Cervical spine mobilization techniques
Table of Contents
What is Mobilization for the Cervical spine ??
- Cervical spine mobilization is a passive, skilled, manual therapy maneuver applied to joints and related to the soft tissue at various speeds and amplitudes taking physiological or accessory movement for therapeutic purposes
- small volume potency applies at a fast velocity, and a large volume force applies at to slow velocity
- it is a manual method that consists of applying the target forces on a painful, stiff, or otherwise neglected joint in addition to upgrading its overall function. Which is not appropriate in all conditions, joint mobilizations/manipulation help improve the range of motion, reduce pain, and reduce stiffness.
- Cervical spine mobilization is a manual therapist’s hand treatment that is repeatedly executed by physical therapists and healthcare professionals who master rehabilitation for locomotion disorders and chiropractors, health professionals treating disorders of the musculoskeletal system that contain bones, muscles, soft tissue, ligaments, etc.
Introduction to the cervical spine
- A healthy spine has three natural curves that initiate an S-shape. These curves soak up shocks to your body and protect your spine from injury. Many different parts create the spine:
- Vertebrae: The spine has 33 irregular vertebrae small bones that form the spinal canal. The spinal canal is a tunnel that houses the spinal cord and nerves, defending them from injury. Most vertebrae locomote to grant a range of motion.
- Facet joints: These spinal joints have cartilage a greasy connective tissue that allows the vertebrae to slide in opposition to each other. Facet joints allow you to twist and turn, giving flexibility and stability. facet joints can establish arthritis and cause back pain or neck pain.
- Intervertebral disc: These flat, round cushions lie in the middle of the vertebrae and act as the spine’s shock absorbers. Each disk has a soft, gel-like center the nucleus pulposus confined by a flexible outer ring the annulus fibrosus. Intervertebral disks are under constant pressure. A herniated disk can crack, permitting some of the nucleus’s gel substance to expose. Herniated disks also called bulging, slipped, or ruptured disks can be terrible.
- Spinal cord and nerves: The spinal cord is a column of nerves that passes through the spinal canal. The line extends from the skull to the lower back. Thirty-one pairs of nerves branch out over the vertebral beginning in the neural foramen. These nerves take out messages in the middle of the brain and muscles.
- Soft tissues: Ligaments attach to the vertebrae to hold the spine in position. Muscles support the back and help you to move in forward and backward. Tendons affix muscles to bones and aid movement.
What are the spine segments?
- The 33 vertebrae compose five specific spine segments. Starting at the neck and/or going down toward the buttock’s rear end, these segments contain
- cervical spine
- thoracic spine
- lumber spine
- sacrum
- coccyx
Cervical spine
- Cervical spine (neck): The top part of the spine has 7 vertebrae C1 to C7. These neck/cervical vertebrae permit you to turn, twist, tilt, and nod movement of your head. The cervical spine creates an inward C-shape termed a lordotic curve.
ligaments of the cervical spine
- The ligaments are strong fibrous bands that clasp the vertebrae together, stabilize the spine and shelter the discs. The 3 major ligaments of the spine are the ligamentum flavum, anterior longitudinal ligament, and posterior longitudinal ligament The Anterior longitudinal ligament and posterior longitudinal ligament are steady strap-like shapes that run from the top of cervical vertebrae to the bottom of the spinal column along with the vertebral bodies. They inhibit excessive movement of the vertebral bones. The ligamentum flavum associates the lamina of each vertebra.
Anterior longitudinal ligament
- A strong strap like a band of variable thickness and width overlays the anterior aspects of the vertebral bodies and intervertebral discs all over the length of the vertebral column. in distinction to superficial to deep its ligamentous fibers run varying lengths:
- the nethermost fibers are short intersegmental fibers
- the intermediate fibers associate 2 to 3 vertebrae
- the superficial fibers associate 3 to a vertebrae
- It is thick, till narrow, along with the vertebral bodies where it is loosely bound to the periosteum. At the levels of the intervertebral disc, it broadens and the fibers strongly affix to the fibrocartilage disc, the hyaline cartilage vertebral end plates, and the edge of the vertebra
- A primary spine stabilizer around one inch broad, the Anterior longitudinal ligament runs the entire length of the spine in distinction to the base of the skull, via the cervical, thoracic, and lumbar spine to the sacrum. It associates the front side anterior of the vertebral body with the front of the annulus fibrosis.
