DRY NEEDLING TECHNIQUE
 DRY NEEDLING
DRY NEEDLING
DRY NEEDLING
# INTRODUCTION :-
- Dry needling, also known as myofascial trigger point dry needling,is an unproven technique in alternative medicine similar to acupuncture. It involves the use of either solid filiform needles or hollow-core hypodermic needles for therapy of muscle pain, including pain related to myofascial pain syndrome. Dry needling is sometimes also known as intramuscular stimulation (IMS).
- While many studies have been performed to test the efficacy of dry needling as a treatment for muscle pain, there remains no scientific consensus as to whether or not it is effective.Some results suggest that it is an effective treatment for certain kinds of muscle pain, while other studies have shown no benefit compared to a placebo. There are not enough high-quality studies of the technique to draw clear conclusions about its efficacy.
# WHAT IS DRY NEEDLING :-
- Dry needling is a modern treatment designed to ease muscular pain. Its popularity is growing. During dry needling, a practitioner inserts several filiform needles into your skin. Filiform needles are fine, short, stainless steel needles that don’t inject fluid into the body. That’s why the term “dry” is used.
- Practitioners place the needles in “trigger points” in your muscle or tissue. Dry needling is also sometimes called intramuscular stimulation. The points are areas of knotted or hard muscle.
- Dry needling practitioners say the needle helps release the knot and relieve any muscle pain or spasms. The needles will remain in your skin for a short period of time, often between 10 and 30 minutes.
# BASIC ABOUT DRY NEEDILING :-
- Trigger-point dry needling is an invasive procedure where an acupuncture needle is inserted into the skin and muscle. It is aimed at myofascial trigger points which are hyperirritable spots in skeletal muscle that are associated with a hypersensitive palpable nodule in a taut band. Trigger point dry needling can be carried out at superficial or deep tissue level.* Superficial dry-needling :
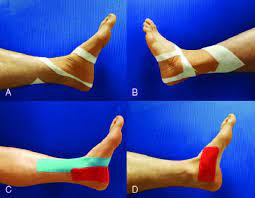
- This was developed by Peter Baldry. He recommended the insertion of needles to 5-10mm over a MTrP ( Mayofecial Triger Point ) for 30 secs. Palpation of the MTrP then determined the level of response and whether needle stimulation was sufficient to alleviate MTrP pain. If not the need was re-inserted.

SUPERFICIAL DRY NEEDLING
* Trigger point model :
- The trigger point model is a dry needling technique that specifically targets myofascial trigger points. They are thought to be due to an excessive release of acetylcholine from selected motor endplates. They can be divided into Active and Latent myofascial trigger points.
- Active trigger points can spontaneously trigger local or referred pain. They cause muscle weakness, restricted ROM and autonomic phenomena.
- Latent trigger points do not cause pain unless they are stimulated. They may alter muscle activation patterns and contribute to restricted ROM.
- Therefore both active and latent trigger points cause allodynia at the trigger point site and hyperalgesia away from the trigger point following applied pressure.
- The formation of trigger points is caused by the creation of a taut band within the muscle. This band is caused by excessive acetylcholine release from the motor endplate combined with inhibition of acetylcholine esterase and upregulation of nicotinic acetylcholine receptors.
- Initially taut bands are produced as a normal protective, physiological measure in the presence of actual or potential muscle damage. They are thought to occur in response to unaccustomed eccentric or concentric loading, sustained postures and repetitive low load stress. However when sustained they contribute to sustained pain.
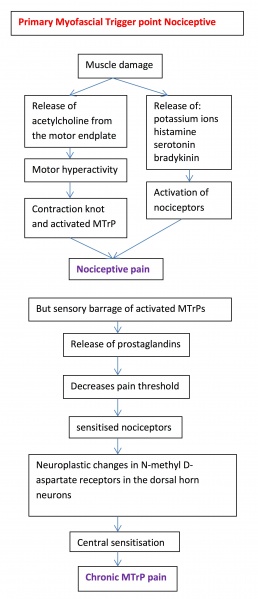
- Pain caused by trigger points is due to hypoxia and decreased bloodflow within the trigger point. This leads to a decreased pH which activates the muscle nociceptors to restore homeostasis. This causes peripheral sensitization.
- Trigger points are also involved in central sensitization. The mechanism remains unclear but trigger points maintain nocioceptive input into the dorsal horn and therefore contribute to central sensitization.

