Knee joint with Ligaments
Table of Contents
Introduction
- The knee joint is a modified hinge joint, the type of synovial joint, that is composed of three functional compartments: the patellofemoral articulation, consisting of the patella, or even “kneecap”, as well as the patellar groove on the front of the femur through which it slides; and the medial as well as lateral tibiofemoral articulations linking the femur, or even thigh bone, with the tibia, the main bone of a lower leg.
- The joint is bathed in synovial fluid inside the synovial membrane called the joint capsule. The posterolateral corner of the knee is an area that has recently been a subject of renewed scrutiny & research.
- The knee is the largest joint as well as one of the most essential joints in a body. it plays the important role in motions related to carrying a body weight in horizontal (running as well as walking) and vertical (jumping) directions.
- At birth, the kneecap is just formed from cartilage, as well as this will ossify (change to bone) between the ages of three to five years. Owing to it being the largest sesamoid bone in the human body, the ossification process takes significantly longer.
What do the knee joint ligaments?
- The knee ligaments have several important works, which are described in detail:
- Absorb shock when the foot strikes the surface.
- Connect a thigh bone to the lower leg bones.
- Keep the bones in a proper position.
- Prevent a knee from twisting or even collapsing.
- Stabilize a knee joint.
- Stop a knee from moving in any unsafe or even unnatural directions.
What are knee joint ligaments made of?
- Most of the ligaments are made of:
- Collagen is the protein that binds tissues in animals.
- Connective tissue.
- Elastic fibers are slightly stretchy.
What are the ligaments of the knee joint?
- Ligaments are elastic bands of tissue that connect bones as well as provide stability & strength to the knee joint.
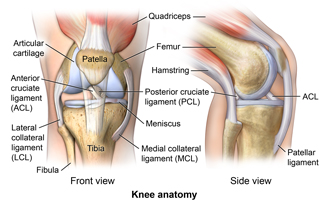
- There are mainly two types of ligaments in the knee:
- Collateral ligaments: The two collateral ligaments are like straps on each side of the knee. A medial collateral ligament (MCL) is on the inner side of the knee, which attaches a thigh bone (femur) to the shin bone (tibia). A lateral collateral ligament (LCL) is on the outer side of the knee. It connects the femur to the calf bone (fibula). The collateral ligaments prevent a knee from moving side to side too much.
- Cruciate ligaments: The two cruciate ligaments are inside the knee joint as well as connect the femur to the tibia. They cross each other to create. An anterior cruciate ligament (ACL) is located toward the front of the knee. A posterior cruciate ligament (PCL) is behind the anterior cruciate ligament. The cruciate ligaments control the way the knee moves front to back.
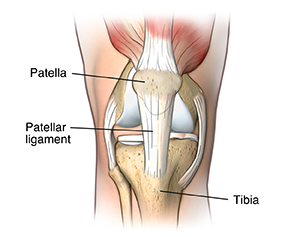
Patellar ligament
- A patellar ligament is the strong, thick fibrous band that is the distal continuation of the quadriceps femoris tendon. This is found superficial/anterior to an infrapatellar bursa as well as extends from an apex of the patella to a tibial tuberosity.
- Along its outer margins, a patellar ligament blends with a medial as well as lateral patellar retinacula, which are extensions of a vastus medialis as well as lateralis muscles, respectively, & the overlying fascia. A patellar ligament plays a major role in stabilizing a patella & preventing its displacement.
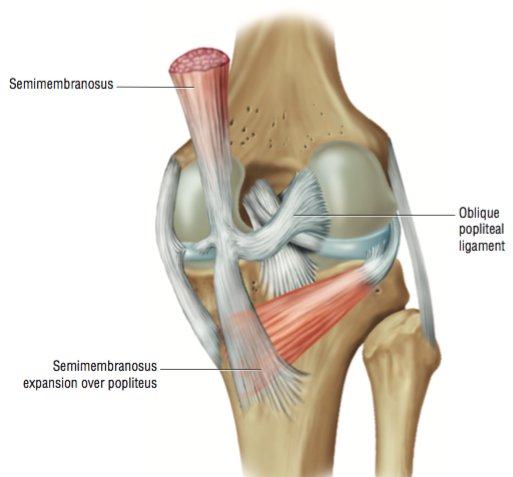
Oblique popliteal ligament
- An oblique popliteal ligament (Bourgery ligament) is the expansion of a semimembranosus tendon that originates posterior to a medial tibial condyle as well as reflects superiorly & laterally to attach on a lateral condyle of a femur.
- As it spans an intercondylar fossa, an oblique popliteal ligament reinforces a posterior part of the knee joint capsule & blends with its central portion.
