Osteoarthritis of Knee: Physiotherapy Treatment and Exercises
Table of Contents
What is Osteoarthritis of the Knee?
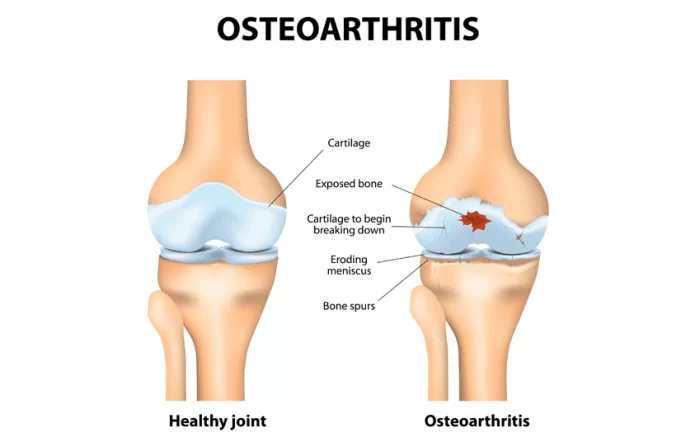
Osteoarthritis of knee is the most common form of arthritis in the knee. It is a degenerative,” wear-and-tear” type of arthritis that occurs most often in people 50 years of age and older, but may occur in younger people, too.
~ In osteoarthritis, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful bone spurs.
~Osteoarthritis develops slowly and the pain it causes worsens over time.
ANATOMY and PATHOLOGICAL Process
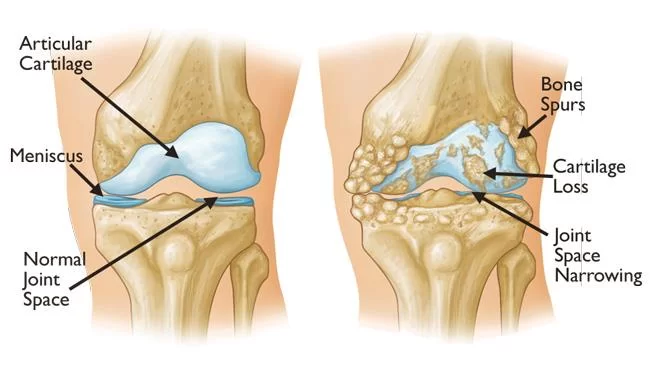
~ The knee joint consists of both approximation of the proximal tibia and the distal end of the femur. The cartilage located on the ends of the femur and tibia contains an extracellular matrix that contains type 2 protoglycans that function by drawing fluid into the joint causing increased shock absorption and proper joint nutrition. There is some evidence to support that as the aging process occurs the type 2 collagen fibers decrease in size and therefore less fluid and nutrition gets into the joint surfaces eventually leading to decreased protection along bony surfaces. femoral condyles and the concave tibial condyles. There is also the art. patellofemoralis between the femur and the patella and the art. tibiofibularis located between the tibia and fibula. OA can only occur in the two primary articulations of the knee, namely the tibiofemoral and
~ The knee (art. genus) is a synovial joint, which consists of 3 articulations. The primary joint, art. tibiofemoral, is located between the convex patellofemoral joint because they have to sustain more motion than the art. tibiofibularis.
~ “The pathogenesis of knee OA has been linked to biomechanical and biochemical changes in the cartilage of the knee joint.” The cartilage ensures that the bone surfaces can move painlessly and with low friction to each other. In OA, the cartilage decreases in thickness and quality, it becomes thinner and softer, cracks may occur and it will eventually crumble off. Cartilage that has been damaged, cannot recover. Finally, the cartilage will disappear. The bone surfaces can also be affected, the bone will expand and spurs (osteophytes) will develop. Not only the cartilage can be affected, there can also be laxity of the ligaments and muscle atrophy.
Causes of Osteoarthritis
1. Age:
As you age it is normal for joint surfaces to “wear down”, especially the major weight-bearing joints of the lower limb. The ability of joint cartilage to repair itself also declines as you grow older.
2. OverWeight (Obesity) :
Your weight will directly affect the amount of loading the knee joints in your lower limb have to support during weight-bearing activities.
3. Previous Knee Joint Injury:
A previous injury to your knee can change the biomechanics of your knee joint. This leads to an abnormal distribution of load through the knee in everyday tasks.
4. Genetics:
The gene that produces your articular knee cartilage is sometimes defective and can lead to either decreased lay down of cartilage, or normal lay down of defective cartilage on the joint surfaces.
5. Jobs or Sports that repeatedly load your knee joint:
Joint compression is essential for stimulating joint nutrition. Repetition of activities that excessively load the knee joint, such as squatting, lifting heavy objects, and running, has been linked to an earlier onset of knee arthritis.
