Fibromyalgia Tender Points: What and Where Are They?
Table of Contents
What Are Fibromyalgia Tender Points?
If you want to know the tender points in fibromyalgia, the number, and locations of tender points when diagnosing patients that helps a lot in the overall planning of the treatment.
The patient with fibromyalgia is normally more concerned about full-body aches and general tenderness than specific tender spots.
- if anyone who suffers from fibromyalgia is that they have a decreased threshold to pain.
- An individual without fibromyalgia could be delicately bumped into and barely mark it. But because a person with fibromyalgia is more sensitive to pain, that same degree of touch could harm a lot more.
- In spite of the fact that fibromyalgia is a condition known for causing widespread pain, therapists used to recognize the specific areas of the body — called tender points — that felt more sensitive to touch to fibromyalgia patients than to a person who does not have these disorder.
- Tender points are specific areas of pain that are near the joints but are not the joints themselves.
- They hurt when someone presses on them. Even firm pressure from a finger — like a poke — can make someone wince or flinch.
- For a point to be scrutinized tender, the spot should create localized pain when the therapist presses on it with their finger.
- The therapist would push with gentle pressure so that their fingernail turns white.
- A point that tested positive for tenderness would be too painful only on the exact spot the doctor presses.
- One of the defining criteria of fibromyalgia is that the pain commonly fluctuates.
- It may come and go, move around, or vary broadly in intensity from day to day.
- On the day that the patient calls their doctor to make an appointment, the patient might have tenderness in all 18 tender points.
- On the day of the appointment itself, the patient can only have tenderness in four of them.
- Over the years, too many people with fibromyalgia have gone asymptomatic because they didn’t have tenderness in 11 spots at the time of their physical exam.
- A tender point diagnostic test is still a helpful guidepost for physicians.
- But enlarging the diagnostic criteria has helped the individual get the right diagnosis.
- Once the patient is diagnosed with fibromyalgia, the doctor will be able to explain to the patient the currently presumed etiology of the pain.
- The patient may then work with their doctor to improve their symptoms.
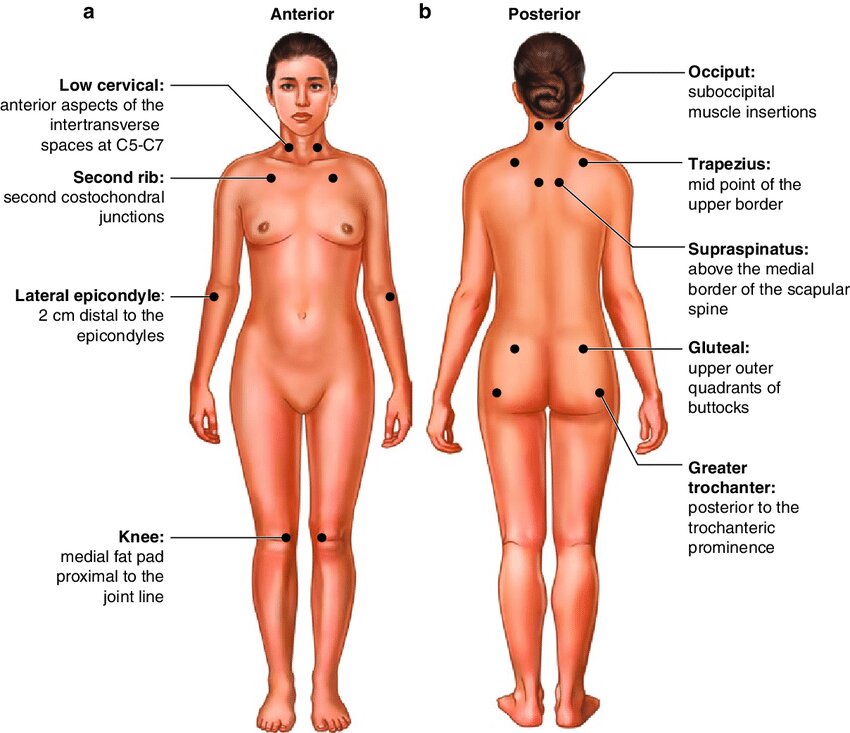
What are the locations of the tender points?