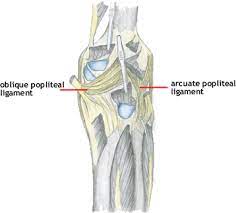
Arcuate popliteal ligament
- The arcuate popliteal ligament is the thick, fibrous band that arises on a posterior aspect of a fibular head as well as arches superiorly & medially to attach on a posterior side of the knee joint capsule of a knee. An arcuate popliteal ligament reinforces a posterolateral part of the knee joint capsule, & together with an oblique popliteal ligament, prevents overextension of a knee joint.
Anterior cruciate ligament
Introduction:
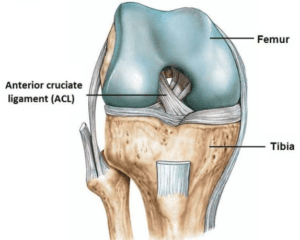
- An anterior cruciate ligament (ACL) is the band of dense connective tissue which courses from a femur to a tibia. The anterior cruciate ligament is a key structure in a knee joint, as it resists anterior tibial translation as well as rotational loads.
Origin:
- Arises from a posteromedial corner of the medial aspect of the lateral femoral condyle in an intercondylar notch. This femoral attachment of the anterior cruciate ligament is on the posterior part of the medial surface of the lateral condyle well posterior to the longitudinal axis of a femoral shaft.
- An attachment is the interdigitation of collagen fibers as well as rigid bone through the transitional zone of fibrocartilage and mineralized fibrocartilage as well.
Orientation:
This runs inferiorly, medially as well as anteriorly.
Insertion:
- Anterior to an intercondyloid eminence of a tibia, being blended with an anterior horn of a medial meniscus.
- A tibial attachment is in the fossa in front of & lateral to the anterior spine, rather than a wide area from 11 mm in width to 17 mm in the anterior-posterior direction.
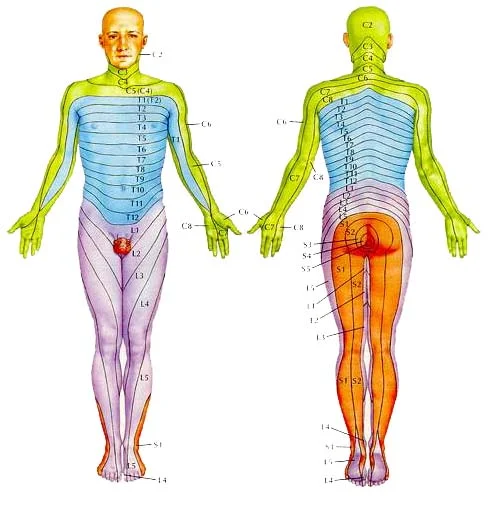
Nerve Supply:
- An anterior cruciate ligament receives nerve fibers from posterior articular branches of a tibial nerve. These fibers penetrate a posterior joint capsule as well as run along with synovial & periligamentous vessels surrounding a ligament to reach as far anterior to an infrapatellar fat pad.
- Most of the fibers are associated with an endoligamentous vasculature & have a vasomotor function. The receptors of the nerve fibers mentioned are as below:
- Ruffini receptors are sensitive to stretching & are located in the area of a ligament, predominantly on a femoral portion where the deformations are the greatest.
- Vater–Pacini receptors are sensitive to rapid motions & are located at the femoral as well as tibial ends of the anterior crucial ligament.
Golgi-like tension receptors are located near the attachments of an anterior crucial ligament and at its surface, beneath the synovial membrane.
Free-nerve endings function as nociceptors, but they can also serve as local effectors by releasing neuropeptides along with vasoactive function. Therefore, they can have a modulatory effect on normal tissue homeostasis or in the late remodeling of the grafts. - The mechanoreceptors cited above (Ruffini, Pacini, as well as Golgi-like receptors) have the proprioceptive function as well as provide the afferent arc for signaling knee postural changes.
- Deformations within a ligament influence the output of muscle spindles through a fusimotor system. Thus, activation of afferent nerve fibers in a proximal part of the anterior cruciate ligament influences motor activity in the muscles around a knee; the phenomenon is called ‘‘ACL reflex.’’
- These muscular responses are elicited by the stimulation of group II or III fibers (for instancemechanoreceptors). An anterior cruciate ligament reflex is the essential part of normal knee function & is involved in the updating of muscle programs.
- It becomes even more obvious in patients with the anterior cruciate ligament injury, where a loss of feedback from mechanoreceptors in an ACL leads to quadriceps femoris weakness. Indeed, the afferent feedback from an ACL has a major influence on a maximal voluntary contraction exertion of a quadriceps femoris.