- It’s affixed to the upper and lower margins of the particular vertebral body.
- reduce the extension of the vertebral column and emphasizes the intervertebral disc.
- the area on the anterior surface of the vertebral bodies of the vertebral column.
amination
- The anterior longitudinal ligament is aminated by recurrent branches of rami communicates.
posterior longitudinal ligament
- The posterior longitudinal ligament is one of the most important ligaments that contribute to stability in the spine. It passes along with the posterior aspect of the vertebral body inside the vertebral canal from the body of the axis to the sacrum. The posterior ligament is serene of longitudinal fibers that are opaquer than the anterior longitudinal ligament. However, like the anterior longitudinal ligament, the blurred fibers are deeper and connect to one vertebra while the superficial fibers attach to three to four vertebrae. The superficial layer is an extension of the tectorial membrane at the axis of the posterior longitudinal ligament, and the deep layer is an origination of the cruciform ligament at the Atlas.
- The fibers are thick at the intervertebral spaces and are more devotee to the annulus fibrosus of the intervertebral discs than at the vertebral body where fibers are thinner. This aberration is more observable in the posterior ligament rather than in the anterior. Therefore, the posterior longitudinal ligament is much more elegant than the anterior longitudinal ligament, which is compelling for the disc herniation occurring posterolateral.
- The Posterior longitudinal ligament consists of superficial and deep connective tissue layers, The superficial layer is the more posterior side, with its extension from the dura mater often being difficult to determine. It consists of a central band of fibers 8 to 10 mm wide expanding over a lot of vertebral segments. Due to its vast association with the intervertebral disc, it has been termed as being ‘‘feeble’’, permitting a craggy appearance over each vertebral body. This craggy appearance converts more probable in the lower thoracic and lumbar areas, where the superficial layer is of more decent width.
- semantic variation even without the lumbar region, where both the central fibers and the ‘‘fanlike’’ portion tend to decelerate in width in the middle of L1 and L5 vertebrae. The deep layer, which is a devotee to the superficial layer in the midline, is of more decent diameter all over its length, being 2 to 3 mm broad at its narrowest point. It also has a craggy appearance.
- In the cervical area, the Posterior longitudinal ligament is a broad band-like structure of equal width beyond both the intervertebral disc and vertebral body, however more inferiorly, it makes increasingly craggy, with its vastest part being beyond the intervertebral disc The division fibers of the superficial and deep layers were difficult to identify at the level of the intervertebral disc, but their affixation to the edges of the vertebral bodies and intervening annulus fibrosus was clear.
- The fibers of each and every layer arose to consolidate, forming a standard connection. Both superficial and deep layers are affixed to a midline bony septum on the posterior surface of the vertebral body in the middle of the superior and inferior edges. This connection was only sometimes expanded because of deficiencies in the septum in the central 3rd of the vertebral body. The adaptation of fibers within the posterior longitudinal ligament was persistent at all levels, with the fiber in the central portion of the superficial layer being more vertical than those of the ‘‘fanlike’’ part. even if the deep layer was observable through the superficial layer
- The posterior longitudinal ligament has a more opposing than supportive role. The observed pattern of movement of opposing materials like masses and bony fragments following a vertebral fracture into the vertebral canal integrates that the Posterior longitudinal ligament acts as a protector for the spinal cord and from displaced disc material.
- Fibers of the superficial layer will limit the forward flexion, while the oblique fibers of the deep layer will limit the lateral flexion and rotation. fibers from both layers consist of all movements, with an elevating number of fibers enrolled with elevating pressure. The craggy appearance of the Posterior longitudinal ligament in the lower thoracic and lumbar area may be due to the elevated rotational and lateral flexion forces brought out in the lower area compared with the upper area of the vertebral column of the spine. The presence of elastin protein in the Posterior longitudinal ligament assists that it has a role in the dynamic movement of the spine. Observed patterns of disc fragment migration following vertebral burst fractures suggest that the Posterior longitudinal ligament also preserves the contents of the vertebral canal.
