parathyroid hormone level, or elevated levels of angiotensin-converting enzyme in the blood. The diagnosis should only be made after excluding other possible causes with similar symptoms such as tuberculosis.
Sarcoidosis might resolve without any treatment within a few years. Nevertheless, some patients may have long-term or severe diseases. Some symptoms might get improved with the use of anti-inflammatory drugs such as ibuprofen. In some cases where the condition causes serious health problems, steroids such as prednisone are indicated. Medications such as chloroquine, methotrexate, or azathioprine may sometimes be used in an effort to decrease the side effects of steroids.
What are the symptoms of sarcoidosis?
Multiple red-brownish papules and plaques on the left mandibular area of an adult face The growth of inflammatory cells affects the skin.
Sarcoidosis is a systemic inflammatory disease it can affect any organ, although it can be asymptomatic & is discovered by accident in some cases. Common symptoms, which tend to be vague, include fatigue which is unrelieved by sleep, lack of energy, and weight loss, joint aches and pains which is the most common symptom, arthritis, Swelling of the knees, dry eyes, blurry vision, shortness of breath, a dry cough, or skin lesions.
Rarely, people may cough up blood. Sarcoidosis is also accompanied by psychological distress & symptoms of anxiety and depression, which are also associated with fatigue.
The cutaneous symptoms are variable & range from rashes and noduli to erythema nodosum, and granuloma annulare. Sarcoidosis & cancer may mimic each another, making the distinction difficult.
The combination of erythema nodosum, bilateral hilar lymphadenopathy, & joint pain is called Löfgren syndrome, which has a relatively good prognosis. This form of the disease occurs significantly more often in nordic countries patients than in those of other origins.
The granulomas or clumps of cells that characterize sarcoidosis may sometimes be associated with high levels of calcium in the blood and urine. Too much calcium in the urine might cause kidney stones.
seizures, hearing loss, or psychiatric disorders could be observed as part of neurological manifestations. Cardiomyopathy, renal calculi, conduction defects, & enlarged liver are observed in a few cases.
The course of sarcoidosis also varies among individual patients. Usually, patients who experience more generalized symptoms, such as weight loss & fatigue, develop a mild form of the disease. Patients suffering from shortness of breath & skin rashes might develop more chronic, severe sarcoidosis.
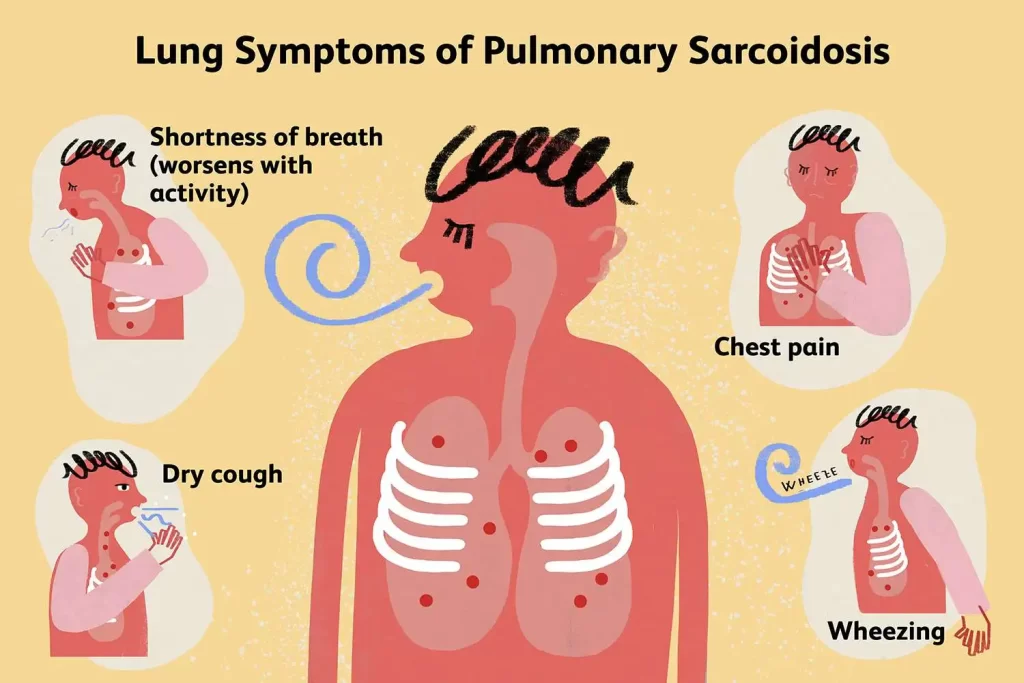
Respiratory symptoms
Affection to the lungs is by far the most common manifestation of sarcoidosis. At least 90% of those patients experience lung involvement. Overall, about half of patients develop permanent pulmonary abnormalities, and some have progressive fibrosis of the lung parenchyma.
Sarcoidosis of the lung is primarily an interstitial lung disease in which the inflammatory process involves the alveoli, small bronchi, & small blood vessels. In acute and subacute stages examination usually reveals dry crackles. At least 5% of cases include pulmonary arterial hypertension. The upper respiratory tract including the larynx, pharynx, and sinuses might be affected.
The stages of pulmonary involvement are based on the radiological stage of the disease, which is helpful in prognosis:
- Stage I: bilateral hilar lymphadenopathy (BHL) alone
- Stage II: BHL with pulmonary infiltrates
- Stage III: pulmonary infiltrates without BHL
- Stage IV: fibrosis
The use of the Scadding grade only provides general information regarding the prognosis of the pulmonary disease over time. it only shows a general relation with physiological markers of the disease & the variation is such that it has limited applicability in individual assessments, including treatment decisions.