Vascular Supply:
- The major blood supply of the cruciate ligaments arises from a middle geniculate artery. A distal part of both cruciate ligaments is vascularized by the branches of a lateral as well as a medial inferior geniculate artery.
- A ligament is surrounded by the synovial fold where the terminal branches of the middle, as well as inferior arteries, form the periligamentous network. From a synovial sheath, blood vessels penetrate a ligament in the horizontal direction & anastomose with the longitudinally orientated intraligamentous vascular network.
- The density of the blood vessels within the ligaments is not homogeneous. In the anterior cruciate ligament, the avascular zone is located within the fibrocartilage of an anterior part where a ligament faces an anterior rim of an intercondylar fossa.
- A coincidence of poor vascularity & the presence of fibrocartilage is also seen in gliding tendons in parts that are subjected to compressive loads, as well as the coincidence of these two factors undoubtedly plays a major role in the poor healing potential of the ACL.
Composition:
- An anterior cruciate ligament has the microstructure of collagen bundles of multiple types (mostly type I) as well as a matrix made of the network of proteins, glycoproteins, elastic systems, & glycosaminoglycans with multiple functional interactions.
Bundles:
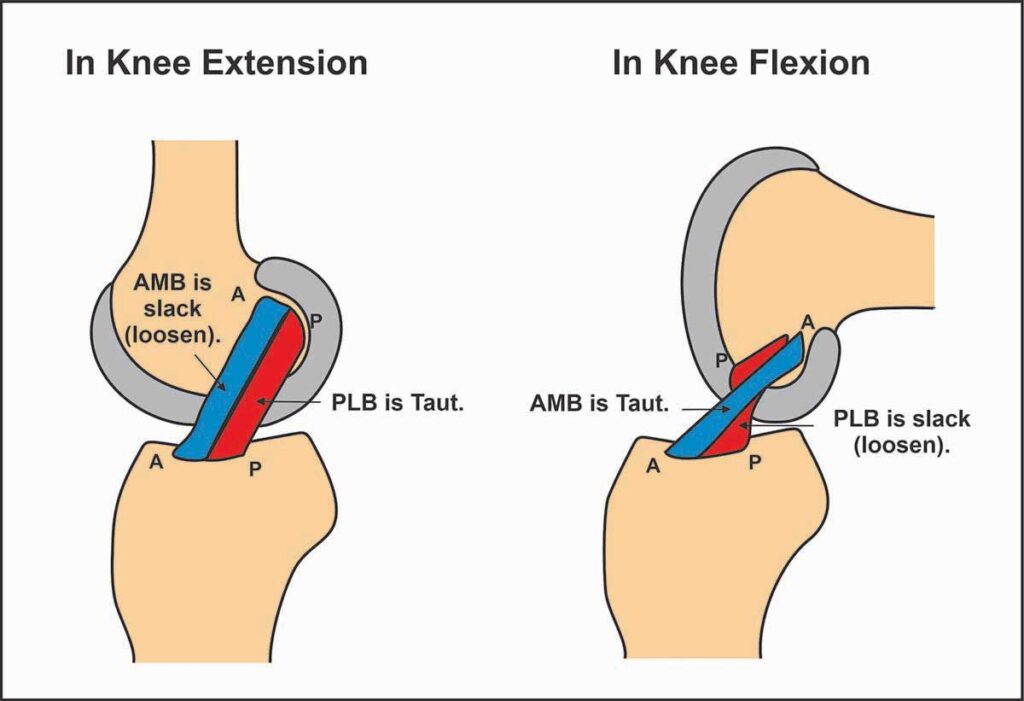
- There are two components of the anterior cruciate ligament, the smaller anteromedial bundle (AMB) & the larger posterolateral bundle (PLB), named according to where the bundles insert into a tibial plateau.
- An anteromedial bundle is tight in flexion & a posterolateral bundle is tight in extension. In extension both bundles are parallel; in flexion, a femoral insertion site of a posterolateral bundle moves anteriorly, both bundles are crossed, an anteromedial bundle tightens as well as a posterolateral bundle loosens.
- With a knee extended, resistance to the anterior translation of a tibia, Lachman’s Test, is by a bulky posterolateral bundle. With a knee flexed, resistance to the anterior translation of a tibia is by an anterior medial bundle.
- Rupture of the posterolateral bundle causes an increase in the hyperextension, anterior translation (extended knee), enhancement in external as well as internal rotation (knee extended), & increases in external rotation with a knee in mid flexion; Rupture of an anteromedial bundle causes anterolateral instability with the increase in anterior translation in flexion, minimal increase in hyperextension, as well as minimal rotational instability.
Function:
- The anterior cruciate ligament provides approximately 85% of the total restraining force of the anterior translation. It also prevents excessive tibial medial as well as lateral rotation, and varus & valgus stresses.