blood supply of the posterior longitudinal ligament
- The prime supply of blood to the spinal cord is in distinction to a single anterior spinal artery and the two posterior spinal arteries. These two posterior spinal arteries are the branches of the vertebral artery in the spine. Posterior arteries convey the blood to the posterior part of the spinal cord, and the anterior portion achieves blood supply from the anterior spinal artery. adjoining to the spinal arteries, there are other arteries also available at each spinal segment called radicular spinal arteries, which come from the body wall arteries. The small penetrating arteries radiate off by both anterior and posterior spinal arteries that hammers interrelate in the spinal cord.
- The radicular spinal arteries supply the blood to the anterior and posterior parts of the spinal cord. The drainage of blood from the spinal cord snatches the place with the aid of anterior and posterior spinal veins. The anterior and posterior spinal veins duct into the internal and external venous plexus. Through the venous plexus, the blood duct into the main venous system with the help of azygos veins, lumbar veins, and hemizygous veins
nerve supply of the posterior longitudinal ligament
- The primary source of the nerve supply of the posterior longitudinal ligament is the meningeal branch rented from the spinal nerve. It concords ascending and descending branches in the vertebral column of the spine. There are transverse roots hammered by the synthesis of ascending and descending roots. The synthesis of the transverse branches from the reverse side generates a network of nerve fibers superficially, which animates the posterior longitudinal ligament in the vertebral segment of the spine. The posterior part of the annulus fibrosus is diverse by the nerve fibers hammering a network deep in the intervertebral part of the posterior longitudinal ligament
- There is no animation of the deep layer of the nucleus pulposus or/and annulus fibrosus because of the shortcoming nerve fibers and nerve boundary. some nerve boundaries are present in the middle part of the nucleus pulposus, but in the peripheral zone, there are heavy nerve fibers. The heavy nerve fibers in the peripheral zone perform a needed part in the regulation of movement and posture in the vertebral column of the spine.
muscle attachment of the posterior longitudinal ligament
- There are 3 groups of muscle in the back of the spine; superficial, intermediate, and deep muscle layers. The superficial layer consists of two muscles the splenius cervicis and splenius capitis. They perform the needed part in the extension of the neck and the movement of the shoulder.
- The intermediate muscle group consists of the longissimus, iliocostalis, and/or spinalis muscles. longissimus, iliocostalis, and spinalis muscles of the intermediate group have the same tendinous arises. The intermediate groups of muscles assist in the flexion of the head and the upper vertebral column and the movement of the thoracic cage. The deep layer consists of the semispinalis, rotatores, and multifidus. The major function superficial intermediate and deep muscle group is the stabilize the vertebral column and maintain an upright posture. They also assist in balance and proprioception
variants
- the posterior longitudinal ligament is smaller and sluggish. It has an oval shape that alters from 2 to 2.25 mm in thickness at the level of L5-S1. From the L5 vertebrae upwards, the ligament hammers a narrow band, which broadens symmetrically at the level of each disc. The fibers of the annulus fibrosus and the edge of the vertebral body are the sites of association of the ligament, but in some cases, not all, it is associated with the posterior aspect of the vertebra.
- The posterior longitudinal ligament tends to be most established at the level of the L3 and L4 vertebra, where its average thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker middle portion almost about 2.5-4 mm thickness all over the whole length of the ligament. The ligament in the central portion of every vertebral body envelops the vascular foramina
interspinous ligament
- This ligament is assured of thin sheets affixing the spinous processes from roots to apexes from C1 to S1 one segment at a time. Anteriorly, Its fibers affix with ligamentum flavum, along with posteriorly its fibers affix with the supraspinous ligament. The ligaments are small and elongated in the thoracic area, broader, thicker, and quadrilateral in a form in the lumbar area, and only slightly clear in the neck. In the neck, they are normally contemplated part of the nuchal ligament.