Skin symptoms
Sarcoidosis involves the skin and is more common in African Americans than in European Americans. The skin is the second most commonly affected organ after the lungs. The most common lesions are plaques, erythema nodosum, maculopapular eruptions, subcutaneous nodules, and lupus pernio.
There is no requirement for treatment since the lesions usually resolve spontaneously in two-four weeks. Although it may be deforming, cutaneous sarcoidosis rarely causes crucial problems. Sarcoidosis of the scalp presents with patchy or diffuse hair loss.
Heart symptoms
Histologically, sarcoidosis of the heart is an active granulomatous inflammation surrounded by reactive edema. The distribution of affected areas is patchy with localized enlargement of heart muscles. This causes scarring and remodeling of the heart, which leads to dilatation of heart cavities and thinning of heart muscles. As the situation progresses, it leads to aneurysms of the heart chambers.
When the distribution is diffuse, there would be dilatation of both of the ventricles of the heart, causing heart failure & arrhythmia. When the conduction in the intraventricular septum is affected, it will lead to heart block, ventricular tachycardia, & ventricular arrhythmia causing sudden death. However, the involvement of the pericardium and heart valves is uncommon.
The frequency of cardiac involvement varies and is seriously influenced by race involvement. The display of cardiac sarcoidosis can range from asymptomatic conduction abnormalities to fatal ventricular arrhythmia.
Conduction abnormalities are the very common cardiac signs of sarcoidosis in humans and it can include complete heart block. Second to conduction abnormalities, in frequency, are ventricular arrhythmias, which occur in about 23% of cases with cardiac involvement.
Sudden cardiac death, either because of ventricular arrhythmias or complete heart block is a rare complication of cardiac sarcoidosis. Cardiac sarcoidosis can cause fibrosis, granuloma formation, the accumulation of fluid in the interstitium of the heart, or a combination of the former two.
Cardiac sarcoidosis might also cause congestive heart failure when granulomas cause myocardial fibrosis & scarring. Congestive heart failure affects 25-75% of those with cardiac sarcoidosis. Diabetes mellitus and sarcoidosis-related arrhythmias are believed to be strong risk factors for heart failure in sarcoidosis.
A small increased risk of acute myocardial infarction has also been described. Pulmonary arterial hypertension occurs by two mechanisms in cardiac sarcoidosis: reduced left heart function due to granulomas weakening the heart muscle or impaired blood flow.
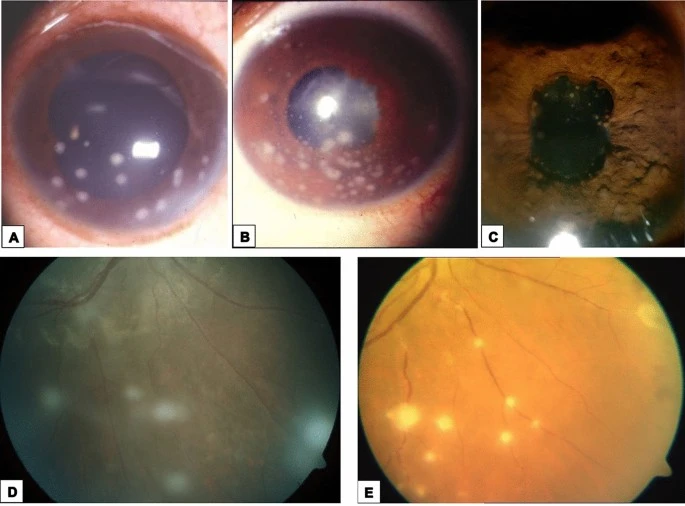
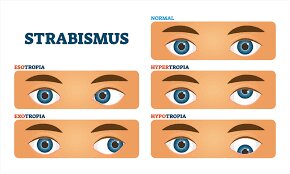
Eye symptoms
Eye involvement signs in the eye include uveitis, and retinal inflammation uveoparotitis, which might result in loss of visual acuity or blindness. The most common ophthalmologic sign of sarcoidosis is uveitis.
The combination of parotitis, anterior uveitis, VIIth cranial nerve paralysis, and fever is called uveoparotid fever or Heerfordt syndrome. Development of scleral nodules associated with sarcoidosis has been observed.
Nervous system
Any of the parts of the nervous system can be involved. Sarcoidosis affecting the nervous system is called neurosarcoidosis. Cranial nerves are most commonly affected, and peripheral facial nerve palsy, often bilateral, is the most common neurological sign of sarcoidosis.
It occurs suddenly and is usually transient. The central nervous system involvement is present in sarcoidosis cases. Other common manifestations of neurosarcoidosis include optic nerve dysfunction, papilledema, palate dysfunction, hearing abnormalities, hypothalamic and pituitary abnormalities, neuroendocrine changes, chronic meningitis, and peripheral neuropathy.
Myelopathy, that is spinal cord involvement, occurs in neurosarcoidosis cases and is often associated with the poorest prognosis of the neurosarcoidosis subtypes. Whereas facial nerve palsies and acute meningitis due to sarcoidosis tend to have the most favorable prognosis, another common finding in sarcoidosis with neurological involvement is autonomic or sensory small-fiber neuropathy. Neuroendocrine sarcoidosis accounts for about 5–10% of neurosarcoidosis cases and can lead to diabetes insipidus, changes in the menstrual cycle, and hypothalamic dysfunction.
The last it can lead to changes in body temperature, mood, and prolactin.
Endocrine and exocrine
Prolactin is frequently increased in sarcoidosis, cases have hyperprolactinemia which frequently leads to amenorrhea, galactorrhea, or nonpuerperal mastitis in women.
It also often causes an increase in 1,25-dihydroxy vitamin D, the active form of vitamin D, which is usually hydroxylated within the kidney, but in patients with sarcoidosis, hydroxylation of vitamin D can take place outside the kidneys, namely inside the immune cells found in the granulomas the condition produces.