Stages of Osteoarthritis of Knee:
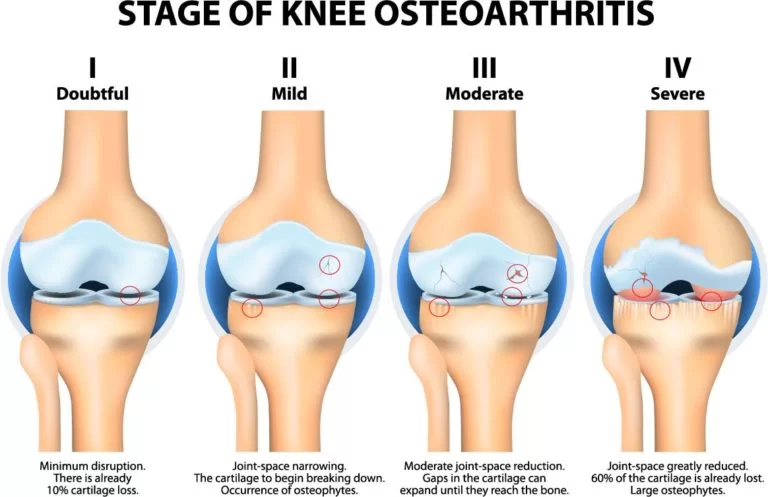
Osteoarthritis of knee is a degenerative condition that sees the cartilage in the knee slowly wear away. The cartilage in the knee joint becomes rough an breaks down over time, causing an overgrowth of the bone underneath. OA gradually develops over many years and can go undetected until you reach the later stages. The progression of OA is measured in four stages. The four stages of Osteoarthritis progression from minor to severe :
Stage 1 – Minor – Little or no Pain or Discomfort
In stage one, there is already a small loss of cartilage (around 10%). Osteophytes, small outgrowths of bone, may also start growing in the knee joint. While there is some cartilage loss, there is little to no narrowing of the joint space between the bones.
Stage 2 – Mild – Some Pain and Joint Stiffness:
~ Stage two sees a continuing loss of cartilage and noticeable osteophyte growth. While the space between the joints (joint space) remains healthy, the places where the bones make contact start to harden, along with the surrounding tissues. Damage to the knee joint at this stage is still minor; the bones are not rubbing or scraping against each other.
Stage 3 – Moderate – Pain, Discomfort, and Swelling:
In stage three, there is a notable loss of cartilage, and the joint space has noticeably narrowed. This stage also sees the joint becoming swollen and inflamed.
Stage 4 – Severe – Intense Pain, Discomfort, Loss of Mobility:
~ Stage four is the most advanced with 60% of knee cartilage worn away. The joint space is significantly narrowed with the bones touching each other. The friction caused by the bones rubbing against each other causes significant inflammation. Patients at this stage of OA typically see the growth of more osteophytes, experience intense pain and in very severe cases the bones may become deformed.
What are osteoarthritis symptoms?
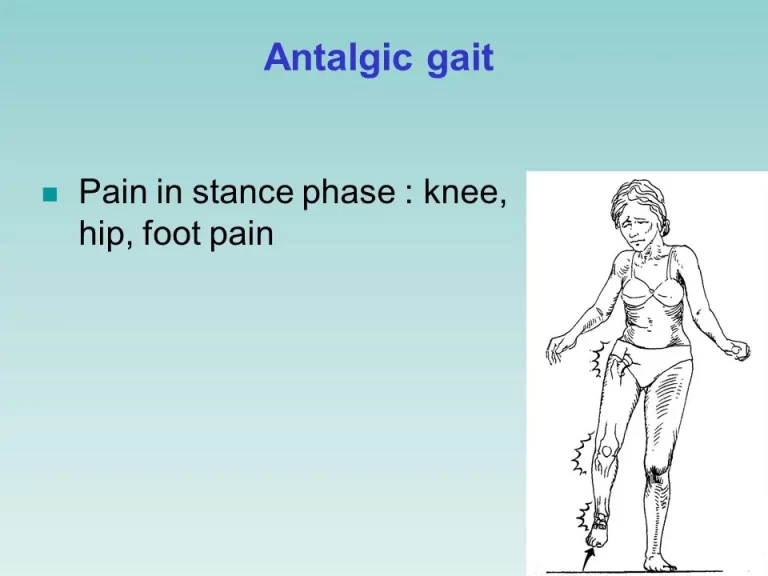
- Loss of flexibility: You may not be able to move your joint through its full range of motion.
- Grating sensation: You may hear or feel a grating sensation when you use the joint.
- Bone spurs: These extra bits of bone, which feel like hard lumps, may form around the affected joint.
- Tenderness: Your joint may feel tender when you apply light pressure to it.