- To a lesser degree, the anterior cruciate ligament checks extension as well as hyperextension. Together with a posterior cruciate ligament (PCL), the ACL guides the instantaneous center of rotation of a knee, thus controlling joint kinematics. While an anteromedial bundle is a primary restraint against anterior tibial translation, a posterolateral bundle tends to stabilize a knee near full extension, particularly against rotatory loads.
Anterior Cruciate Ligament (ACL) Structure as well as Biomechanical Properties
Introduction
- An Anterior Cruciate Ligament (ACL) is a key structure in a knee joint, as it resists anterior tibial translation as well as rotational loads. It is one of the most frequently injured structures while high-impact or even sporting activities. An anterior cruciate ligament does not heal when torn, & surgical reconstruction is a standard treatment in the field of sports medicine.
- Such reconstruction goals at restoring kinematics as well as stability of an injured knee, to prevent future degenerative changes. Hence, an adequate understanding of the complex anatomy, function, as well as biomechanics of the anterior cruciate ligament is critical to elucidate the mechanisms of injury, and understand the fate of chronic anterior cruciate ligament deficiency, & to increase surgical reconstruction.
Development of the anterior cruciate ligament
- The knee originates from vascular femoral as well as tibial mesenchyme in the fourth week of gestation between a blastoma of the femur and tibia as well.
- By nine weeks, the Cruciate ligaments are composed of numerous immature fibroblasts having scanty cytoplasm & fusiform nuclei.
- After week 20, the remaining development consists of marked growth along with little change in form. At these stages, two main bundles are already detectable, but the bundles seemed more parallel when compared to a bundle orientation of an adult anterior cruciate ligament.
- It is surrounded by the mesentery-like fold of the synovium that originates from a posterior capsular apparatus of the knee joint. Hence, while the anterior cruciate ligament is located intra-articularly, it remains extra-synovial throughout its course.
- An early manifestation of an anterior cruciate ligament with two different bundles in the fetal knee suggests early development of a knee joint is guided by the ACL.
- Cruciate ligaments present at an early stage of development could lead to an assumption that they interact with the resulting shape of femoral condyles as well as the tibial plateau.
Anatomy
Femoral Attachment
- The anterior cruciate ligament is a band-like structure of dense connective tissues. The anterior cruciate ligament is attached to the fossa on a posterior aspect of a medial surface of a lateral femoral condyle. A femoral attachment is in a form of the segment of the circle, with its anterior border straight as well as its posterior border convex.
- Its long axis is tilted slightly forward from a vertical, & the posterior convexity is parallel to a posterior articular margin of a lateral femoral condyle. From its femoral attachment, the anterior cruciate ligament runs anteriorly, medially, as well as distally to the tibia. Its length ranges from 22 to 41 mm (mean, 32 mm) & its width from 7 to 12 mm.
Tibial Attachment
- The anterior cruciate ligament is attached to the fossa in front of & lateral to an anterior tibial spine. At this attachment, the anterior cruciate ligament passes beneath a transverse meniscal ligament.
- A few fascicles of the anterior cruciate ligament can blend with an anterior attachment of the lateral meniscus. In some instances, fascicles from the posterior aspect of a tibial attachment of the anterior cruciate ligament may extend to, as well as blend with, a posterior attachment of the lateral meniscus.
- A tibial attachment of an anterior cruciate ligament is somewhat wider as well as stronger than a femoral attachment. A cross-sectional area increases from a femur to a tibia, as follows: 34 mm2 proximally, 33 mm2 mid-proximally, 35 mm2 at mid-substance level, 38 mm2 mid-distally, as well as 42 mm2 distally. They also reported that a tibial insertion of the anterior cruciate ligament is approximately 120% of the femoral insertion site.
Spatial Orientation
- Literature becomes confusing when fascicular anatomy is categorized. Welsh (1980), as well as Arnoczky (1983), described the ACL as being the single broad continuum of fascicles, along with different portions taut throughout a range of motion. However functionally,
- Girgis divided the anterior cruciate ligament into two parts, an anteromedial bundle (AMB) as well as a posterolateral bundle (PLB), while other authors have separated the anterior cruciate ligament into three functional bundles (AMB, intermediate band, as well as PLB).
- The anterior cruciate ligament courses anteriorly, medially, as well as distally across a joint as it passes from a femur to a tibia. As it does, it turns on itself in a slight outward (lateral) spiral. This is because of the orientation of its bony attachments.
