Myofascial Release Therapy
Table of Contents
DEFINITION :
- Myofascial pain syndrome is a common clinical problem of muscle pain involving sensory, motor, and autonomic symptoms caused by myofascial trigger points. Despite myofascial pain is commonly found in clinical practice, there are few prevalence studies found in the scientific literature. Skootsky et al. found that 30% of patients that visited a primary care unit presented myofascial trigger points. In a recent study regarding shoulder pain, Bron et al. concluded that all 72 subjects included in their study presented myofascial trigger points in shoulder girdle muscles, mainly in the infraspinatus muscle and upper trapezius.
- A myofascial trigger point is defined as a hyperirritable spot, usually within a taut band of skeletal muscle which is painful on compression and can give rise to characteristic Referred Pain, motor dysfunction, and autonomic phenomena.
WHAT IS MYOFASCIAL RELEASE?
- Myofascial Release is a safe and very effective hands-on technique that involves applying gentle sustained pressure into the Myofascial connective tissue restrictions to eliminate pain and restore motion. This essential “time element” has to do with the viscous flow and the piezoelectric phenomenon: a low load (gentle pressure) applied slowly will allow a viscoelastic medium (fascia) to elongate.
- Trauma, inflammatory responses, and/or surgical procedures create Myofascial restrictions that can produce tensile pressures of approximately 2,000 pounds per square inch on pain-sensitive structures that do not show up in many of the standard tests (x-rays, myelograms, CAT scans, electromyography, etc.)
- The use of Myofascial Release allows us to look at each patient as a unique individual. Our one-on-one therapy sessions are hands-on treatments during which our therapists use a multitude of Myofascial Release techniques and movement therapy. We promote independence through education in proper body mechanics and movement, self-treatment instruction, enhancement of strength, improved flexibility, and postural and movement awareness.
- Myofascial release (MFR, self-myofascial release) is an alternative medicine therapy that claims to treat skeletal muscle immobility and pain by relaxing contracted muscles, improving blood and lymphatic circulation, and stimulating the stretch reflex in muscles.
- Fascia is a thin, tough, elastic type of connective tissue that wraps most structures within the human body, including muscle. Fascia supports and protects these structures. Osteopathic theory proposes that this soft tissue can become restricted due to psychogenic disease, overuse, trauma, infectious agents, or inactivity, often resulting in pain, muscle tension, and corresponding diminished blood flow.
- The use of myofascial release as a treatment is not supported by good evidence; as a replacement for conventional treatment, it risks causing harm.
ETIOLOGY:
- Several possible mechanisms can lead to the development of myofascial trigger points, including low-level muscle contractions, muscle contractures, direct trauma, muscle overload, postural stress, unaccustomed eccentric contractions, eccentric contractions in unconditioned muscle, and maximal or submaximal concentric contractions.
> Low-level muscle contractions:
Low-level muscle contractions involve a selective overload of the earliest recruited and last derecruited motor units (“Henneman’s size principle”). Smaller motor units are recruited before and derecruited after larger ones; as a result, the smaller type I fibers are continuously activated during prolonged motor tasks, which in turn it can result in metabolically overloaded motor units with subsequent activation of autogenic destructive processes and muscle pain, this is also known as the Cinderella hypothesis.
> Muscle contractures:
Prolonged contractures are likely to lead to the formation of taut bands inside muscle fibres. The taut band is the first sign of the muscular response to biomechanical stress. This can lead to the formation of latent trigger points, which can eventually evolve into active trigger points
> Direct trauma:
Direct trauma may create a vicious cycle of events wherein damage to the sarcoplasmic reticulum or the muscle cell membrane may lead to an increase of the calcium concentration, subsequent activation of actin and myosin, a relative shortage of adenosine triphosphate (ATP), and an impaired calcium pump, which in turn will increase the intracellular calcium concentration, even more, completing the cycle. As a result, taut bands inside muscle may be developed and lead to the formation of active or latent myofascial trigger points.
> Maximal or submaximal concentric contractions:
During maximal or submaximal concentric contractions high amounts of energy (ATP) are required. When the demands of exercise begin to exceed the ability of the muscle cells to produce ATP, anaerobe glycolysis will begin consuming more and more of the available intracellular ATP. The muscle will eventually run out of ATP and sustained muscle contractions may occur, starting the development of trigger points.
