Pseudogout
Table of Contents
What is Pseudogout?
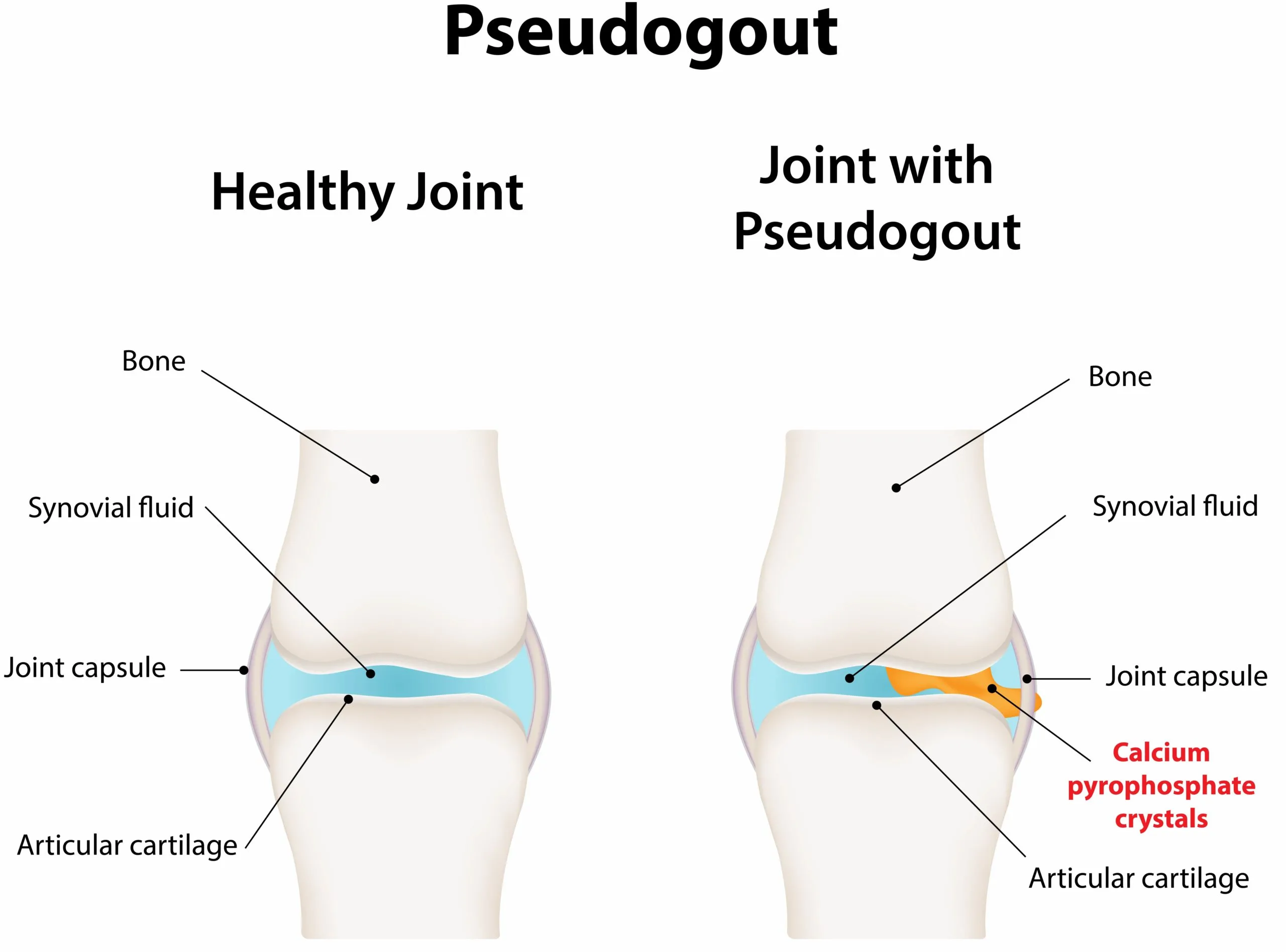
The ‘pseudogout syndrome’ was first explained by Kohn & colleagues in 1962 & accurately depicts acute attacks of synovitis induced by calcium pyrophosphate dihydrate (CPPD) crystals.
Calcium pyrophosphate dihydrate is a type of arthritis that is painful & starts suddenly in one or more of the joints. Episodes can present for days or weeks. some populations use this to refer to calcium pyrophosphate deposition disease (CPPD), which occurs when calcium pyrophosphate crystals form & build up in the joints & surrounding tissues.