- An orientation of a femoral attachment of an anterior cruciate ligament, about a joint position (flexion/extension), is also responsible for a relative tension of a ligament throughout the range of motion. The attachment of the anterior cruciate ligament is the collection of individual fascicles that fan out over the broad flattened area. These fascicles have been summarily divided into 2 groups:
- Anteromedial band (AMB)
Attachment: Originating at a proximal aspect of a femoral attachment & inserting at an anteromedial aspect of a tibial
attachment
Orientation: In the frontal plane, the anteromedial band has a more vertical orientation (approximately 70° to a knee baseline).
The anteromedial band is moderately lax at an extended knee as well as tight at flexion.
Functional at flexion. - Posterolateral bulk (PLB)
Attachment: Inserted at a posterolateral aspect of a tibial attachment.
Orientation: Posterolateral bulk is oriented more horizontally (approximately 55° to a knee baseline), posterolateral bulk is tight at an extended knee as well as lax at flexion.
Functional at extension. - Internal rotation lengthens the anterior cruciate ligament a little more than does external rotation, most noticeably at 30° of the flexion. In addition, Markolf et al. reported that the anterior cruciate ligament acts as a secondary restraint to varus-valgus angulation at the full extension. Twisting is resisted by the combination of the capsular shearing, slanting collateral ligament action, joint surface, as well as meniscal geometry, while a cruciate play only a secondary role.
- While the two-group designation provides the general idea as to the dynamics of an anterior cruciate ligament through a range of motion, it oversimplifies somewhat, different portion of the anterior cruciate ligament is taut throughout a range of motion. It is of great clinical importance due to, in any position of a knee, the portion of the anterior cruciate ligament remains under tension as well as functional.
- Recently, the classification of intra-articular rupture pattern of an anterior cruciate ligament with regards to its two bundles. This classification consists of the alphanumeric code with letters for a location of an AM bundle rupture as well as numbers for the location of the PL bundle rupture. Femoral rupture location for an AM bundle is graded 1, mid-substance rupture is graded 2 & the tibial rupture of an AM bundle is graded 3. The elongated, functional insufficient AM bundle is graded 4 & the intact AM bundle 5.
- For the APL bundle, the rupture at a femoral origin, a mid-substance or a tibial insertion is graded A, B, and C as well, respectively. Elongated PL bundles are graded as D & intact PL bundles as E. An intra-operatively assessed rupture pattern of an AM & PL bundle may be expressed using this alphanumeric code; for example, 1A for the femoral rupture of an AM & the femoral rupture of a PL bundle.
- The validity, as well as reliability of the possible classification, are currently in development.
Biomechanics
- The fiber bundles of an anterior cruciate ligament do not function as the simple band of fibers with constant tension; in fact, they show different tensioning patterns throughout the full range of motion.
- Differentiation of an anterior cruciate ligament into two functional bundles, an anteromedial bundle (AMB) as well as a posterolateral bundle (PLB), seems the oversimplification, but a two-bundle description of the fibers of an anterior cruciate ligament has widely been accepted as the basis for understanding the function of the anterior cruciate ligament. The terminology of the bundles was chosen according to their tibial insertion with the fibers of an AMB originating in the most proximal part of a femoral origin of the AMB & inserting at an anteromedial tibial insertion.
- The forces taken up by a PLB are higher in lower flexion degrees when compared to an AMB. An AMB, however, was shown to take up more of an applied external force in higher flexion angles. Using the liquid metal strain gauge, Bach et al. reported a higher strain in a PLB than in the AMB in knee flexion below 200.
Coronary Ligaments
Description
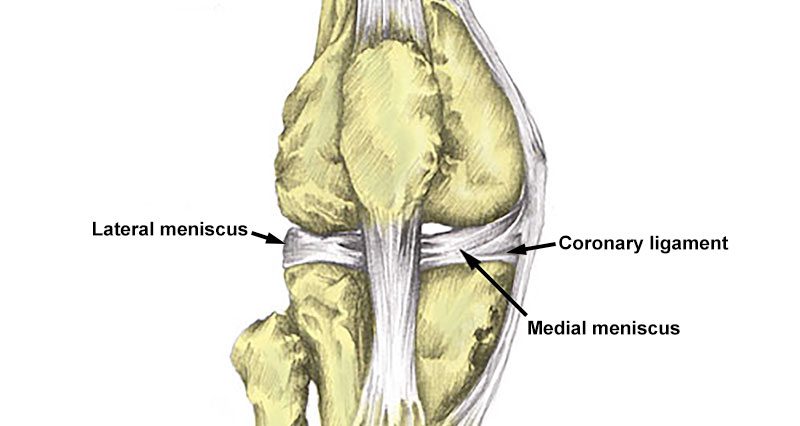
- The Coronary ligaments of a knee or even meniscotibial ligaments are part of a fibrous capsule of a knee joint. There are two coronary ligaments like medial coronary ligament as well as lateral coronary ligament. They connect inferior edges of a meniscus to a periphery of the tibial plateaus.