- The interspinous ligaments are thin and short structures that affix adjoining spinous processes. The Interspinous ligament is well vascularized and consists of sensory nerves, particularly on their posterior and lateral surfaces. These ligaments arise somewhat from the ligament Flava, somewhat from the reciprocal vertebral laminae, and somewhat from the caudal aspect of the spinous process. The lumbar Interspinous ligament is somewhat thicker and tends to be more sparkler and quadrilateral in nature and generally happens in pairs. The lumbar Interspinous ligament is usually blocked out with a fiber location passing obliquely or/and horizontally in an anterior-posterior direction from the superior edge of the caudal spinous process to the cranial spinous process.
- The Interspinous ligament is part of the posterior ligamental complex, and they act as stabilizers of the spine and assist to limit spine flexion.
nerve supply
- The lumbar interspinous ligaments receive a nerve supply from the medial branches of the lumbar dorsal rami and experimental stimulation of the interspinous ligament gives low back pain and referred pain in the lower limbs. This distributes the interspinous ligament as an alluring source of low back aches.
blood supply
- The interspinous ligament is well supplied by small blood vessels and sensory nerves, the latter especially in its posterior part and on its lateral surfaces.
- movements: The role of the interspinous ligament is to limit flexion bending forwards by restricting the separation of the spinous processes of the vertebral column.
ligamentum flavum
- The ligamentum flavum is a short but thick ligament that affixes the laminae of adjacent vertebrae from C2 to S1 and is considered a medical ward extension of a facet joint. It contains 80% elastin fibers and 20% collagen fibers. This high percentage of elastin fibers contributes to the ligament with its yellow color and flexible nature.
- Despite the elastic and flexible essence of the ligament, at the neutral position, the ligament has a hypocrisy preventing it from buckling. At the lumbar vertebra, this conceit is given by the traction and tension forces applied by muscles on the Thoracolumbar fascia by the supraspinous, interspinous ligaments to ligamentum flavum causing hypocrisy in the neutral position of the theinterspinous_supraspinous thoracolumbar ligamentous complex
- At any intersegmental level, the ligamentum flavum is a paired structure represented symmetrically on both sides.
- In the neck area, the ligaments are thin but wide and long; ligaments are broader in the thoracic area and broadest in the lumbar area.
Attachments
- The ligament flavum arises from the lower half of the anterior surface of the lamina beyond and connects to the posterior surface and upper margin of the lamina beneath, hammering a cup-like clasp on the upper border of the lamina beneath.
- On either side the ligament divides into two portions:
- The medial portion: gorge to the back of the next lower lamina and astride the gap between the neighboring vertebrae fusing with the interspinous ligament
- The lateral portion: gorge in front of the facet joint where it affixes to the anterior aspect of the inferior and superior articular processes and hammers the anterior capsule. Most lateral fibers extend beyond the superior articular process to the pedicle beneath.
Function
- The point-out elasticity provides to conserve the upright posture and assists the vertebral column in reopening its shape after flexion. It prevents excessive separation of the neighboring vertebral lamina and inhibits buckling of the ligament into the spinal canal during extension, inhibiting canal compression. The lateral part of the ligament prevents the anterior capsule of the facet joint from being hideout within the joint cavity during movement.
Alar ligament
- Two strong rounded cords affix to the skull to C2 Axis.
attachment
- arise from either side of the odontoid process and affix to the medial aspect of the occipital condyles.
function
- firm in flexion, limit rotation, and side flexion to the adverse side.
- Perform a role in stabilizing the C1 and C2 vertebrae of the cervical spine, especially in rotation
intertransverse ligament
- the intertransverse ligaments are ligaments that are implanted in the middle of the transverse processes of the spine.
- In the cervical area, the intertransverse ligament consists of a few irregular, scattered fibers that are often regained by muscles. In the thoracic area, they are rounded cords intimate affix to the deep muscles of the back. In the lumbar area, the intertransverse ligament is thin and membranous.
- The intertransverse ligaments generally blend with the intertransverse muscles.
- The function of the intertransverse ligaments is to prevent lateral flexion of the spine.
Apical ligament of dens
- length in the middle of the 2nd cervical vertebra in the neck and the skull. It stays as a fibrous cord in the triangular interval in the middle of the alar ligaments.