1,25-dihydroxy vitamin D is the main cause of hypercalcemia in sarcoidosis and is overproduced by sarcoid granulomata. Gamma interferon produced by activated lymphocytes & macrophages plays a major role in the synthesis of 1 alpha, 25(OH)2D3.
Hypercalciuria is the excessive secretion of calcium in one’s urine and hypercalcemia is an excessively high amount of calcium in the blood seen in individuals and likely results from the increased 1,25-dihydroxy vitamin D production.
Thyroid dysfunction is seen in 4.2% of cases.
Parotid enlargement occurs in about 5% of cases. Bilateral involvement is the rule. The gland is generally not tender, but firm & smooth. Dry mouth can occur; other exocrine glands are rarely affected. The eyes, their glands, or the parotid glands are affected in some cases.
Gastrointestinal and genitourinary
Symptomatic gastrointestinal involvement occurs in less than 1% of cases, & most commonly the stomach is affected, although the small or large intestine may also be affected in a small portion of cases. Studies of the autopsy have revealed GI involvement in less than 10% of people.
These cases would likely act like Crohn’s disease, which is a more commonly intestine-affecting granulomatous disease. About 1% of people have evidence of pancreatic involvement at autopsy.
Kidney involvement Symptomatically occurs in just a few cases, although evidence of kidney involvement at autopsy has been reported in people & occurs exclusively in cases of chronic disease. Symptomatic kidney involvement is usually nephrocalcinosis, although granulomatous interstitial nephritis that presents with reduced creatinine clearance & little proteinuria is a close second Less commonly, the epididymis, testicles, prostate, ovaries, uterus, fallopian tubes, or the vulva may be affected, the latter may cause vulva itchiness.
Involvement of testicular has been reported in about 5% of people in autopsy. Sarcoidosis may lead to infertility in male patients.
Around 70% of people have granulomas in their liver, although only in about 20–30% of cases, liver function test anomalies present this fact are seen. About 5% of patients exhibit hepatomegaly. Only some amount of cases of liver involvement is symptomatic.
Usually, these changes reflect a cholestatic pattern and include raised levels of alkaline phosphatase which is the most common liver function test anomaly seen, while bilirubin & aminotransferases are only mildly elevated. Jaundice is rare.
The symptoms of the reproductive system
Sarcoidosis mainly can affect the male reproductive system, particularly the testes, and it may cause male infertility and erectile dysfunction. The disease rarely involves the female reproductive system.
Sarcoidosis does not increase the incidence of fetal or maternal complications during pregnancy except if it has caused severe impairment of the heart or lungs. However, the disease may worsen after childbirth.
Blood
Abnormal blood tests are frequent, accounting for over half of cases, but are not diagnostic. Lymphopenia is the most common blood abnormality in sarcoidosis. Anemia occurs in about 20% of people with sarcoidosis Leukopenia is less common and occurs in even fewer cases but is rarely severe. Thrombocytopenia and hemolytic anemia are relatively rare.
In the absence of splenomegaly, leukopenia might reflect bone marrow involvement, but the most common mechanism is a redistribution of blood T cells to sites of disease. Other nonspecific findings cover monocytosis, occurring in the majority of sarcoidosis cases, alkaline phosphatase, or increased hepatic enzymes.
People with sarcoidosis frequently have immunologic anomalies like allergies to test antigens such as Candida or purified protein derivatives. Polyclonal hypergammaglobulinemia is also a relatively common immunologic anomaly seen in sarcoidosis.
Lymphadenopathy is swollen glands and it is common in sarcoidosis and occurs in 15% of cases. Intrathoracic nodes are enlarged in 75% of all people; usually, this involves the hilar nodes, but the paratracheal nodes are commonly involved. Peripheral lymphadenopathy is most common, particularly involving the cervical, axillary, epitrochlear, & inguinal nodes. Approximately 75% of cases show microscopic involvement of the spleen, although only in about 5–10% of cases does splenomegaly appear.
What are the symptoms of sarcoidosis when it affects the spleen?
Cytopenias are deficiencies in the amounts of certain blood cells which are the most common “miscellaneous” symptom. The affection of the spleen or bone marrow may lead to anemia and other blood abnormalities.
These conditions generally are not of clinical significance. Bone thinning known as osteopenia is also common in sarcoidosis, as a result of the disease or as a side effect of prednisone therapy.
Some very common conditions seen in those with sarcoidosis are depression and obstructive sleep apnea. Frequently, these are the most significant problems affecting daily life.
Depression may occur in up to 2/3 of patients with sarcoidosis & can cause much of the fatigue that people with sarcoidosis experience. Sleep apnea is suspected in individuals with fatigue, excessive daytime sleepiness, or an unrefreshed feeling of awakening in the morning. Most patients snore, or experience episodes of choking or gasping at night.
Sarcoidosis of the sinuses or nose, weight gain from steroids, and lupus pernio are three factors that increase the chances of obstructive sleep apnea. If the doctor suspects sleep apnea, it may be diagnosed by overnight monitoring in a sleep lab. This sleep test is called a polysomnogram.
What are the symptoms of sarcoidosis when it affects the liver?
Granulomas are present in the liver in 50% to 80% of patients with sarcoidosis. Nevertheless, patients usually do not notice the symptoms due to liver involvement.
Rarely, liver disease can progress to hypertension in the liver also called portal hypertension or cirrhosis; a disease-causing widespread disruption of liver function.
Bone, joints, and muscles
Sarcoidosis can involve the joints, bones, and muscles. This causes a wide variety of musculoskeletal complications that act through different mechanisms.