- A meniscotibial ligament solidly anchors a posterior horn of the medial meniscus.
- A meniscotibial ligament is thicker as well as shorter. This travels from a medial meniscus to a distal edge of the articular cartilage of a medial tibial plateau. The lateral meniscotibial ligament attaches to the lateral face of the lateral meniscus and descended oblique dorsally to reach a superolateral margin of a lateral tibial condyle.
Function
- The coronary ligaments function to stabilize menisci as well as limit rotation of a knee.
Clinical relevance
- Meniscotibial ligament strain is a common cause of knee pain in middle-aged sportspeople. Coronary ligament injuries can happen either as the rupture in its mid-substance or as avulsion. In the study by Peltier et al, they concluded that lesions of a meniscotibial ligament can increase rotatory instability of a knee. Injury to a meniscotibial ligament attachment of a posterior horn of the medial meniscus is suggested by recent literature to be associated with the ramp lesions.
- Ramp lesions are reported to enhance forces on an anterior cruciate ligament.
Lateral Collateral Ligament
Description
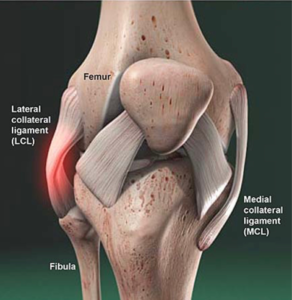
- A fibular or even lateral collateral ligament (LCL) is the cord-like band & acts as a primary varus stabilizer of a knee. It is one of four critical ligaments involved in stabilizing a knee joint.
Anatomy
- Origin: Lateral epicondyle of a femur bone.
- Insertion: Fibula head
- At a proximal level, this ligament is closely related to the knee joint capsule, without having direct contact, as it is separated by a fat pad, An insertion is augmented by an iliotibial band. A popliteus tendon is deep to a lateral collateral ligament, separating it from a lateral meniscus. The lateral collateral ligament further splits the biceps femoris into two parts.
Function
- The lateral collateral ligament stabilizes a lateral side of a knee joint, mainly in varus stress & posterolateral rotation of a tibia relative to a femur. The lateral collateral ligament acts as a secondary stabilizer to the anterior as well as posterior tibial translation when the cruciate ligaments are torn.
- This is the primary restraint to varus rotation from 0-30° of the knee flexion. As a knee goes into flexion, the lateral collateral ligament loses its significance & influence as the varus-stabilizing structure. When a knee is extended, the lateral collateral ligament is stretched.
Clinical relevance
- The incidence of lateral collateral ligament injuries is relatively low (6%) when compared to other knee injuries. This is commonly associated with other knee ligament injuries, hence lateral collateral ligament tear may be easily overlooked as a result of that.
Medial Collateral Ligament of the Knee joint
Description
- A medial collateral ligament (MCL) is the flat band of connective tissue that runs from a medial epicondyle of a femur to a medial condyle of a tibia & is one of four major ligaments that supports the knee joint. Medial collateral ligament injuries often happen in sports, being the most common ligamentous injury of the knee joint, as well as 60% of skiing knee injuries involving the medial collateral ligament.
- The medial collateral ligament is also known as a tibial collateral ligament. The medial collateral ligament provides valgus stability to a knee joint.
- This is strong broadband found on an inner aspect of a knee joint & is the largest structure situated on the medial side. The most common ligament injury of the knee joint. This structure is divided into superficial as well as deep ligaments.
- A superficial ligament is also known as a tibiofemoral ligament. A deep ligament is identified as a mid-third capsular ligament.
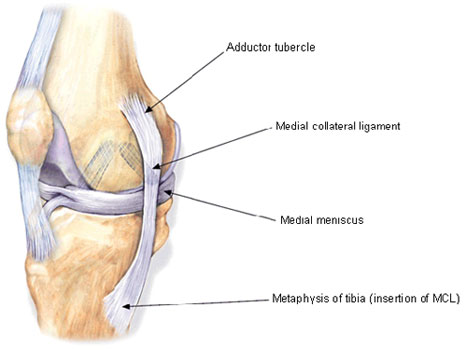
Attachments
- A superficial medial collateral ligament (MCL) has one femoral as well as two tibial attachments.
A femoral attachment is situated on a medial epicondyle. - A proximal attachment blends into the semimembranosus tendon as well as distal attachment is at a posteromedial crest of the tibia.
- A Deep medial ligament (deep MCL) is divided into two, meniscofemoral as well as meniscotibial ligaments. An origin of a meniscofemoral comes from a femur just distal to superficial medial collateral, inserting into a medial meniscus. A meniscotibial ligament is thicker as well as shorter. It travels from a medial meniscus to a distal edge of the articular cartilage of a medial tibial plateau.