- The apical ligament of dens was on average 7.5 mm long and 5.1 mm broad. Structurally, the ligament is a small association of elastic fibers encompassing a core of notochordal particles essentially it represents an elemental nucleus pulposus that is the particle of notochord seen at other vertebral levels.
attachments
- arises from the tip of the odontoid process on the Axis commonly hammers a small coronal groove located there and insertion into the anterior rim of the foramen magnum at the base on the mid-point.
- The apical ligament is disconnected anteriorly from the anterior atlantooccipital membrane by a thin layer of fat and connective tissue. Posteriorly it is detached from the superior crus of a cruciform ligament by an intervening layer of connective tissue. The tectorial membrane is established farther dorsally, posterior to the cruciform ligament. Laterally the alar ligaments expand from the odontoid process to the medial aspect of the condyles of the occipital bone. There is no accordant relation between the middle of the alar ligament and the apical ligament.
function
- The apical ligament is a small ligament that affixes the apex tip of the dens of the C2 vertebra to the anterior portion of the foramen magnum. It is the weak, fibrous particle of the notochord and does not devote necessarily itself to stability.
Nuchal ligament
- the nuchal ligament is addressed on the back of the neck Continuous with the Supraspinous ligament. It hammers a two-layered fibroelastic septum that detached the dorsal muscles of the neck and spans from the spine of the C7 vertebra to the occiput bone.
attachments
- Extension from the external occipital protuberance on the skull and/or median nuchal line to the spinous process of C7 vertebrae. The deep fibers of the ligament affix to the external occipital crest, the posterior tubercle of the atlas, and the medial surface of the bifid processes of the other cervical vertebrae.
Function
- Limits flexion
- gives a connection in the middle of Trapezius and Splenius capitis.
supraspinous ligament
- The supraspinous ligament or supraspinal ligament is a strong fibrous cord that affixes together with the apices of the spinous processes from the 7th cervical vertebra to the 3rd or 4th lumbar vertebrae. From the C7 vertebra to the skull ligament turn in to structurally specific from more back parts of the ligament and is called the ligamentum nuchae
- Origin: It originates from the C7 vertebra.
- Insertion/Terminates: Sacrum
- The supraspinous ligament is fully grown up only in the upper lumbar area and may terminate at L3 vertebrae, in spite of the most common termination site tending to be at L4 vertebrae. The supraspinous ligament is almost always absent at L5 and S1 vertebrae.
- It is thicker and broader in the lumbar area rather than in the thoracic area, it joins with the thoracolumbar fascia.
- The most superficial fibers of the supraspinous ligament enlarge beyond 3 or/and 4 vertebræ; those more deeply seated ligaments pass in the middle of 2 or /and 3 vertebræ while the deepest ligaments affix the spinous processes of relative vertebrae
- The deep layer of the supraspinous ligament is approved by tendinous fibers of the multifidus muscle. in the middle of the spinous processes, it is prolonged with the interspinal ligaments. The supraspinous ligament’s middle fibers affix with the thoracolumbar fascia’s dorsal layer.
Function
- Limits flexion onward with other ligaments of the vertebral column.
- The supraspinous ligament contributes as a midline affix for some important muscles.
- The supraspinous ligament aids in managing the upright position of the head.
- It’s stretched in flexion, its fibers limit the division of spinous processes during forward flexion, and during hyperflexion, the interspinous ligament and supraspinous ligament are the first to fall.
- At the lumbar area, through the affixation of the supraspinous ligament to the thoracolumbar fascia and interspinous ligament, they hammer together the Interspinous_supraspinous thoracolumbar ligamentous complex which it`s function is to move tension that is addressed on Thoracolumbar fascia to ligamentum flavum causing conceit in the neutral position
Muscle of the cervical spine
Anterior Neck Muscles
- Superficial muscles – platysma, sternocleidomastoid
- Suprahyoids – Digastric, mylohyoid, geniohyoid, stylohyoid
- Infrahyoids – sternohyoid, sternothyroid, thyrohyoid, omohyoid
Vertebral Muscles
- Muscles from musculoskeletal columns around vertebrae. These are subdivided into the anterior, lateral, and posterior vertebral muscle groups.