The symptoms are the same as the symptoms of other diseases, especially gout which is why this form of arthritis had the name pseudogout – “false gout”. Some symptoms of Calcium pyrophosphate dihydrate disease may appear to be symptoms of rheumatoid arthritis or osteoarthritis.
CPPD commonly affects the knee or wrist joints. Less frequently, it can involve the hips, shoulders, elbows, knuckles, toes, or ankles. Rarely it affects the neck & causes neck, & shoulder pains, headaches, & in some cases fevers. This happens when the calcium crystals deposit around the dens part of the second cervical vertebra. The disease is named crowned dens syndrome.
It occurs when calcium pyrophosphate crystals build up in the joints & the tissues that surround them. This buildup causes symptoms that can seem similar to those of gout. Nevertheless, gout results from a different type of crystal.
The Arthritis Foundation (AF) states that people are more likely to develop CPPD as they age. Nearly half of those above the age of 85 years have developed crystals. Nevertheless, many peoples do not have symptoms.
CPPD deposition might also cause symptoms similar to septic arthritis, polyarticular inflammatory arthritis frequently misdiagnosed as rheumatoid arthritis (RA) or degenerative osteoarthritis (OA).
particular emphasis on the use of available agents to target the ‘inflammasome’, which plays a major role in crystal-induced inflammation, & the theoretical potential of specific anticrystal therapies.
Without treatment, a patient can experience painful & severe attacks or chronic inflammation & pain. Over time, CPPD can lead to joint damage & long-term disability.
Although no treatment is available to dissolve the crystals, a patient can take medications to help treat the symptoms.
What are the symptoms of Pseudogout?
Pseudogout most frequently affects the knees, but it also affects the ankles, wrists, & elbows.
Large joints are more usually affected & the attacks are characterized by the cardinal signs of inflammation which might involve one or several hot, tender, red, & swollen joints. The knee is the most usually involved joint, followed by the wrist, ankle, elbow, toe, shoulder, & hip.
General symptoms might include:
- bouts of joint pain
- swelling of the affected joint
- fluid buildup around the joint
- chronic inflammation
- The swollen joint is warm & tender to the touch
- Red skin involving the affected joint
What are the causes of Pseudogout?
Pseudogout is happen when calcium pyrophosphate crystals form in the synovial fluid in the joints. Crystals can also deposit in the cartilage, where they can lead to damage. The buildup of crystal in the joint fluid results in swollen joints and acute pain.
This condition outcomes from the abnormal production of calcium pyrophosphate dihydrate (CPPD) crystals in the cartilage (cartilage is the “cushion” between the bones) or the joint fluid (synovial fluid). This can cause a sudden attack of arthritis same to gout.
Researchers don’t fully understand why crystals occur. The chance of them occurring likely increases with age. Crystals form in about half of patients over the age of 85, according to the Arthritis Foundation. Nevertheless, many of them don’t have pseudogout.
Pseudogout can frequently run in families, so many healthcare professionals believe it to be a genetic condition. Other contributing factors might include:
- hypothyroidism, or an underactive thyroid
- hyperparathyroidism, or an overactive parathyroid gland
- excess iron in the blood
- hypercalcemia, or much more calcium in the blood
- magnesium deficiency
What is the prevalence of Pseudogout?
Calcium pyrophosphate dihydrate crystal deposition disease affects both men & women. It occurs more often in people as they age, commonly affecting people over age 60.
What are the risk factors of Pseudogout?
Factors that can increase a patient’s risk of pseudogout include:
- Older age. The risk of occurring pseudogout increases with age.
- Joint trauma. Trauma to a joint, such as a severe injury or surgery, elevates the risk of pseudogout in that joint.
- Genetic disorder. In some families, family members have a hereditary tendency to have pseudogout. These patients tend to develop pseudogout at younger ages.
- Mineral imbalances. The risk of pseudogout is higher for patients who have excessive calcium or iron in their blood or too little magnesium.
- A thyroid condition:
- Kidney failure.
- Parathyroid disease.
- Low magnesium.
Other medical conditions. Pseudogout has also been linked to the non-active thyroid gland or an overactive parathyroid gland.
The condition is also usually present in patients who have osteoarthritis/degenerative joint disease. “Attacks” of osteoarthritis associated with pain, swelling, & redness of the joint might, in fact, in certain cases, be because of CPPD.
What are the complications of Pseudogout?
In some cases, the crystal deposits in the synovial fluid can cause permanent joint damage. Joints that have been affected by pseudogout can eventually have cysts or bone spurs, which are growths that stick out on the bones.