TRIGGER POINT DRY NEEDLING
# DIFFRENT FORMS OF DRY NEEDLING :-
- Dry Needling refers to both drug-free needling of trigger points in the treatment of myofascial pain and dysfunction, as well as the treatment of other musculoskeletal pain using sterile disposable acupuncture needles. There are basically two different types of Dry Needling:
1. intramuscular stimulation (IMS) and
2. superficial Dry Needling (SDN).
- In IMS, the needle is inserted directly into the trigger point or taut band. This triggers a local twitch response (LTR) of the taut band. The LTR is perceived by many patients as a sensation of muscular release and as a sign that the right trigger point was needled. In addition, there is evidence to support the therapeutic value of the LTR in enhancing the release of fascia related adhesions, as well as to reduce inflammation around the Trigger Point.
- In SDN, the needle is inserted superficially obliquely to the skin surface, to about 3-4 mm above the trigger point or painful area. This triggers several reflex analgesic mechanisms via the spinal cord and the brain.
- Another method of Dry Needling is the intramuscular electrical stimulation (IMES), where at least two needles are inserted into the taut band and are stimulated by light TENS currents.
- The proper technique must always be chosen and adapted according to the patient and his complaints.

NEEDLING FOR TRAPAZIUS PAIN
# EFFECTS OF MECHANISMS :-
> Mechanical effects
– Dry Needling may mechanically disrupt a dysfunctional motor end plate
– Needling results in a Local Twitch Response (LTR)
– The LTR results in an alteration to muscle fiber length as well as having an inhibitory effect on antagonistic muscles
> Neurophysiological effects
– Baldry (2001) suggests that dry needling techniques stimulate A-nerve fibers (group III) for as long as 72 hours post needling
– Prolonged stimulation of the sensory afferent A-fibers may activate the enkephalinergic inhibitory dorsal horn interneurons, which implies that dry needling causes opioid mediated pain suppression
– Another possible mechanism of dry needling is the activation of descending inhibitory systems which would block noxious stimulus into the dorsal horn
– The LTR may also utilize the excessive ACh in the tissue which previously was triggering increased firing of localized fibers
> Chemical effects
– Studies by Shah and colleagues (2001) demonstrated increased levels of various chemicals at sensitized motor end plates such as: Bradykinin, Substance P and CGRP (regulator of Calcium and Phosphate balance). These chemicals were reduced immediately post a LTR.
– CGRP enhances the release of ACh from nerve terminals, which results in increased ACh receptors at the neuromuscular junction.
– Needle penetration will cause micro-trauma and micro bleeding (localized inflammation) and hence the introduction of PDGF into the area to help promote healing.
> Stimulation of a local twitch response (LTR)
– Dry-needling of these myofascial trigger points via mechanical stimulation causes an analgesic effect. This mechanical stimulation causes a local twitch response (LTR). An LTR is an involuntary spinal cord reflex contraction of the muscle fbers in a taut band. Triggering an LTR has been shown to reduce the concentration of nociceptive substances in the chemical environment near myofascial trigger points.
> Muscle regeneration
– The needle may cause a small focal lesion which triggers satellite cell migration to the area which repair or replace damaged myofibers. This occurs 7-10 days after dry needling. It is unclear whether continued dry needling within this period may disrupt this process.
> A localised stretch to the cytoskeletal structures
> This stretch may allow sarcomeres to resume their resting length.
> Electrical polarization of muscle and connective tissue
> The mechanical pressure causes collagen fibers to intrinsically electrically polarize which triggers tissue remodelling.
# TECHNIQUES OF DRY NEEDLING :-

> In-and-out techniques
- Some forms of dry needling use a technique called pistoning or sparrow pecking. Both of these techniques rely on in-and-out needle insertion. In other words, the needles don’t stay inserted in the skin for a period of time. The needles prick the trigger points and are then removed. However, research does not support this method of dry needling.
> Non-trigger point technique
- Some dry needling techniques treat a broader landscape of the central nervous system. This is called non-trigger point treatment. Instead of inserting needles only in the area of pain, the practitioner may instead insert needles in areas around but not directly on the point of pain.
- This technique relies on the idea that pain is the result of a greater nerve or muscular issue, not a focused one only in the main area of pain.
- Dry needling is most often performed by physical and sports injury therapists. Currently, dry needling practitioners don’t need extensive training to perform dry needling. No regulatory agency controls training, licensure, or supervision for this procedure.
- Because there’s no credentialing board, there’s also no way to determine if someone’s training is legitimate and satisfactory.