Anterior (Prevertebral) Vertebral Muscles
- These are also termed Deep cervical flexors:
- Rectus Capitis Anterior
- Rectus Capitis Lateralis
- Longus capitis
- Longus colli/ Longus cervicis
Lateral Vertebral Muscles (Paravertebral)
- Scalenes muscle – anterior, middle, posterior, and/or minimus scalene
Posterior Vertebral Muscles
- These can be subdivided into intrinsic muscles and extrinsic muscles.
Extrinsic muscle
- Trapezius and Levator scapulae
Intrinsic muscles
- Superficial muscles :
- splenius capitis,
- splenius cervicis
Deep muscles:
- Suboccipital group –
- rectus capitis posterior major
- rectus capitis posterior minor
- obliquus capitis inferior
- obliquus capitis superior
- Transversospinalis muscles –
- semispinalis capitis
- semispinalis cervicis
- rotatores cervicis
- the multifidus muscle is known as the deep neck extensors
- Interspinales and intertransversarii.
The Movements and muscles in the cervical spine a
Flexion
- Longus Colli / Sternocleidomastoid
- Scalene anterior
- Longus capitis
- Rectus capitis anterior head only
Extension
- Levator Scapulae
- Splenius cervicis
- Splenius capitis
- Trapezius
- Erector spinae
- The Rectus capitis posterior
- The rectus capitis major
- The rectus capitis minor head only
Lateral Flexion
- Scalene anterior, medius, and posterior
- Sternocleidomastoid
- Splenius capitis
- Trapezius
- Erector spinae
- The Rectus capitis lateralis head only
Rotation
- Semispinalis cervicis
- Multifidus
- Scalene anterior
- Splenius cervicis and capitis
- Sternocleidomastoid
- Inferior oblique head only
- Rectus captitis posterior major head only
range of the movement
- Flexion 50 degrees
- Extension 15 degrees
- Right lateral flexion 20 degrees
- Left lateral flexion 20 degrees
- Right rotation 5 degrees
- Left rotation 5 degrees
What conditions and disorders affect the cervical spine?
- Torticollis
- intervertebral disc prolapse
- osteomyelitis
- osteoporosis
- cervical bulging disc
- cervical herniated disc
- cervical spondylitis
- cervical spondylolisthesis
- cervical spondylolysis
- cervical spine stenosis
- cervical radiculopathy
- cervical myelopathy
Goals for cervical spine mobilization
pain, muscle guarding, and spasm
- painful joint, reflex, muscle guarding, and muscle spasm can be inspected with slight joint play methods to prompt neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and/or distraction movement are used to encourage mechano receptors that may inhibit the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- minor amplitude distraction or/and gliding for movement of the joint is used to generate synovial fluid movement, which is an agent for taking the nutrients to the avascular part of the articular cartilage
- musical joint play techniques help to maintain nutrient exchange and prohibit the painful and degenerating effects of statis when the joint is swollen or/and painful, and can not go over a range of motion
- when the glide is adjusted to treat pain, muscle spasms and muscle guarding small amplitude methods should not apply stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be inspected with a progressively vigorous joint stretching method to elongate hypermobile capsular and ligamentous connective tissue
- uninterrupted or/and distracted stretch forces helped to amplify a shortened tissue mechanically
Positional faults/subluxations
- A faulty or/and inappropriate position of one bony companion in addition to its opposing surface may affect the conclusion in limited motion or/and pain
- postural faults can ensure in traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be conserved
- by maladapted neuromuscular control across a joint
- during inspecting an active range of motion, faulty tracking of the joint surface outcome in pain or/and lessened motions
Progressive limitations
- diseases that progressively prohibit movement can be inspected with joint play techniques to maintain available motion or/and leesen the progressive automated deduction
- the patient’s response is essential for the dosage of distraction or/and glide to treatment and the state of the disease
Functional immobility
- when the patient can’t functionally locomote the joint for a longer period
- the joint can be inspected with non-stretch gliding or/and a distraction procedure to maintain available joint play and prohibit degenerating and reduce the effect of immobility
Grades for cervical spine mobilization
- grade 1 small amplitude oscillations and/or glide are used for pain, modulation, typically during the acute stage of injury
- grade 2 large amplitude oscillations and/or glide are used for pain modulation, dosage, and indication same for grade 1
- grade 3 large amplitude oscillation and/or glide that goes up to the restrictive joint barrier,
- this grade is designed to enhance joint ROM and is used only during the subacute, chronic stage of healing
- grade 4 small amplitude oscillation and/or glide that goes up to the restrictive joint barrier,