The crystal deposits associated with pseudogout can also cause joint damage, which can mimic the signs & symptoms of osteoarthritis or rheumatoid arthritis.
Pseudogout might also result in loss of cartilage.
How to prevent Pseudogout?
While patients can’t prevent the disease, you can find treatments to decrease the inflammation & relieve the pain. Treating the underlying condition that causes pseudogout might slow its development & lessen the severity of symptoms.
What is the diagnostic procedure for Pseudogout?
CPPD can not be diagnosed simply from a blood test. It’s diagnosed by the study of the synovial fluid from the affected inflamed joint, which is observed under a microscope for CPPD crystals.
Fluid is aspirated by a needle from the inflamed joint. This process is called arthrocentesis. Removing the fluid might also help reduce the pressure within the joint, & this can help reduce the pain.
Since different types of crystals in the joint can be the cause of other types of arthritis, it’s important that an accurate diagnosis be made. Then the doctor can prescribe the appropriate treatment.
The American College of Rheumatology describes that CPPD is challenging to diagnose because it is so similar to gout & other types of arthritis.
If the doctor suspects that the patient has pseudogout, they will usually:
- ask about the symptoms, such as when they started & how long they last
- to ask about the patient’s family & medical history
- image the joint utilizing X-rays or ultrasound, CT, or MRI scans
- They might also use a needle to take a small amount of fluid from the affected joint & send it to a laboratory. Technicians will see the presence of calcium pyrophosphate crystals.
The definitive diagnosis of pseudogout is most usually & accurately made by identifying CPPD crystals, by compensated polarized light microscopy, in the SF of affected joints. Furthermore, all patients presenting with suspected CPPD deposition can be screened for chondrocalcinosis using certain key radiographs: a non-weight-bearing anteroposterior (AP) view of both knees, an AP view of the pelvis for visualization of the symphysis pubis & hips, & a posteroanterior (PA) view of each hand to include the triangular ligament of the wrists.
Changes in the metacarpophalangeal joints, such as squaring of the bone ends, presence of subchondral cysts & hook-like osteophytes, are characteristic features of the arthropathy of hemochromatosis, but are also found in patients with CPPD deposition alone. Thus, a probable diagnosis of CPPD arthropathy can be made in patients who present with acute or chronic arthritis of the knee, hip, wrist, shoulder, or metacarpophalangeal joints in the setting of radiographic features, even without the direct demonstration of CPPD crystals by microscopy.
Given the aforementioned disease associations, most patients with CPPD deposition, & particularly those who are relatively young, should undergo screening for abnormal serum calcium, phosphate, magnesium, alkaline phosphatase, & thyroid-stimulating hormone levels, & any evidence of iron overload by haematinic analyses (ferritin, iron saturation and transferrin). This is especially true with regard to hemochromatosis in light of the strong association between this condition & all forms of CPPD-related arthropathy, & the deleterious consequences of delayed diagnosis.
What is the treatment plan for Pseudogout?
Medical treatment for pseudogout:
The treatment of CPPD is the same as the treatment of acute gout attacks with anti-inflammatory medication. Uric acid-lowering drugs are not prescribed. Symptoms are frequently relieved within 24 hours after initiating treatment with anti-inflammatory medications.
The aims of treatment are to relieve pain & inflammation & prevent recurrent attacks that could lead to significant pain & joint damage.
The type of treatment prescribed will depend on several factors, including the person’s age, the type of other medicines they’re taking, overall health, medical history, & the severity of the attack.
Treating associated metabolic conditions:
Decreasing iron overload, treating hypothyroidism -No hard evidence that this improves CPPD-related arthropathy
Magnesium supplementation-Only indicated in hypomagnesemia states. Otherwise, the evidence is largely anecdotal
Anti-inflammatory drugs
Anti-inflammatory drugs are generally continued until the CPPD attack completely resolves. If side effects from the therapy occur, treatment might be changed to a different medicine. The healthcare provider will discuss the definite side effects with the patient.
Colchicine is commonly prescribed for CPPD attacks. At low doses, it can be prescribed for a longer period of time to decrease the risk of recurrent attacks of CPPD.
Nonsteroidal anti-inflammatory drugs (NSAIDs), especially if colchicine cannot be prescribed, are utilized to treat CPPD attacks.
Certain patients cannot take these medications, such as those who have poor kidney function, bleeding disorders, stomach or digestive disease, heart disease, & certain other health complications. Types of NSAIDs involve aspirin, naproxen, & ibuprofen.