- The 18 tender points connected with fibromyalgia occur in consistent pairs from the back of the head to the inner knees.
- Tender points occur on both the left sides and the right sides of the body at these nine situated:
Occiput:
- Bilateral, at the suboccipital muscle insertions. and the area of the neck muscles attaches to the base of a skull.
Low cervical:
- Bilateral, at the antecedent aspects of an intertransverse space at C5-C7. (Front lower neck).
Trapezius:
- Bilateral sides, at the midpoint of an upper border.
- (Halfway in the middle of the neck and the shoulder).
Supraspinatus:
- Bilateral, at origin, above a scapula spine close by the medial border. (Muscle above an upper inner shoulder blade).
2nd Rib:
- Bilateral or both sides, at the 2nd costochondral junctions, just lateral to the junctions on upper surfaces. (Edge of the upper breast bone).
Lateral epicondyle:
- Bilateral, 2 cm beneath an epicondyle. (2 cm lower the side bone at the elbow).
Gluteal:
Bilateral or both sides, in upper outer quadrants of buttocks in an anterior fold of muscle. (Upper outer buttock).
Greater trochanter:
- Bilateral, posterior to the trochanteric prominence. (Hip bone).
Knee:
- Bilateral or both sides, at a medial fat pad nearest to the joint line. (Just over a knee on the inside).
- Pain in at least eleven of the eighteen tender points is required for an FM( fibromyalgia) diagnosis.
What Causes Tender Points?
- Doctors don’t know what causes these pressure points. But they do know that their locations are not arbitrary.
- They happen in predictable places on the body.
- That means too people with fibromyalgia have common symptoms with their tender points.
TENDER POINT-
What Can Make Tender Point Pain Worse?
- A various number of things may make fibromyalgia symptoms worse. They include:
- Anxiety
- Changes in the environment — for example, cold or humidity
- Depression
- Fatigue
- Hormonal changes, like PMS
- Infections
- Lack of sleep or restless sleep
- Emotional stress
- Physical exhaustion
- Not moving around enough.
Tips for coping with tender points-
- The patient with fibromyalgia is normally more concerned about full-body aches and general tenderness than specific tender spots.
- If the patient has fibromyalgia, they probably think most about the symptoms that interfere with their daily life. This may include:
- Morning stiffness
- Difficulty moving
- Pain during handshakes and hugs
- Painful knots in the muscles.
- Painful knots in the muscles are often myofascial trigger points. Trigger points are hard, knotty lumps that create taut skeletal muscles.
- Unlike tender points, which generate only localized pain, trigger points create both localized and referred pain.
- Referred pain experience like it shoots or radiates to a different part of the body.
- Trigger points are far more common in people with fibromyalgia than they are in the common population.
- Although, anyone may develop them. There is a chronic universal pain condition called myofascial pain syndrome.
- It includes chronic trigger point pain.
- Myofascial pain syndrome may coexist with fibromyalgia.
- In addition, a study published in the journal Pain Trusted Source discovered that much of the neck and shoulder pain that individuals with fibromyalgia experience is caused by trigger points, not tender points.
Treatment for trigger point-
Pain medication-
- A doctor might prescribe over-the-counter (OTC) pain medications, like acetaminophen.
- The Food and Drug Administration (FDA)has also validated several medications to treat other conditions that are also suitable for FM.
- Most medicines change a person’s brain chemistry to help reduce pain levels.
- These medicines involve milnacipran and duloxetine.
- Another medication, pregabalin, blocks nerve cells that play important role in the transmission of pain.
- Some individuals with severe FM pain can become dependent on different types of pain medication.
- For this reason, doctors generally do not recommend narcotic pain medications due to the possibility of dependency.
- Discover the natural pain relief methods here.
Sleep medications-
- A healthcare professional might advocate various OTC and prescription medications to get rid of the sleep-related problems that occur due to FM.
Antidepressants-
- In some cases, a doctor might recommendable antidepressants and antianxiety medications to reduce the anxiety, depression, and sleep symptoms of FM.