- this grade is intended to improve joint ROM and is used only while the chronic stage of healing
- grade 5 (HVT) high velocity and low amplitude thrust/glide applied at the physiologic limit of joint motion
- this grade is performed only one time and solely improves the range of motion
Cervical spine mobilization exercises
Mobilization for cervical flexion

- Patient position: prone with arm relaxing comfortably at patient’s side
- put a pillow beneath the clavicular region for patient comfort and to promote a neutral cervical thoracic curve
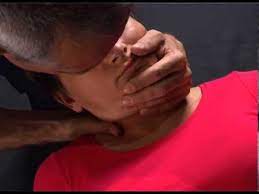
Therapist position and hand placement
- stand on either side of the patient with your body facing toward his/her head
- adopt a two thumbs contact method on the spinous process of the superior restricted segment of the three-joint complex
mobilizing force
- giving the force through the thumbs, slide the superior vertebra in a cephalad anterior direction
- flexion glide is used to increase flexion of the cervical spine
Mobilization for cervical extension

- Patient position: prone with arm relaxing comfortably at patient’s side
- use a pillow for patient comfort and to promote a neutral thoracic curve
Therapist position and hand placement
- stand at the patient’s head side with the body facing toward his/her feet
- use two thumb contact method on the spinous process of the superior restricted segment of the restricted 3-joint complex
mobilizing force
- using the force through the thumbs, slide the superior vertebra in a caudal posterior direction
- extension glide is used to increase the extension of the cervical spine
Mobilization for cervical rotation

- Patient position: prone with arm relaxing comfortably at patient’s side
- take a pillow for patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on either side of the patient with your body facing toward the patient’s head
- apply a two thumbs contact method on the transverse process on the superior restricted vertebrae of the three-joint complex to create rotation toward the direction of restriction
mobilizing force
- giving force through the thumbs, slide the superior vertebra in a cephalad anteromedial direction
- rotation glide is used to increase the rotation of the spine
Mobilization for cervical side bending
- patient position: supine
Therapist position and hand placement
- stand at the edge of the patient’s head with one hand supporting the head and the opposite hand side of the restriction
- the other hand is in contact with the lateral aspect of the vertebra to be manipulated
- the medial side of the second MCP joint should be in contact with the margin of the facet and pillar to be manipulated
- rest of your hand relaxed position on the posterolateral part of the patient’s neck
- passively the therapist places the patient’s head and neck into the flexion, contralateral rotation, and side bending to take up the slack until the segment is treated
mobilizing force
- giving force through the metacarpal joint of the 2nd digits, slide or up glide the cervical facet in an anterior superior medial direction at a 45 degree
- side bending glide is used to increase the side bending of the cervical spine
- side bending accelerates the diameter of the ipsilateral foramen
Alternate technique
- patient position: supine
Therapist position and hand placement
- stand at the edge of the patient’s head with one hand supporting the head and the other hand opposite side of the restriction
- the other hand in relation to the lateral aspect of the vertebra to be manipulated
- the medial side of the 2nd MCP joint should be in contact with the edge of the facet and pillar to be manipulated
- rest of your hand in a relaxed position on the posterolateral portion of the patient’s neck
- passively the therapist places the patient’s head and neck into the extension, ipsilateral rotation, and side bending to catch up the slack until the segment is treated
mobilizing force
- giving force through the metacarpal joint of the 2nd digits, slide or downward glide the cervical facet in an anterior superior medial direction at a 45 degree
Craniocervicle flexion

- patient position: supine with hand put down comfortably on the affected side
Therapist’s position and hand placement and the patient’s attempt
- stand at the edge of the treatment table, support the occiput bone with one hand,
- place another hand across the forehead
- ask the patient to look upward gently
- apply resistance against the patient’s occiput
- initiating gentle isometric contraction in the suboccipital muscles
- when the patient relaxes, take up the relax position by passively nodding the head through any new range
Alternate technique
- sit on a stool at the patient’s head side with your foream relaxing on the treatment table
- one hand stabilizes the c2 vertebra by clasping the transverse process in the middle of the proximal part of the thumb and index finger
- the other hand supports the occiput bone,