Function
- A medial collateral ligament is recognized as being the primary static stabilizer of the knee joint & helps in passively stabilizing the knee joint.
- Superficial, as well as deep ligaments each, have a unique function, making the medial collateral ligament the primary responder to valgus stress & a secondary restraint to rotational forces.
- The MCL, specifically a proximal division, resists valgus forces through all degrees of knee flexion. A distal division of an MCL assists stabilize the external rotation of a knee joint at 30-degree flexion.
- The Deep MCL assists stabilize the internal rotation of a knee joint from full extension through 90-degree flexion (helps a knee in rotational stability primarily in extension moving through into early flexion). In spite of the relationship of a deep MCL with a medial meniscus, there is no influence of a medial collateral ligament on the stability of a medial meniscus.
- Together, the medial collateral ligament also assists guide a knee joint through its full range of motion when the tensile load is applied.
- With low load, a ligament is relatively compliant; with enhancing load, a ligament responds with increasing stiffness until it is nearly linear. Beyond this, the medial collateral ligament will continue to absorb energy until failure.
- The medial collateral ligament also prevents hyperextension of the knee joint & posterior translation of a tibia, secondary to a function of a posterior cruciate ligament (PCL). A posterior oblique ligament, the continuum of oblique fibers at a posterior aspect of the medial collateral ligament is responsible for the function.
- A ligament also plays the role in knee joint position sense or even proprioceptive feedback. When the medial collateral ligament is stretched beyond its ability or even exposed to an excessive load, it evokes neurological feedback signals that then generate a muscle contraction.
Blood Supply
- Branches of superior as well as inferior genicular arteries supply the medial collateral ligament. An area near a bony insertion is more richly vascularized.
Nerves
- The medial collateral ligament is innervated by a medial articular nerve, the branch of a saphenous nerve.
- Innervation is greatest in an epiligament & near the insertions. A ligament may perceive pain & process proprioception through specialized sensory mechanoreceptors like Ruffini endings, Pacinian corpuscles, Golgi receptors, as well as bare nerve endings. Complete medial collateral ligament tears will completely disrupt the pattern of innervation.
Clinical Relevance
- The medial collateral ligament is one of the most commonly injured ligaments of a knee joint. Valgus stress is the most common mechanism of the injury.
- Injuries may be contacted (the direct blow to an outer aspect of a lower thigh or even upper leg) or non-contact (common in skiing). Contact injuries are mostly more severe. Injuries to a medial collateral ligament may have detrimental effects on surrounding structures.
- This is recognized that either partial or even complete ruptures in a ligament significantly increase the load on the anterior cruciate ligament.
- Partial tears show that increases in anterior cruciate ligament load were identified at 30-degree knee flexion & valgus load & internal torque.
- A medial meniscus is often also injured because of its relationship with the deep MCL.

Medial Patellofemoral Ligament (MPFL)
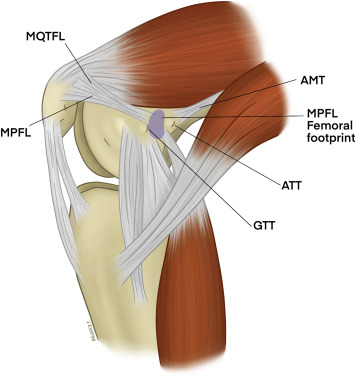
Description
- A Medial Patellofemoral Ligament (MPFL) is the hour-glass-shaped ligament made of bands of retinacular tissue. The medial patellofemoral ligament plays a significant role in the stabilization of a medial aspect of the patella. Especially while the early stages of knee flexion, the medial patellofemoral ligament is a critical component in patellar tracking as well as stability within the trochlear groove.
Attachments
- A medial patellofemoral ligament is located in the second layer of three soft tissue layers within a medial aspect of the knee joint. A medial patellofemoral ligament originates from the triangular space running between an adductor tubercle, medial femoral condyle & gastrocnemius tubercle, superior to a superficial medial collateral ligament (MCL).
- An MPFL inserts onto a superomedial aspect of a patella.
- A proximal insertion extends to the quadriceps tendon whereas the distal insertion crosses deep to a distal vastus medialis obliquus (VMO).
Function
- The main function of a medial patellofemoral ligament(MPFL) is to provide restraint to a patella while early knee flexion (0-30 degrees).
- This acts in maintaining appropriate patellar tracking within a trochlear groove while providing 50-60% of the restraining force against lateral displacement.
Clinical relevance
- While acute lateral patellar dislocations (LPD), a medial patellofemoral ligament is ruptured >90% of the time with almost 100% rupture happening in repeat dislocations.