Trigger point injections for fibromyalgia-
- Trigger point injections may deactivate a painful trigger point, by giving pain relief in certain areas.
- Trigger point injections should be given by an experienced pain specialist with specialized equipment.
- Injections may include saline, steroids, or local anesthetics like lidocaine.
Acupuncture treatment for fibromyalgia-
- A study in the Journal of Manipulative and Physiological Therapeutics Trusted Source suggested that two different types of massage therapy eventually help females with fibromyalgia.
- Manual lymph drainage therapy is a massage therapy that moves fluid away from areas where lymph vessels are blocked or damaged.
- Connective tissue massage is an intense massage technique, that main focus is on manipulating myofascial tissue.
- Researchers propose that both techniques reduce pain, increase the quality of life, and increase pain thresholds.
- Not all massages are generated equally, so do not anticipate the best results from the local spa.
- The patient might want to start by asking for recommendations from friends, the family physician, or the fibromyalgia specialist.
- For more help finding a well-qualified massage therapist near the area, also check out the American Massage Therapy Association’s directory of certified practitioners.
Effective sleep hygiene-
- Going to bed at the same time each night and waking at the same time every morning may help a person evolve a regular sleep pattern.
- Doctors also advocate avoiding caffeine close to bedtime.
- Taking these steps may decrease the impact of FM on sleep hygiene for some people.
Relaxation techniques-
- It is needful to find ways to relax each day. For example, deep breathing, meditation, and yoga may all be beneficial.
- Relaxing may improve mood, decrease fatigue, and reduce pain.
Getting support-
- Accepting help from family and friends can help, as can seeking professional assistance from a counselor.
- Support groups are also available through organizations like the National Fibromyalgia Association.
Home Remedies for Tender Point Pain–
- How the person handles fibromyalgia pain at home is another essential part of the overall treatment.
- For example, therapeutic massage may manipulate the muscles and soft tissues of the body to help ease pain, muscle tension, spasms, and stress.
- Try putting moist heat on the muscles two times a day to reduce deep muscle pain and stiffness.
- The patient may use a moist heating pad, luck warm bath or shower, or a heat “cozy” that the warm in the microwave.
- It’s also essential to manage the schedule and control stress levels.
- Make sure to block out time each day to rest and relax.
- Try not to make too many commitments that can wear the patient out.
- An individual can also apply relaxation exercises like guided imagery, deep-breathing exercises, or the relaxation response to manage how the patient deal with stress.
- Also, try to go to bed at the same time every night. It allows your body to rest and repair itself.
- And get regular exercise. It will help the patient to manage the pain and other symptoms of fibromyalgia.
FAQ
An individual with fibromyalgia generally feels various types of pain in their bodies. Along with widespread, deep muscle pain, it is normal to feel multiple tender points, too. Tender points are areas of pain surrounding the joints, but may not be in the joints themselves. These places hurt when the therapist press on them.
Learn about medications utilized to treat fibromyalgia symptoms and how they may help decrease pain and fatigue and improve sleep quality. The most useful treatment approach for fibromyalgia is a combination of self-care, physical activity, and cognitive-behavioral therapy. But medication can also be needed.
The 5 Stages of a Fibromyalgia Diagnosis
Stage 1: The Unknown. The patient has a variety of symptoms of widespread, ever-changing pain, often ignored as they struggle through the days, slipping behind the social engagements and housework.
Stage 2: The Aware.
Stage 3: The Flare.
Stage 4: The Roundabout.
Stage 5: Making Peace.
Because fibromyalgia is complex in nature and difficult to identify, a rheumatologist will perform a complete medical history and a full physical exam. A physical exam may help reveal signs of inflammation throughout the body’s joints and musculoskeletal system.
While Multiple sclerosis and fibro can have some symptoms of inequality, they are ultimately distinct conditions with very various causes and treatments. Fibromyalgia and multiple sclerosis are both chronic diseases with no treatment. Fibromyalgia and multiple sclerosis may both cause some of the same symptoms.