NEEDLING FOR GASTROCNEMIUS MUSCLE
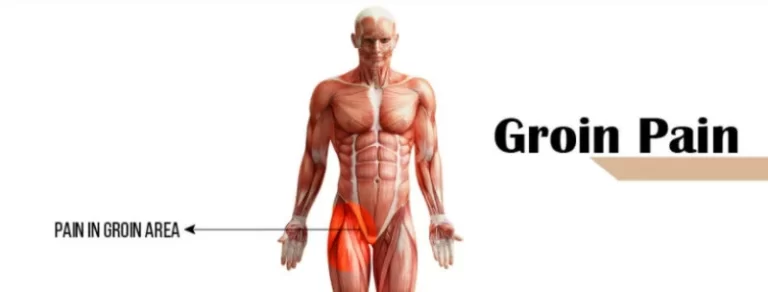
# INDICATION :-
– dentification of myofascial trigger points in the muscle through palpation
– Deep dry needling reproduces the patient’s pattern of pain
– Identification of ‘Jump’ and ‘Shout’ sign on palpation on MTrP
* The minimum criteria for diagnosis of myofascial trigger points are:
– Spot tenderness in a palpable band of skeletal musle
– Subject recognition of pain with palpation
– Clinical presentation
# ABSOLUTE CONTRAINDICATION :-
* DN therapy should be avoided in patients under the following circumstances :
– In a patient with needle fobia.
– Patient unwillng – fear, patient belief.
– Unable to give consent – communication, cognitive, age-related factors.
– Medical emergency or acute medical condition.
– Over an area or limb with lymphedema as this may increase the risk of infection/cellulitis and the difficulty of fighting the infection if one should occur.
– Inappropriate for any other reason.
# RELATIVE CONTRAINDICATION :-
-Abnormal bleeding tendency
-Compromised immune system
-Vascular disease
-Diabetes
-Pregnancy
-Children
-Frail patients
-Patients with epilepsy
-Phychological status
-Patient allergies
-Patient medication
-Unsuitable patient for any reason
# POST TREATMENT :-
-Assess range of motion (ROM) for restriction and pain
-Give patient a stretching programme
-Identify activities that may reactivate MTrP
# KEY POINTS ABOUT NEEDLING :-
- The effectiveness of this treatment depends greatly on the skill of the therapist to accurately palpate mysofascial trigger points as well as kinaesthetic awareness of the anatomical structures.
- A cochrane review (2005) of RCTs concluded that trigger point dry needling may be beneficial for low back pain when used in combination with other treatments. However further higher quality studies are needed to confirm this.
- It is suggested that dry-needling reduces/removes nociceptive input from trigger points, normalize synaptic efficacy and reduce peripheral and central sensitization.
- Dry-needling can restore muscle activation and strength as well as Range of motion (ROM).
- Dry-needling decreases pain in patients with Chronic low back pain and in patients with hemiparetic upper limb post CVA.
- A systematic review of 23 trials considering needling therapies for myofascial trigger point pain concluded that direct dry-needling (where MTrPs were directly targetted) was as benificial as wet needling. There is no clear evidence that it is beneficial above placebo. More studies of higher quality with a reproducible diagnostic criteria and a valid placebo are needed to draw firm conclusions on this.

DRY NEEDLING FOR GLUTAEUS MUSCLES
* A systematic review and meta analysis with level 1a evidence suggests that:
- Very low–quality to moderate quality evidence suggests that dry needling performed by physical therapists is more effective than no treatment, sham dry needling, and other treatments for reducing pain and improving pressure pain threshold in patients presenting with musculoskeletal pain in the immediate to 12-week follow-up period.
- Low-quality evidence suggests superior outcomes with dry needling for functional outcomes when compared to no treatment or sham needling.
- No difference in functional outcomes exists when compared to other physical therapy treatments.
- Evidence of long-term benefit of dry needling is currently lacking.









4 Comments