- Lateral dislocations most often happen when the foot is planted & the internal rotational force is applied to the flexed, valgus knee joint. Medial patellofemoral ligament reconstruction surgery is often performed in patients with patellofemoral instability who may suffer recurrent lateral patellar dislocations.
- Surgical repair of the medial patellofemoral ligament restores medial patellar stability.
Assessment
- Medial patellofemoral ligament rupture will present with pain as well as tenderness along with a medial retinaculum & a medial border of a patella. A patient will present with apprehension while the lateral translation of a patella with the absence of the firm end feel.
Treatment
- Conservative treatment, especially after the first lateral patellar dislocation, has been regarded as the most appropriate course of treatment.
- Rehabilitation with physiotherapy & bracing is the prescribed treatment for lateral patellar dislocation. Surgical intervention of the medial patellofemoral ligament is performed only when conservative treatment fails or even if a patient presents with recurring dislocations.
Posterior Cruciate Ligament
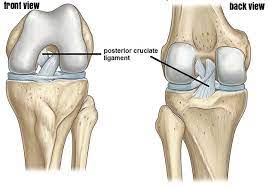
Description
- A posterior cruciate ligament (PCL) is the strongest as well as the largest intra-articular ligament in the human knee & the primary posterior stabilizer of the knee joint. It comprises two functional bundles: the larger anterolateral bundle (ALB) as well as the smaller posteromedial bundle (PMB). The size of a femoral attachment of the anterolateral bundle is near twice the size of its tibial attachment.
Attachments
- Origin
The posterior cruciate ligament originates from an anterolateral aspect of a medial femoral condyle within the notch. - Insertion
The posterior cruciate ligament inserts along with the posterior aspect of a tibial plateau, approximately 1 cm distal to a knee joint line. - The average surface area of the posterior cruciate ligament attachments to a femur as well as tibia was studied by Voos et al. This found the area of a femoral footprint to be 209 mm2 & tibial footprint to be 243 mm2. Hence, the posterior cruciate ligament insertion sites are roughly three times larger than their mid-substance.
Vascular Supply
- A middle geniculate artery perforates a posterior capsule running parallel to a superior edge of the synovial septum. It has branches to the posterior cruciate ligament synovium around the forming a plexus of vessels supplying the posterior cruciate ligament.
- There is also the potential supply from the branch of an inferior geniculate artery.
Nerve Supply
- A tibial, as well as obturator nerve, has posterior articular branches to a posterior capsule. These branches perforate a posterior capsule to reach the PCL.
Function
- The posterior cruciate ligament functions as one of the main stabilizers of a knee joint & serves primarily to resist excessive posterior translation of a tibia relative to a femur.
- The posterior cruciate ligament also acts as the secondary stabilizer of a knee preventing excessive rotation specifically between 90° and 120° of knee flexion. The two bundles of the posterior cruciate ligament, ALB as well as PMB function synergistically.
Clinical Relevance
- Posterior cruciate ligament (PCL) tears comprise 3% of outpatient knee injuries as well as 38% of acute traumatic knee hemarthroses.
- These injuries rarely happen in isolation, & up to 95% of posterior cruciate ligament tears happen in combination with other ligament tears. Posterior cruciate ligament tears are increasingly being recognized as a source of morbidity & decreased function due to persistent instability, pain, impaired function as well as the development of degenerative joint disease.
- The posterior cruciate ligament tears are typically produced by external trauma namely, a classic “dashboard injury” resulting from the posteriorly directed force on an anterior aspect of a proximal tibia with the knee flexed. In athletics, a typical mechanism of isolated posterior cruciate ligament tears is the direct blow to an anterior tibia or even a fall onto a knee with the foot in the plantar flexed position. Football, soccer, rugby as well as skiing are among the sports with the highest incidence of PCL tears.
- Symptoms depend upon an injury mechanism (high vs low-energy) & chronicity. Stiffness, swelling as well as pain on a posterior aspect of a knee are typical symptoms, while anterior knee pain as well as instability when descending stairs are more often associated with chronic isolated tears.
Assessment
- A careful vascular examination of the lower extremities is essential due to a posterior cruciate ligament injury that may be accompanied by a popliteal artery injury. If the pulses are weak or even an ankle-brachial index is 0.8, the intimal tear should be suspected & arteriography should be performed.
- Acute posterior cruciate ligament injuries present with joint swelling & about 10° to 20° of restriction in further flexion because of pain. Chronic posterior cruciate ligament injuries may present with limited activity like having difficulty in climbing slopes owing to lethargy & pain in the anterior as well as medial areas of a knee rather than instability.


One Comment