- Knee pain that increases when you are active, but gets a little better with rest
- Knee joint swelling
- feeling of warmth in the knee joint.
- stiffness in the knee, especially in the morning or when you have been sitting for a while
- decrease in mobility of the knee, making it difficult to get in and out of chairs or cars, use the stairs, or walk
- Creaking, crackly sound is heard when the knee moves
Diagnosis:
A diagnosis of osteoarthritis of the knee based on your symptoms and an examination. During the examination, they’ll check for:
- tenderness over your knee
- creaking and grating (crepitus)
- bony swelling
- excess fluid
- restricted movement
- instability of your knee
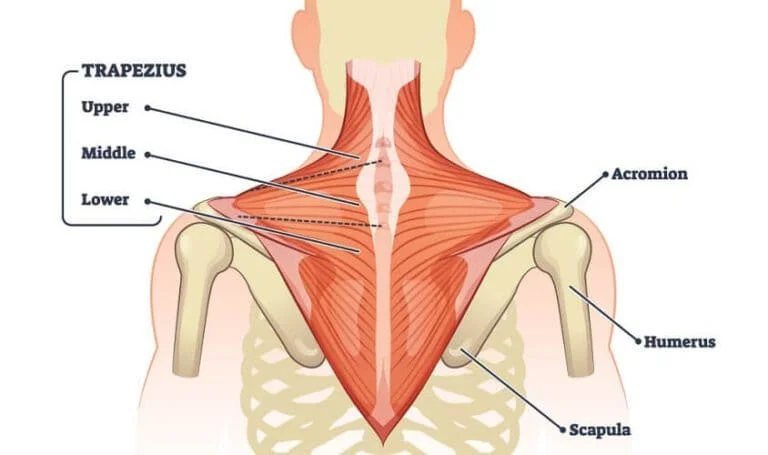
- thinning of the muscles that support your knee.
X-rays: Cartilage doesn’t show up on X-ray images, but cartilage loss is revealed by a narrowing of the space between the bones in your joint. An X-ray may also show bone spurs around a joint. Some people may have X-ray evidence of osteoarthritis before they experience any symptoms.
Magnetic resonance imaging (MRI): An MRI uses radio waves and a strong magnetic field to produce detailed images of bone and soft tissues, including cartilage. An MRI isn’t commonly needed to diagnose osteoarthritis but may help provide more information in complex cases.
Lab tests: Analyzing your blood or joint fluid can help confirm the diagnosis.
Blood tests: Although there is no blood test for osteoarthritis, certain tests may help rule out other causes of joint pain, such as rheumatoid arthritis.
Joint fluid analysis: use a needle to draw fluid out of the affected joint. Examining and testing the fluid from your joint can determine if there’s inflammation and if your pain is caused by gout or an infection
MEDICAL TREATMENT:
- Acetaminophen: A pain and fever relieving OTC (Over-the-counter drug) drug. Because of its safety and mild effectiveness, it is one of the most used oral medicines. It is also proven to be effective when acetaminophen can be combined with other drugs, e.g. ibuprofen, both with lower doses.
2.NSAIDs: If there isn’t any significant or positive response to the use of acetaminophen, NSAID is then recommended. NSAIDs are primarily used for joint pain. Despite its common use, the consumption of this drug should be limited to short-term, in order to control episodic painful flares and to prevent other side effects, such as myocardial infarction and stroke.
There are two forms of Nonsteroidal inflammatory drugs:
- Oral NSAIDs
- Topical NSAIDs
Both forms are advised to contain cyclooxygenase 1 and 2 (COX-1 and COX-2) inhibitors, which help in gastric mucosa protection.
3. Opioids: When there is a lack of reaction to NSAIDs, opioids are used. Both Tramadol and codeine contain opioids, which are refractory pain-relieving medicines that are generally used for the treatment of moderate to severe knee OA.
4. Intra-articular injections: Pain-relieving fluids that are consumed if opioids aren’t sufficient. They are directly injected into the arthritic joint of the knee in full extension. Hyaluronic acid and corticosteroids are examples of injected fluids.
Surgery for Osteoarthritis of Knee:
- high-tibial osteotomy
~ indications
younger patients with medial unicompartmental OA
~ technique
valgus producing proximal tibial osteotomy
2. unicompartmental arthroplasty (knee)
~ indications
isolated unicompartmental disease
~ outcomes
TKA has lower revision rates than UKA in the setting of unicompartmental OA
3. total knee arthroplasty
~ indications
symptomatic knee osteoarthritis
failed non-operative treatments
~ techniques
cruciate retaining vs. cruciate sacrificing implants show no difference in outcomes
patellar resurfacing
no difference in pain or function with or without patella resurfacing
lower reoperation rates with resurfacing
drains are not recommended
PHYSIOTHERAPY TREATMENT:
Physiotherapy treatment are most important part of treatment, In early phases it’s highly effective for the permanent solution of osteoarthritis. It may include pain-relieving electrotherapy modalities like. IFT, TENS, Ultrasound with Rest, and Knee Exercise.