Arthritic syndromes can be classified as acute or chronic. Sarcoidosis patients with acute arthritis frequently also have bilateral hilar lymphadenopathy and erythema nodosum. These three associated syndromes often occur combine in Löfgren syndrome.
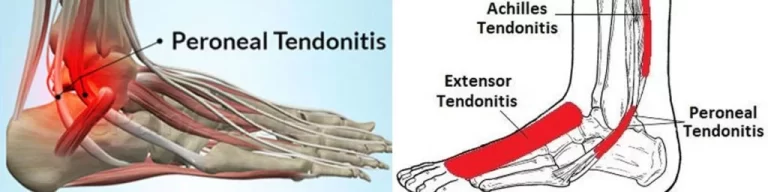
The arthritis symptoms of Löfgren syndrome occur most often in the ankles, followed by the knees, wrists, elbows, and metacarpophalangeal joints. Usually, true arthritis is not present, but instead, periarthritis appears as a swelling in the soft tissue around the joints that can be seen by ultrasonographic methods.
These joint symptoms tend to occur at the same time as erythema nodosum develops. Even when erythema nodosum is absent, it is believed that the combination of hilar lymphadenopathy and ankle periarthritis can be considered a variant of Löfgren syndrome.
Enthesitis also occurs in about one-third of patients with acute sarcoid arthritis, mainly affecting the Achilles tendon and heels. Soft-tissue swelling of the ankles can be prominent, and a biopsy of this soft tissue reveals no granulomas but does show panniculitis similar to erythema nodosum.
Chronic arthritis usually occurs in the setting of more diffuse organ involvement. The ankles, knees, wrists, elbows, and hands might all be affected in the chronic form and often this presents itself in a polyarticular pattern.
Dactylitis similar to that seen in psoriatic arthritis, which is associated with pain, swelling, overlying skin erythema, and underlying bony changes may also occur. Development of Jaccoud arthropathy is very rarely seen.
Bone involvement in sarcoidosis has been reported in 1–13% of cases. The most frequent areas of involvement are the hands and feet, whereas the spine is not commonly affected. around half of the patients with bony lesions experience pain and stiffness, whereas the other half stay asymptomatic. Periostitis is rarely seen in sarcoidosis and has been found to be present in the femoral bone.
Which are the types of sarcoidosis?
Sarcoidosis is classified into a vast range according to the area involved. It can divided into the following types:
- Mucosal sarcoidosis
- Neurosarcoidosis
- Papular sarcoid
- Subcutaneous sarcoidosis
- Ulcerative sarcoidosis
- Annular sarcoidosis
- Erythrodermic sarcoidosis
- Lupus pernio
- Scar sarcoid
- Ichthyosiform sarcoidosis
- Hypopigmented sarcoidosis
- Löfgren syndrome
- Systemic sarcoidosis
- Morpheaform sarcoidosis
What are the causes of sarcoidosis?
The exact cause of sarcoidosis is not known. The current working hypothesis is, that in genetically susceptible individuals, sarcoidosis is caused by an alteration to the immune response after exposure to an environmental, occupational, or infectious agent. Some cases may be acquired by treatment with tumor necrosis factor (TNF) inhibitors like etanercept.
Genetics
The presence of these genetic components and disease in more than one family member is usually related to antigens of the major histocompatibility complex (MHC), especially DR alleles.
The heritability of sarcoidosis varies according to nationality.
Investigations of genetic susceptibility yielded many candidate genes, but only a few were confirmed by further investigations and no reliable genetic markers are known. Recently, the most interesting candidate gene is BTNL2; several HLA-DR risk alleles are also been investigated.
In persistent sarcoidosis, the HLA haplotype HLA-B7-DR15 is either cooperating in the disease, or another gene between these two loci is associated. In nonpersistent disease, a powerful genetic association exists with HLA DR3-DQ2. Cardiac sarcoid has been connected to tumor necrosis factor-alpha variants.
Infectious agents
Various microorganisms like mycobacteria and propionibacteria have been associated with the disease. Possible infective etiology has been described in a few studies where sarcoidosis developed in a previously negative individual after cardiac or bone marrow transplantation, but none of the known relations is specific enough to suggest a direct causative role.
The most implicated infectious agents include mycobacteria, borrelia, fungi, and rickettsia. A meta-analysis investigating the role of mycobacteria in sarcoidosis found it was present in some cases. Still, they also detected a possible publication bias, so the results need further confirmation.
Mycobacterium tuberculosis catalase-peroxidase has been recognized as a possible antigen catalyst of sarcoidosis. The disease has also been reported by transmission through organ transplants.
Autoimmune
Association of autoimmune disorders has been frequently observed. The exact mechanism of this relation is not well familiar, but some evidence supports the hypothesis that this is a consequence of Th1 lymphokine prevalence.
Cytokines including Th1, IL-2, IL6, IL 8, IL12, IL 18, IL 27, and interferon (IFN) gamma & tumor necrosis factor-alpha are closely associated with sarcoidosis.
Some of these are implicated in granuloma formation with macrophage and epithelioid accumulation, activation, and aggregation. Some of these interleukins are believed to act like disease modifiers. Tests of delayed cutaneous hypersensitivity have been utilized to measure progression.
What are the risk factors of sarcoidosis?
Anyone can develop sarcoidosis, but there are factors that might increase your risk including:
Age and sex. Sarcoidosis can occur at any age but frequently occurs between the ages of 20 and 60 years. It is also more common in women than men.
The condition affects people from all ethnic backgrounds. People of African origin and those of Northern European origin have a higher incidence of sarcoidosis. African-Americans are more likely to have involvement in other organs along with the lungs.
Family history. If someone in the family has had sarcoidosis, you’re more prone to develop the disease.