PATHOPHYSIOLOGY:
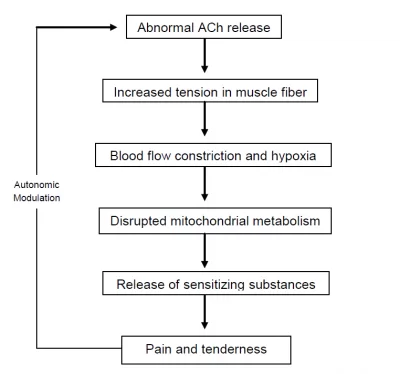
- The initial change in a muscle that is associated with myofascial pain seems to be the development of the taut band, which is in terms a motor abnormality. Several mechanisms have been hypothesised to explain this motor abnormality, the most accepted one is the “Integrated Hypothesis” first developed by Simmons and later expanded by Gerwin.
- Simmons’ integrated hypothesis is a six-link chain that starts with the abnormal release of acetylcholine. This triggers an increase in muscle fiber tension (formation of a taut band). The taut band is thought to constrict blood flow which leads to local hypoxia. The reduced oxygen disrupts mitochondrial energy metabolism reducing ATP and leading to tissue distress and the release of sensitizing substances. These sensitizing substances lead to pain by activation of nociceptors and also lead to autonomic modulation that then potentiates the first step: abnormal acetylcholine release.
DIAGNOSIS :
- Palpation is the gold standard in identifying the presence of taut bands in muscle. This involves the training and accurate skills of practitioners to identify these taut bands.
- Palpation of taut bands needs a precise knowledge of muscle anatomy, the direction of specific muscle fibres, and muscle function.
- The palpation of muscle must meet several essential criteria and confirmatory observations to identify the presence of trigger points.
> Essential criteria:
– Taut band palpable (where a muscle is accessible)
– Exquisite spot of tenderness in a taut band
– Patient recognition of current pain complaint by the pressure of the examiner
– Painful limit to full stretch ROM
> Confirmatory observations:
– Visual or tactile local twitch response
– Referred pain sensation on compression of the taut band
– SEA confirmed by electromyography
- The interrater reliability of palpation has been a subject of scientific research over the past years. There has been improvement in the methodological quality in recent studies but the main problem rests in the lack of rater blinding. It is a problem hard to solve because the reliability of palpation depends on the high expertise level of the examiner.
- Recent research has shown interesting results using magnetic resonance elastography. The technique involves the introduction of cyclic waves into the muscle and then using phase contrast imaging to identify tissue distortions. The speed of the waves is determined by the images. Shear waves travel more rapidly in stiffer tissues. The taut band can then be distinguished from the surrounding normal muscle.
- Another recent technique used to confirm the extension of myofascial trigger point sites is sonoelastography combined with Doppler imaging.
- It uses a clinical ultrasound imaging system with a 12-5 MHz linear array, associated with an external vibration source (hand-held vibrating massager) working at cycles of approximately 92Hz. Doppler imaging is used to identify surrounding blood flows.
- Ballyns et al. showed in their study that sonoelastography can be a useful tool to classify myofascial trigger points by area. Larger areas correspond to active trigger points and smaller ones to latent trigger points.
Note that this technique needs preliminary manual palpation of trigger points.
DIFFERENTIAL DIAGNOSIS:
- One source of confusion associated with myofascial pain is fibromyalgia. It is true that both entities are likely to cause severe muscle pain and tenderness but they do not share the same etiology or pathogenesis and their clinical presentation is not the same. Therefore two different conditions should be distinguished.
- In 1990 the American College of Rheumatology published the diagnostic and classification criteria for fibromyalgia. This classification has been updated recently in 2010.The diagnosis of fibromyalgia is based on a history of widespread pain (for at least 3 months of duration), defined as bilateral, upper and lower body, as well as spine, and the presence of excessive tenderness on applying pressure to 11 of 18 specific muscle-tendon sites or tender points.
- Main differences between myofascial pain and fibromyalgia:
– Myofascial Pain Fibromyalgia
– Local Pain Widespread Pain
– Regional Condition Bilateral as well as axial Pain
– Presence of Taut Band Absence of taut bands Referred Pain Presence of at least 11 tender points - A differential diagnosis should be made with other conditions such as muscle spasm, neuropathic or radicular pain, delayed onset muscle pain, articular dysfunction, and infectious myositis.