IFT (Interferential therapy): Interferential Current stimulation is very useful in the treatment of circulatory and muscular disorders, stiffness of joints, edema, and inflammation.
TENS is a method of electrical stimulation that primarily aims to provide a degree of symptomatic pain relief.
Ultrasound Therapy: The use of Sound-wave in Physiotherapy Physiological Healing And Pain Relieving Effects is known as Ultrasound Therapy.
~ Cold therapy: By reducing circulation, cold therapy can help decrease swelling.
~ Heat therapy: Heat therapy increases blood flow to decrease stiffness in the knee joints and muscles surrounding the knee.
~ Knee Braces: Your physiotherapist may recommend the use of a knee brace to support your knee and help to de-load certain structures. There are many different styles available and it is important to find one that suits your individual needs!
Osteoarthritis Knee exercises:
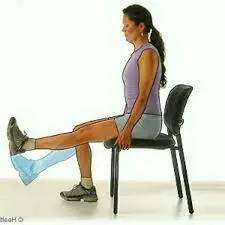
SITTING QUADS:
Sit on a chair with both legs bent at 90°.
Slowly raise your right leg so that it’s parallel to the floor, keeping your left foot on the ground.
Hold for 30 seconds, then slowly bring the right foot back to the floor, and repeat on left leg.
Do 10 times twice a day.
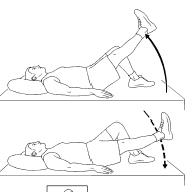
STRAIGHT LEG RAISING (SLR)
Lie flat on your back on the floor or bed with your arms at your sides, and toes up.
Keep your leg straight while tightening your leg muscles, and slowly lift it several inches.
Tighten your stomach muscles to push your lower back down.
Hold and count to 5, then lower your leg as slowly as possible.
Repeat, then switch to the other leg.

STATIC QUADS:
Lie on your back with the leg you want to exercise straight. Place a small rolled towel underneath the knee. Slowly tighten the muscle on top of the thigh (quadriceps) and push the back of the knee down into the rolled towel. Hold the contraction for 5 seconds and then slowly release, resting 5 seconds between each contraction. Perform 3 sets of 10 repetitions, 1 time daily.

CALF STRETCH:
Stand facing a wall with the leg to be stretched behind you and the other leg in front. Place your hands or forearms on the wall for support.
Slowly bend the front knee, keeping the heel of the leg behind you down on the floor. Once you feel a stretch in your calf muscle at the back of your ankle, hold for 30 seconds. Slowly relax. Perform 3 repetitions
DO’S & DON’TS:
Do exercise daily: Regular cardio exercise strengthens the muscles and increases the flexibility of your knee. It includes walking, swimming, water aerobics, and stationary cycling.
Do use the “RICE” Principle: Rest, ice, compression, and elevation are beneficial for Knee pain which is caused by a minor injury. Give rest to your Knee then apply ice to reduce swelling, wear a bandage to keep your knee elevated.
Do consider acupuncture: It is a Chinese practice of inserting needles in specific points on the body to change the flow of energy.
Don’t overlook your weight: Being Overweight has a negative impact on your knee; losing weight reduces stress on your knees. Smaller changes in weight can make bigger differences.
Don’t be shy about using a walking aid: A crutch can decrease the stress on your knee. Knee splints and braces also help you to stay stable.
Don’t let your shoes make matters worse: Doctors always recommend special insoles that you fix in your shoes. It will reduce stress on your knees. Take advice from the doctor to find the appropriate insole.
Don’t risk a fall: An unstable Knee can cause more knee damage. Use handrails on staircases or sturdy ladders to catch something from a high shelf.
Don’t rest too much: Stick with a daily exercise program because too much rest can weaken your muscles, which can worsen joint pain. If you don’t know how to do exercise then take advice from the doctor or therapist.
FAQ
Osteoarthritis is mostly treated with lifestyle changes, such as eating a balanced diet and doing frequent exercise. medicine to ease your discomfort.
supportive therapies: to aid in easing the burden of daily tasks.
The 4 stages of Knee osteoarthritis are:
Stage 1- Minor
Stage 2-Mild
Stage 3 -Moderate
Stage 4 -Severe
Pain in the joints.
Increase Pain, and stiffness after a prolonged period of immobility.
Joints that seem a little bigger or more crooked than normal.
A feeling or sound in your joints that is grating or crackling.
Restricted joint range of motion.
The good news is that osteoarthritis, the most prevalent kind of arthritis, may be managed and even improved with time. Its agony and its effects are something you can overcome.




15 Comments