Differential diagnosis of sarcoidosis:
Differential diagnosis includes:
- metastatic disease
- lymphoma
- varicella infection
- septic emboli
- rheumatoid nodules
- granulomatosis with polyangiitis
- tuberculosis
- Atypical infections, such as Mycobacterium avium complex, cytomegalovirus, and cryptococcus.
- Sarcoidosis is confused most commonly with neoplastic diseases, such as lymphoma, and lung cancer or disorders characterized also by a mononuclear cell granulomatous inflammatory process, such as mycobacterial and fungal disorders.
- Cat scratch disease
- Occupational lung disease
What is the diagnostic procedure for sarcoidosis?
Because the symptoms and laboratory results associated with sarcoidosis can occur in other diseases, there is no single test that can diagnose it. nevertheless, the classic sign of the disease is the formation of granulomas; abnormal masses or nodules consisting of related inflamed tissue, in one or more major organs of the body.
granulomas-related sarcoidosis is not different from granulomas that are present in other diseases. As a result, a complete physical examination and medical history – including occupational history, medication history, and environmental exposures, must be made before the conclusion that the illness is, in fact, sarcoidosis.
What are the tests used to diagnose sarcoidosis?
The main tools doctor will use to diagnose sarcoidosis include:
Chest X-rays:
This test provides a picture of the lungs, heart, and surrounding lymph nodes, and shows where infection-fighting white blood cells have formed, which is frequently, the first indication of sarcoidosis.
An X-ray shows how much of the lungs are affected by sarcoidosis. Chest X-ray findings fall into one of the following 5 patterns classified in the chart below. It is important to know that these X-ray patterns do not represent disease stages ( they are not sequential steps in the disease course).
The categories allow doctors to classify the “types of disease.”
Chest X-ray patterns
- 0 = Normal: chest X-ray.
- I = Bilateral hilar lymphadenopathy: the X-ray shows a similar degree of enlargement of lymph nodes at the “root” of both sides of the lungs. It is a usual presentation of sarcoidosis.
- II = Bilateral hilar lymphadenopathy plus pulmonary infiltrations: the X-ray shows a disease process as explained above with expansion into and throughout additional lung tissue.
- III = Pulmonary infiltration only: the X-ray shows a disease process that is spread throughout the lung tissue without enlargement of lymph nodes.
- IV = Pulmonary fibrosis: the X-ray manifests small lung fields, scarring, and retraction of both hila. This type of disease is a very severe or permanent form of the disease.
Bronchoscopy:
Bronchoscopy involves passing a small tube down to the trachea and into the bronchial tubes (airways) of the lungs. The aim of this test is to inspect the bronchial tubes and extract a biopsy to look for granulomas and to rule out infection.
Bronchoscopy is a safe, low-risk, outpatient procedure that provides doctors with a good chance of making an accurate diagnosis. To prepare for this test, the patient will be asked not to eat or drink anything by mouth for 8 hours before the exam. Before the start of the examination, medications will be given to patients to help them relax.
Because these medications can make you dizzy.
The procedure usually lasts 15 to 45 minutes, with a few additional hours for recovery. The doctor may perform a bronchoalveolar lavage, biopsies of the air sacs or airway wall using forceps, or a biopsy of a lymph node
using a needle that is inserted via the bronchoscope. Guidance of the needle with an ultrasound probe connected to the bronchoscope can almost always lead to a diagnosis of sarcoidosis when it is present.
CT scan:
This test is another form of X-ray that provides an even more closure look at the lungs and lymph glands than that is provided by a routine chest X-ray.
This test does not hurt & the simple procedure involves lying on a table for about 10 minutes.
Mediastinoscopy:
This is a surgical procedure that includes a small incision at the base of the neck through which an instrument is travel to biopsy lymph nodes in the chest cavity. This test is performed under general anesthesia in the operating theatre of a hospital and takes 1 to 2 hours.
The requirement for mediastinoscopy to make a diagnosis has gone down dramatically as EBUS-guided biopsies have become widespread.
These tests measure how well the lungs are working; expanding, and exchanging oxygen and carbon dioxide in the blood.
One pulmonary function test uses equipment called a spirometer. This equipment records the changes in airflow as a patient inhales & exhales, as well as the overall volume of air exhaled.
The evolution of granulomas & fibrosis of the lung tissue stiffens the lung tissue and destroys the air sacs, making it more difficult for the lungs to perform these tasks.
Other biopsies:
In addition to the bronchoscopic biopsy or lymph node biopsy, tissue samples can be taken by mediastinoscopy from any other involved site including other lymph nodes, skin, & other sites to determine where granulomas have formed.
Blood tests:
Blood analysis assesses the number and types of blood cells and blood proteins in the body, and how well the cells are working. They also trace increases in calcium levels & abnormal liver function that sometimes accompany sarcoidosis.
One blood test measures a substance called angiotensin-converting enzyme (ACE), which is secreted in huge amounts by cells that make up granulomas.
A newer blood test is sometimes more purposive than ACE which is a measurement of the soluble interleukin 2 receptor levels.
Serum markers of sarcoidosis, include soluble interleukin-2 receptor, serum amyloid A, lysozyme, angiotensin-converting enzyme, & the glycoprotein KL-6. Angiotensin-converting enzyme blood levels are utilized in the monitoring of sarcoidosis.
Bronchoalveolar lavage can show an increased CD4/CD8 T cell ratio, which is indicative of pulmonary sarcoidosis. In at least one study the induced sputum ratio of CD4/CD8 and the level of TNF were correlated to those in the lavage fluid.
A sarcoidosis-like lung disease called granulomatous–lymphocytic interstitial lung disease can be noticed in patients with common variable immunodeficiency and for that reason, serum antibody levels should be measured to exclude CVID.