- passively by the therapist nod the patient’s head with the hand beneath the occiput to take up the feeble of the suboccipital muscles
- then told the patient to move their eyes upward
- the patient direction looks upward for 3 to 5 seconds and then relax
- after the patient relaxes, take up the relax position by passively nodding the head through any new range
- repeat the methods 3 to 5 times or/and until desired the outcome is achieved
- only the motion in the middle of the occiput bone and c2 vertebrae should occur
- the contraction is gentle and the method is to hold and relax the rectus capitis posterior minor muscle
Craniocervical rotation

- patient position: supine with the hand put down comfortably at the side
Therapist position and hand placement
- stand at the head of the patient
- wrap hands surround the side of the patient’s head with a finger beneath the occiput
- put down the patient’s head in end-range of cervical flexion
- after that, rotate his/her head in the direction of the restriction
- if restricted rotation is to the left side, put down the hand into the end range left rotation
- once the patient is at the end range advise the patient looks in the adverse direction
- while resisting the rotation movement with gentle pressure in opposition to the side of the hand after a 3 to 5-second hold
- the patient has to relax and move the head into a more significant rotation
- this creates gentle isometric contraction of the suboccipital muscles
Precaution for cervical spine mobilization
- if a mobilization procedure creates a change in sensation or an increased pain to radiate down an extremity or/and if a patient reports a feeling of dizziness or lightheadedness or does not perform additional manipulations
- use extreme precaution if the patient reports either a current history of corticosteroid injection use or excessive pain
Joint effusion
- the joint effusion happens due to trauma or/and Diseaserapid swelling of the spine generally designate
- bleeding in the spine and may happen/occur with diseases aspiration of the blood to lessen/reduce the necrotizing effect on an articular cartilage
- slow swelling for more than 4 hours generally designates severe spine effusion or/and edema on the spine due to mild trauma irritation or/and Disease do not stretch the inflamed or/and injured spine with manipulation because the joint capsule is already stretched by being extended to accommodate the extra fluid
- the limitation of movement is, in addition, to add extra fluid and muscle response to pain, not from shortened fibers
- gentle/slight oscillating motion that does not stress the joint capsule may help to block the transmission of a pain stimulus so it is not perceived and may help to initiate/start fluid flow while maintaining available cooperative movement
- if a patient’s response to a slight method is increased/accelerated pain or/and joint irritability
- the method of mobilization was exercised too strenuously or should not be done with the current state of Pathology
Inflamation
- whenever inflamation is present, stretching raises/elevate the pain and muscle guarding conclusion in greater tissue damage
- slight distraction movements may temporarily decelerate the pain response
hypermobility
- the joint of the patient with probable necrosis of ligaments or/and joint capsules should not be manipulated with stretching methods
FAQS
- how do the mobilization for torticollis ??
the passive mobilization phase is applied by slight but tight gripping of the sterno cleno mastoid muscle two or three fingers below the muscle origo and the muscle is mobilized rhythmically in the anteroposterior direction.
- how much time the mobilization is given for the cervical spine ??
soft tissue mobilization was applied three times a week and home program exercises were recommended which consisted of positioning the neck and head
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation initiate within range, not achieve the limit of the movement, apply the glide for 2 or/and 3 seconds for 1 to 2 minutes
that goes center point into the joint range of movement, attending any part of the range and still not arriving the end range. This procedure can be given to treat stiffness by accelerating the range of motion and/or pain - When do we use joint mobilization for the cervical spine?
The major goal of cervical spine mobilization is to regain the normal joint play movement that might have been compromised by damage or/and injury. Normal movement of the affected cervical spine will be recouped faster if it is compromised early in the treatment program. Also, mobilization is advantageous in cases when the range of motion is not present in the cervical spine
- How long do you do joint mobilization for the cervical spine?
Typical treatment of the cervical spine joint may add a series of 3 to 6 mobilizations grasp on up to 30 seconds, with 1 to 3 oscillations or/and glide per second