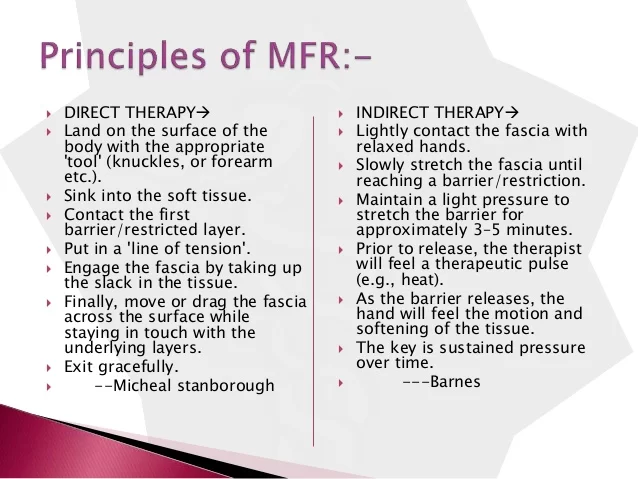
PRINCIPLES OF MFR:
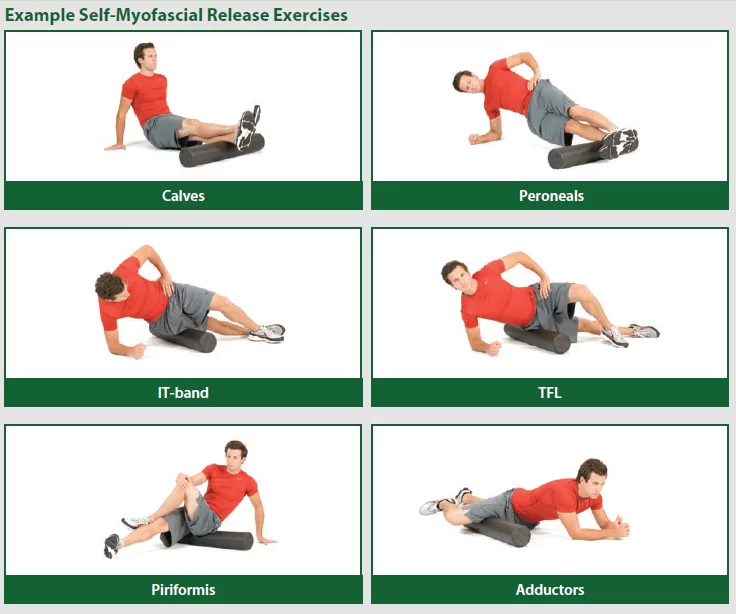
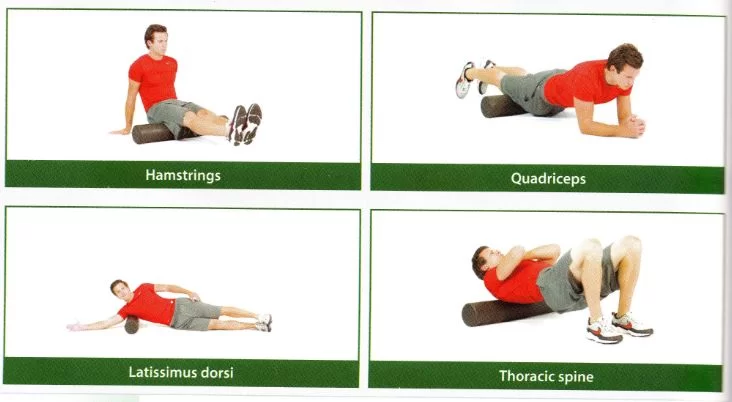
COMMON BODY PARTS TREATED BY MFR:

- There are many common body parts that can be treated with myofascial release. Common body parts treated by myofascial release are:
– Upper back
– Lower back
– Buttock
– Thigh
- Myofascial release can also be performed on other areas of the body and be effective to reduce pain and tightness in soft tissues.

MANAGEMENT OF MYOFASCIAL RELEASE :
- There are two different approaches to the treatment of myofascial trigger points. There are non-invasive techniques such as Ultrasound therapy, Low-level laser therapy, Transcutaneous Electrical Nerve Stimulation (TENS), drug therapy (e.g. myorelaxants), and several physical and manual therapy techniques such as:
– Stretching techniques (e.g. spray and stretch)
– Post-isometric relaxation
– Active Release Techniques
– Trigger point pressure release
– Muscle energy techniques
– Massage
- In a recent study, Bron et al.conducted a controlled trial in the treatment of myofascial trigger points in patients with shoulder pain. They decided to only use manual techniques associated with home exercises and ergonomic recommendations. After 12 weeks of treatment, there was a statistically significant improvement in the intervention group compared with the control group.
- On the other hand, there are different invasive techniques that share a common goal: the inactivation of an active loci in a central trigger point with a needle.
Different modalities exist:
– Dry needling
– Anesthetic injections
– Botulin toxin A injection
COMMON EQUIPMENT USED IN MFR:







Mayofascial Release the Best Physiotherapy Technique we use in Our Clinic for Muscular Pain, Informative Article.