Corticosteroids (also called steroids) might be prescribed for people who cannot take NSAIDs or colchicine. Steroids also work by decreasing inflammation. Steroids can be injected into the affected joint or they can be given as pills.
Anticrystal agents
- Probenecid-Good theoretical rationale but the evidence is lacking
- Phosphocitrate-Strong evidence from animal studies but no safety or efficacy data for humans
Unlike gout, there are no available agents which directly attack crystal load in CPPD deposition disease. Probenecid is a transmembrane-transport inhibitor that reduces the production of extracellular PPi in vitro, but to date has never been demonstrated to decrease CPPD crystal deposition in humans. The clear contribution of CPPD crystals to the acceleration of joint degeneration in the various CPPD-related arthropathies & the possible pathological role of these crystals in osteoarthritis has resulted in significant interest in the potential of phospho-citrate to directly target crystal deposition in both of these diseases.
Calcification of articular cartilage is now well recognized as an indissociable sign of osteoarthritis. Furthermore, there is strong in vitro proof that such calcium deposition is inhibited by phospho-citrate. Taken together with previous work demonstrating that CPPD crystals accelerate joint degeneration in a rabbit model of osteoarthritis, this suggests that agents which directly target articular calcification might not only have the potential to manage CPPD-related arthropathy but also osteoarthritis itself.
Targeting the inflammasome
- Methotrexate -has an emerging role in the prevention of recurrent attacks
- Inhibition of IL-1 pathway (anakinra, canakinumab, IL-1 Trap) -Might become key agents for refractory polyarticular condition
- Anti-TNFα drugs-has poor efficacy in auto-inflammatory conditions & therefore unlikely to be successful in pseudogout
Alongside the recent advances in the understanding of the mechanisms included in crystal-induced joint inflammation, specific attention has been focused on the ability of methotrexate to decrease the frequency & intensity of recurrent attacks of pseudogout, particularly in relation to polyarticular condition.
Despite the fact that this agent is relatively contraindicated in patients with hemochromatosis-associated arthropathy, because of its broad-spectrum ability to inhibit most cytokine pathways involved in joint inflammation, this generally well-tolerated molecule represents an attractive alternative in the treatment & prophylaxis of the entire spectrum of ‘pseudogout syndrome’.
The anti-inflammatory effect of methotrexate is mediated chiefly by an increase in extracellular adenosine levels, which activates membrane receptors on macrophages & other inflammatory cells, thereby inhibiting the release of several cytokines, most notably IL-1β. Thus, by acting in this proximal manner, methotrexate has a potent indirect effect on the ability of the inflammasome to produce IL-1β. Multicentre clinical trials are currently underway to further evaluate the potential impact of this widely available & affordable medication in this region.
Specific insights into the role of IL-1β in a variety of auto-inflammatory conditions have resulted in a number of case reports documenting the efficacy of anakinra, an IL-1 receptor antagonist, in difficult-to-manage polyarticular pseudogout.
Although several reports exist of gout being successfully managed with anti-TNFα drugs, published cases of pseudogout successfully treated with these agents are lacking. As with many auto-inflammatory conditions, it seems that CPPD-related arthritis responds not good to this class of medication. To date, the experimental data indicating that TNFα, unlike in rheumatoid arthritis, appears to exert its influence downstream of IL-1β in the acute inflammatory cascade associated with pseudogout would seem to be borne out clinically.
Certain medications, such as anakinra & canakinumab, have been shown to be beneficial in the treatment of acute attacks. Nevertheless, as of 2020, these have not yet been approved by the FDA.
Side effects of medicines:
Not all patients have occurred side effects from these medicines. How frequently any side effects vary from patient to patient. The occurrence of side effects depends on the dose, type of medicine, length of treatment, concurrent illnesses, & other medications the patient might be taking.
Some side effects are more severe than others. Before any medicine is prescribed, the healthcare provider will discuss with you the potential benefits & risks of taking the medication.
Surgery
If joints are wearing out, the doctor might recommend surgery to repair or replace them.
Physical therapy treatment for Pseudogout:
During acute exacerbations, the physical therapist should focus on reinforcement of the management program & splinting orthotics, or other assistive devices to protect the affected joint. An ice pack can be given to the affected joint.
Pain management modalities can include:
- Cryotherapy
- Ultrasound therapy
- Transcutaneous electrical nerve supply (TENS)
During inter-critical phases, physical therapists might offer assistance with the maintenance of a range of motion, strength, & function by giving strengthening and stretching exercises. The physical therapist can also assist the patient in keeping a suitable exercise routine & keeping their weight under control.