ACE levels, however, are not always high in sarcoidosis patients, and increased ACE levels can also show up in other illnesses. In a word, there is no specific blood test to diagnose sarcoidosis.
Pulse oximetry:
This test measures the amount of oxygen in the blood by a sensor attached to a patient’s finger. If the oxygen level is reduced the doctor may recommend the use of supplemental oxygen.
Electrocardiogram (EKG or ECG):
This is a routine heart test that checks the electrical activity of the heart. For this test, electrodes with adhesive pads are attached to the skin of the patient’s chest, arms, & legs. The EKG machine creates a picture, on graph paper, of the electrical impulses, that pass through the heart. This screening test helps doctors detect some abnormalities in the heart rhythm.
PET Scan:
In this test, a little amount of radioactive material called F-fluorodeoxyglucose is injected into a vein. This substance collects in the region where the granulomas have collected.
A scanner then determines and records the location and amount of inflammation in the body. This scan will detect inflammation created by diseases other than sarcoidosis so it will be used in combination with another test.
Cardiac magnetic resonance imaging (CMR):
It is one of the tests for diagnosing cardiac sarcoidosis. It has 78% specificity in diagnosing cardiac sarcoidosis. Its T2-weighted imaging can detect acute inflammation.
Meanwhile, late gadolinium contrast (LGE) can detect fibrosis or scarring. Lesions at the subpericardium and mid-wall enhancement of the basal septum or inferolateral wall are strongly suggestive of sarcoidosis.
MRI:
It can also follow up on the treatment efficacy of corticosteroids and the prognosis of cardiac sarcoidosis.
Gallium scanning:
The radioactive chemical gallium-67 is injected into a vein in this procedure. The gallium collects in inflamed body tissue. A scan of the body then indicates which tissues & amount of how much tissue is affected.
The scan will disclose any type of inflammation occurring in the body, nevertheless, does not necessarily mean the patient has sarcoidosis. Because of this test’s limitations, it is not performed generally.
Purified protein derivative:
This is a type of skin test that is used to help establish earlier exposure or infection with tuberculosis.
Since tuberculosis is sometimes confused with sarcoidosis, this simple test is often performed. In sarcoidosis, this skin test is generally negative or non-reactive.
Slit-lamp examination:
This examination sees the inside of the eye and is utilized to detect eye-related problems caused by sarcoidosis.
What are the complications of sarcoidosis?
Most patients who receive a diagnosis of sarcoidosis do not experience complications. Nevertheless, sarcoidosis can become a chronic or long-term, condition. Other potential complications might include:
- Lungs- Untreated pulmonary sarcoidosis can lead to permanent scarring in your lungs (pulmonary fibrosis), making it difficult to breathe and sometimes causing pulmonary hypertension and can even cause lung infection
- Eyes- Inflammation can affect almost any part of the eye and may cause damage to the retina, which can eventually cause blindness. Rarely, sarcoidosis also can cause cataracts, which are characterized by clouding of the lens in your eye, and glaucoma, which is a group of eye diseases that can cause blindness.
- Kidneys- Sarcoidosis can affect how the body handles calcium, which can lead to kidney stones and reduce kidney function. In rare cases, this can leads to kidney failure.
- Heart.-Cardiac sarcoidosis results in granulomas in the heart that can disrupt heart rhythm, blood flow, and normal heart function. Rarely, this might lead to death.
- Nervous system- A small number of patients with sarcoidosis develop problems related to the central nervous system when granulomas form in the brain and the spinal cord. for example, Inflammation in the facial nerves can cause facial paralysis.
- infertility in men or difficulty conceiving because of sarcoidosis affecting the testes.
- In rare instances, sarcoidosis causes severe heart and lung damage. If this occurs, the patient may need immunosuppressive medications.
What is the treatment plan for sarcoidosis?
Medical treatment for sarcoidosis:
Treatment for sarcoidosis varies greatly depending on the patient’s condition. At least half of the patients do not require systemic therapy.
Most patients only require symptomatic treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin. For those presenting with lung symptoms, except the respiratory impairment is devastating, active pulmonary sarcoidosis is observed usually without therapy for two to three months; if the inflammation does not subside spontaneously, therapy is begun.
Major categories of drug interventions include antimetabolites, glucocorticoids, and biologic agents especially monoclonal anti-tumor necrosis factor antibodies.
Investigational treatments include specific antibiotic combinations & mesenchymal stem cells. If drug intervention is indicated, a step-wise approach is frequently used to explore alternatives in order of increasing side effects and monitor potentially toxic effects.
Corticosteroids
Most commonly prednisolone has been the standard treatment for many years. In some patients, this treatment can slow or reverse the course of the disease, but other patients even do not respond to steroid therapy. The use of corticosteroids in mild disease is disputed because in many cases the disease is set aside spontaneously.
Antimetabolites
Antimetabolites, also categorized as steroid-sparing agents, such as methotrexate, azathioprine, mycophenolic acid, and leflunomide are often used as alternatives to corticosteroids.
Of these, methotrexate is the most widely used drug. Methotrexate is considered a first-line treatment in neurosarcoidosis, frequently in conjunction with corticosteroids. Long-term treatment with methotrexate is associated with liver damage in about 10% of patients and hence may be a significant concern
In patients with liver involvement and requires regular liver function test monitoring. Methotrexate can also lead to pulmonary toxicity, although this is fairly not common and more commonly it can confound the leukopenia caused by sarcoidosis. Due to these safety concerns, it is frequently recommended that methotrexate is combined with folic acid in order to prevent toxicity.
Treatment of Azathioprine can also lead to liver damage. Nevertheless, the risk of infection appears to be about half lower in those treated with methotrexate instead of azathioprine.
Leflunomide is being used as a replacement for methotrexate, possibly due to its apparently lower rate of pulmonary toxicity. Mycophenolic acid has been used successfully in uveal sarcoidosis, neurosarcoidosis, and pulmonary sarcoidosis.
Immunosuppressants
As the granulomas are caused via collections of immune system cells, particularly T cells, there has been some success using immunosuppressants like cyclophosphamide, chlorambucil, and cyclosporine, immunomodulatory as pentoxifylline and thalidomide, and anti-tumor necrosis factor treatment such as infliximab, golimumab, etanercept, & adalimumab.
Cyclophosphamide and chlorambucil are rarely used in the treatment of sarcoidosis due to their high degree of toxicity, especially their potential for causing cancers.
Infliximab has been utilized successfully to treat pulmonary sarcoidosis in a number of cases. Etanercept, on the other hand, has failed to demonstrate any significant efficacy in people with uveal sarcoidosis.
Likewise, golimumab has failed to show any effectiveness in those with pulmonary sarcoidosis.
Adalimumab treatment response is similar to that seen with infliximab, but as adalimumab has a better tolerability profile it might be preferred over infliximab.
Specific organ treatments
Ursodeoxycholic acid has been utilized successfully as a treatment for conditions with liver involvement.
Thalidomide has also been tried successfully as a treatment for treatment-resistant lupus pernio in trials, which might stem from its anti-TNF activity, although it failed to show any efficacy in pulmonary sarcoidosis.
The cutaneous condition may be successfully controlled with antimalarials such as chloroquine and hydroxychloroquine and the tetracycline antibiotic, minocycline. Antimalarials have also demonstrated efficacy in treating sarcoidosis-induced hypercalcemia & neurosarcoidosis. Long-term use of antimalarials is limited, nevertheless, by their potential to cause irreversible blindness & hence the need for regular ophthalmologic screening.
This toxicity is usually less of a problem with hydroxychloroquine than with chloroquine, although hydroxychloroquine can disturb glucose homeostasis.
Recently selective phosphodiesterase 4 (PDE4) inhibitors like roflumilast, apremilast, and the less subtype-selective PDE4 inhibitor, pentoxifylline, have been used as a treatment for sarcoidosis, with successful results being obtained with apremilast in cutaneous sarcoidosis. Pentoxifylline has been utilized successfully to treat acute disease although its use is greatly limited by its gastrointestinal toxicity mostly vomiting, and diarrhea.
ACE inhibitors have been reported to cause an excuse in cutaneous sarcoidosis and improvement in pulmonary sarcoidosis, including improvement in pulmonary function, remodeling of the lung parenchyma, and prevention of pulmonary fibrosis in separate cases.
Nicotine patches have been found to possess anti-inflammatory effects in sarcoidosis patients, although whether they had disease-modifying effects requires more investigation.
Antimycobacterial treatment has also proven itself effective in treating chronic cutaneous sarcoidosis. Quercetin has also been used as a treatment for pulmonary sarcoidosis.
Because of its not common nature, the treatment of male reproductive tract sarcoidosis is disputed. Since the differential diagnosis includes testicular cancer, some suggested orchiectomy, even if evidence of sarcoidosis in other organs is present. In the newer approach, testicular, epididymal biopsy, and resection of the largest lesion have been proposed.
Neurostimulants such as methylphenidate and modafinil have shown some effectiveness as an adjunct for the treatment of sarcoidosis fatigue.
Treatments for symptomatic neuropathic pain in sarcoidosis patients are similar to that for other causes and include antidepressants, anticonvulsants, and prolonged-release opioids, however, only 30 to 60% of patients experience limited pain relief.
Patients with severe or advanced lung sarcoidosis may need oxygen therapy. Sarcoidosis is frequently treated with the help of a multidisciplinary team of healthcare professionals. Because the disease can affect so many organ systems, patients may look out for the condition with healthcare providers who specialize in the treatment of the lungs, heart, brain, kidneys, liver, eyes, and skin. At specialized medical centers, these healthcare providers work as a team to develop a comprehensive treatment plan to control the symptoms and protect the patient’s overall health.
Surgical treatment for sarcoidosis:
Sarcoidosis frequently responds to treatment or may resolve without treatment, surgery is rare. Nevertheless, severe and extensive damage to organs like the lungs, heart, or kidneys could require an organ transplant.
Lung transplant surgery
Lung transplantation is reserved for treating patients with very severe lung damage resulting from sarcoidosis. An organ transplant includes removing a damaged organ, such as a lung, and replacing it with a healthy organ from a deceased donor. Organ transplants can significantly improve quality of life but involve many risks, including the risk of infection and even death if the body does not accept the transplanted organ.
Lung damage & scarring are common complications of sarcoidosis, occurring in 20 to 30 percent of all cases. If this damage is extensive, a lung transplant may be required.
One or both lungs can be replaced in a procedure an invasive chest surgery. Depending on its nature, the surgery takes from 4 to 12 hours and requires an extended hospital stay for recovery.
Heart surgery
If the heart is severely affected by sarcoidosis, a heart transplant might be performed. A pacemaker may also be implanted in a patient to help regulate heart function.
The pacemaker is inserted into the chest,& a needle is used to thread the wires into the correct placements in the heart. The surgery can take several hours, but typically only involves an overnight hospital stay, where the heart’s function is monitored.
Kidney transplant surgery
For kidney abnormalities associated with sarcoidosis, transplantation of the kidney may be considered. This surgery usually takes around 3 hours & replaces a damaged kidney with one from a donor or from a matched but deceased person. Recovering from surgery requires a hospital stay of at least a few days.
Risks associated with surgery
Surgery for sarcoidosis is considered to be a treatment option of last resort and carries risks. Nevertheless, if necessary & successful, it could lengthen lifespan and improve quality of life.