Home management for Pseudogout:
There is no cure for CPPD. Researchers are yet to discover a way to prevent the crystals that cause the disease.
Instead, patients can work with healthcare professionals to decrease the frequency of attacks & ease the symptoms.
If an attack occurs, the patient tries the following for symptom relief:
- resting the affected joint or joints
- Apply a towel-wrapped ice pack or Hot pack to the affected joint.
- Take nonsteroidal anti-inflammatory drugs, such as ibuprofen, indomethacin, or naproxen
- Patients who have bad kidney function, take blood thinners, or have a history of stomach ulcers are unable to take NSAIDs. In these cases, the healthcare professional might drain the joint fluid & inject a corticosteroid.
Additionally, the AF notes that some foods can help fight against inflammation. The patient can try including plenty of the following foods in the diet:
- Fruit: Good options include cherries, strawberries, raspberries, & citrus fruits.
- Fish: The patient can try eating salmon, herring, tuna, sardines, scallops, & anchovies.
- Nuts: The AF particularly recommends walnuts, pine nuts, almonds, & pistachios.
- Beans: Kidney beans & pinto beans are particularly rich in antioxidants.
- Olive oil: The patient should aim for 2–3 tablespoons daily.
- Whole grains: These include oatmeal, brown rice, & quinoa.
- Nightshade vegetables: Examples include eggplant, potatoes, tomatoes, & red bell peppers. Some patients believe that these foods trigger arthritis flares, so it is best to monitor symptoms when eating them.
The patient should avoid processed foods & those high in saturated fats.
What is the outlook for Pseudogout?
Deposits of CPPD crystals occur over a long duration of time. Like gout, CPPD attacks can reoccur from time to time in the same joint or different joints. The starting attack might last a week to two weeks unless it’s managed.
Over time, CPPD attacks might occur more often, involve more joints, have more severe symptoms, & last longer. The frequency of attacks varies. Attacks might occur from once every few weeks to less than once a year. Nevertheless, frequent, repeated attacks can damage the joints.
Pseudogout & the associated CPPD-related arthropathies are likely to increase in prevalence because of the demographic drift toward an aging population. Thus, the management of these diseases will continue to present particular challenges in the future. The usage of regular colchicine as a prophylactic agent against acute attacks of pseudogout will probably become more widespread. Similarly, drugs targeting the IL-1 pathway offer considerable potential in severe refractory conditions. Nevertheless, in contrast to MSU crystals in gout, there is no practical way to remove CPPD crystals from the joint. Therefore, current management strategies stay symptomatic but not disease-modifying. Further research into ways of decreasing the CPPD crystal burden is very necessary.
There is no cure for CPPD, but patients can manage the condition using medications & lifestyle adjustments.
Nevertheless, over time, the calcium pyrophosphate crystals can cause more damage to the joint. In some cases, this damage can outcome in disability.
FAQ (frequently asked questions)
Gout & pseudogout, while both joint problems caused by crystals are caused by different types of crystals. Gout is caused by sodium urate crystals & pseudogout is caused by calcium pyrophosphate crystals. Gout takes place when high levels of uric acid cause monosodium urate crystals to form in & around the joint. This leads to damage to the joints & inflammation. CPPD takes place when calcium pyrophosphate crystals form & build up in the joints & surrounding tissues, resulting in pain & inflammation.
Pseudogout or false gout is a form of arthritis that results from deposits of calcium pyrophosphate crystals its medical term is calcium pyrophosphate dihydrate crystal deposition disease CPPD. It commonly affects the knees & wrists.
Pseudogout occurs when deposits of calcium pyrophosphate crystals accumulate in a joint. Initially, crystals deposit in the cartilage & can cause damage. They also can cause a reaction with inflammation that leads to joint pain & swelling. This can cause more chronic arthritis that mimics osteoarthritis or rheumatoid arthritis.
To cope with pseudogout recommend changing the patient’s diet to eliminate foods that favor inflammation. These include polyunsaturated vegetable oils, & all sources of trans-fatty acids, such as margarine & partially hydrogenated vegetable oils.
It is safe for the patient to walk with pseudogout. In fact, doing a joint-friendly activity such as walking can help improve gout-related pain. Gout is a type of arthritis that commonly affects the big toe joint, but it can also affect the lesser toes, ankles, & knees.
It can take up to 2 years for crystals to be completely clear out from the body, so the patient might continue to have attacks during this time.