As in all surgeries, there is a risk of lingering pain & infection at the site of the surgery. Organ damage from surgery, especially in the chest, is possible, as are complications because of blood clotting and fluid buildup. These may require additional surgeries to fix it.
Organ transplantation, in particular, includes risks of rejection. Patients need to take immunosuppressant medications for the rest of their life to prohibit rejection. Although immunosuppressants might have the added benefit of reducing the progression of sarcoidosis itself, they also increase a patient’s vulnerability to infection and sickness.
The general anesthesia used during surgery involves a risk of an allergic reaction. Since sarcoidosis can affect multiple organs, including the liver and kidneys, different drugs with different dosages may need to be considered.
Managing sarcoidosis:
Managing sarcoidosis includes monitoring symptoms closely to track the effectiveness of treatments. Medical treatment can be utilized to control symptoms, restrict complications and improve outcomes in patients with persistent sarcoidosis. If a patient has sarcoidosis, the healthcare provider will carefully monitor her to see if the sarcoidosis is getting better or worse and will adapt the treatment depending on how the body is doing.
If sarcoidosis goes into remission, meaning you no longer have any symptoms, the doctor may choose to slowly stop medications. Most relapses, also known as flares or recurrences, occur in the first 6 months after medication has been stopped, so it is important to monitor health closely. The longer patient goes without symptoms, the less likely it is that you will relapse.
An important part of managing disease will be finding emotional support. Many patients being treated for sarcoidosis feel anxious because symptoms interfere with their daily routine. Depression & anxiety are common. Tell the doctor if the patient has these feelings as a treatment for anxiety and depression may make your sarcoidosis treatment more effective. It can also be helpful to find a community or support group of other patients with sarcoidosis.
Physical therapy treatment for sarcoidosis:
Structured physical activity programs can improve exercise capacity, muscle strength, & fatigue in sarcoidosis. Additionally, physical training regimens appear to improve general physical and psychological well-being, suggesting a role in the treatment of sarcoidosis. Pulmonary rehabilitation & training have been incorporated into expert consensus recommendations
Physical therapy treatment is based on the symptoms that the individual appears with. Acute sarcoidosis often times regresses spontaneously. Nevertheless, more chronic stages of sarcoidosis require treatment based on the affected systems.
In most cases with pulmonary involvement, physical therapy can be helpful by increasing ventilation through strategies that may include breathing exercises, strength training, and endurance exercises.
The result of these treatments may be variable but are designed to allow the patient a more normal life by decreasing dyspnea, increasing endurance, and decreasing fatigue. Both upper and lower extremity exercises can be used along with breathing exercises for optimal treatment outcomes.
What is the prognosis of sarcoidosis?
Gross pathology image showing sarcoidosis with honeycombing appearance: Prominent honeycombing is present in the lower lobes accompanied by fibrosis and some honeycombing in the upper lungs. Honeycombing is made up of cystically dilated airways separated by scar tissue resembling the honeycomb of bees. It is a nonspecific end stage of many kinds of interstitial lung disease.
Asymptomatic patients do not need treatment and often remain stable for many years. nevertheless, those who develop symptomatic lung or extrapulmonary disease tend to have a guarded prognosis.
The disease can be set aside spontaneously or become chronic, with exacerbations and remissions. In some cases, it can develop into pulmonary fibrosis and death. In benign cases, remission could occur in 24 to 36 months without even treatment but regular follow-ups are needed.
Some cases, however, may persist for several decades. Two-thirds of people with the condition achieve remission within 10 years of the diagnosis. When the heart is involved. The risk for premature death was markedly increased compared to the general population for a smaller group of cases with severe disease at diagnosis.
Serious infections, occasionally multiple during the course of the disease, & heart failure might contribute to the higher risk of early death in some patients with sarcoidosis.
In many patients with sarcoidosis, medical treatment is required, and the disorder spontaneously resolves. Nevertheless, in a certain number of patients, the disease may take a fulminant course with severe symptoms. Factors that indicate a poor prognosis involve significant chest imaging findings, extrapulmonary involvement, & the presence of pulmonary hypertension.
Many studies indicate that a chest x-ray is a very good marker for disease prognosis. In severe cases, patients may need oxygen, and experience heart block & respiratory failure. Data related to mortality are not available because, in many cases, long-term follow-up is missing. Overall, it shows that about one-fifth of patients develop functional impairment, and there is a mortality rate of 3 to 5% in patients who are not treated. The highest mortality rates are in African American females past the fifth decade of their life.
FAQ (frequently asked questions)
Is sarcoidosis an autoimmune disease?
Some scientists believe sarcoidosis is an autoimmune disease. They think it is the result of the body mistakenly attacking itself contrary to foreign bodies like viruses or bacteria.
It frequently overlaps with other known autoimmune diseases like rheumatoid arthritis & autoimmune thyroid disease.
Nevertheless, it also appears factors like genetics and environmental exposures might play a role. So no single cause Trusted Source has been identified.What is the life expectancy for someone with sarcoidosis?
Patients with asymptomatic sarcoidosis do not usually require treatment. In fact, many will remain stable for years without progressing symptoms.
Those who do develop advanced symptoms or complications frequently have a favorable outlook. Overall, the mortality rate in the untreated patient is 5 percent trusted Source.
But the long-term outlook for untreated patients can be difficult. Respiratory failure from severe scarring is possible, & it can lead to death.Is sarcoidosis a serious illness?
For a few patients, sarcoidosis is a chronic condition. In some patients, the disease might result in the deterioration of the affected organ. Rarely, sarcoidosis can be fatal. Death usually is the result of complications with the lungs, heart, or brain.




5 Comments