Dermatomes
Table of Contents
Overview
The term “dermatome” is a combination of two Greek words: “derma” meaning “skin” & “tome” meaning “cutting” or “thin segment”. Dermatomes are areas of the skin whose sensory distribution is innervated by afferent nerve fibers from the dorsal root of a single spinal nerve root, which is the portion of a peripheral nerve that “connects” that to the spinal cord.
Nerve roots arise from each level of the spinal cord (e.g., C3, C4), and many, but not all, converge in a plexus (brachial, lumbar, or lumbosacral) to form different peripheral nerves, as discussed above. This arrangement may give rise to a single nerve root supplying a few peripheral nerves. The median nerve, for example, is derived from the C6, C7, C8, and T1 nerve roots, while the ulnar nerve is derived from C7, C8, and T1.
30 dermatomes communicate sensation from a particular part of the skin to the brain: 8[Eight] cervical nerves (note that C1 has no corresponding dermatomal area), 12 [Twelve] thoracic nerves, 5[Five] lumbar nerves, and 5[five] sacral nerves. Each of the spinal nerves has roots. Infection, compression, or traumatic injury may lead to dysfunction or damage to a spinal nerve root, causing symptoms in the corresponding dermatome.
Function
Dermatomes can provide helpful details when healthcare providers are attempting to diagnose or treat a specific kind of medical problem. To understand this, imagine your spinal cord as a freeway. It procedures massive amounts of traffic — nerve signals — that travel between your body and brain.
Your spinal nerves function similarly to the on and off ramps of your spinal cord. Your spinal nerves allow nerve signals to come and go. If you lose muscle control in an area of your body or cannot feel temperature, touch, or pain, it could be due to a problem with the connected spinal nerve. In effect, the on- and off-ramps are closed, so there’s no traffic going to or from that location.
Dermatomes are an important indicator that can alert healthcare providers to a problem with your spine’s bones, spinal cord, spinal nerves, or any of their associated nerve branches. Depending on the affected dermatomes, healthcare providers can rule out certain conditions and narrow down the possibilities while attempting to provide care for you.
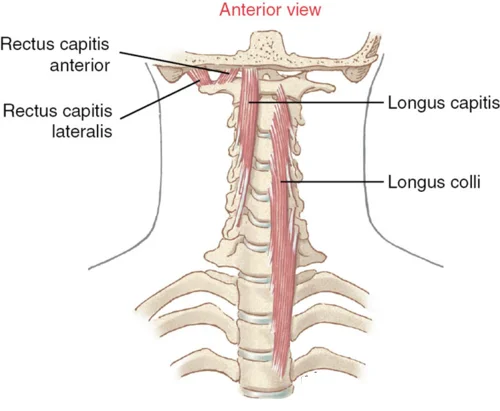
Spinal nerves originate from nerve roots. Dorsal nerve roots branch out from the spinal cord’s dorsal horn and perform sensory functions. Ventral nerve roots originate in the spinal cord’s ventral horn and transmit motor impulses to muscles.
The spinal nerves exit the spinal canal via intervertebral foramina (neuroforamina) and innervate various structures based on dermatomal patterns. There are 31 distinct spinal segments, which correspond to 31 distinct spinal nerves on both sides. The 31 spinal nerves are organized as follows:
- 8 pairs of cervical nerves
- 12 pairs of thoracic nerves
- 5 pairs of lumbar nerves
- 5 pairs of sacral nerves
- 1 pair of coccygeal nerves
The cervical nerves C1–C7 exit the intervertebral foramina above their respective vertebrae. The cervical nerve C8 exits between the C7 and T1 vertebrae. The remaining spinal nerves all exit beneath their respective vertebrae.
Axial dermatomes are primarily layered horizontally. In comparison, appendicular dermatomes are organized longitudinally. These patterns are fairly standard, with some variations due to the extensive overlap of spinal nerve coverage areas.
History
Dermatomes appeared as a result of early attempts to link anatomy and sensation biology. There are various definitions of dermatomes, and several maps are commonly used. Although useful, dermatomes differ significantly between maps and even among individuals, with some evidence indicating that current dermatome maps are inaccurate and based on flawed studies.
The medical profession typically recognizes two primary dermatome maps. To begin, the Keegan and Garret Map of 1948 depicts dermatomes that correspond to the developmental progression of limb segments. Second, the Foerster Map of 1933 depicts the medial area of the upper limb as innervated by T1-T3, indicating the distribution of pain from angina or myocardial infarction. This latter map is the most commonly used in healthcare and corresponds to the dermatomes used in the American Spinal Cord Injury Association Impairment Scale. In recent years, there have been few attempts to verify the original dermatome maps. Lee et al. conducted a thorough review of the discrepancies among dermatome maps.
Location of Dermatomes
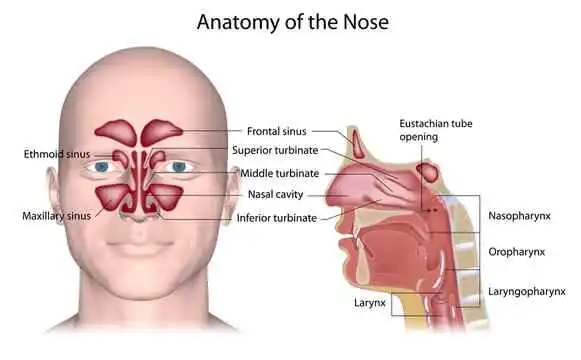
Dermatomes are skin areas that are controlled by nerves that connect to the spinal cord. That is, dermatomes cover the entire body except for the face. The nerves in your face are an exception because they are not connected to your spinal cord.
The structure of your spine’s nerve connections also results in a lot of overlap between a dermatome and its neighbors. So, sensations from a specific dermatome travel through multiple spinal nerves at the same time.
Understanding the layout of the dermatomes requires knowledge of spine anatomy. Your spine (also known as your backbone) is made up of interlocking bones called vertebrae (only one is a vertebra). Your spinal nerves branch out to the left and right from your spinal cord, passing through gaps in your vertebrae.
The spine has five sections:
- Cervical spine: It is located in your neck. It contains seven vertebrae and eight spinal nerves.
- Thoracic spine: It comprises your upper and middle back. This section contains twelve vertebrae and twelve pairs of spinal nerves.
- Lumbar spine: It is located in your lower back. It contains five and five pairs of spinal nerves.
- Sacral spine: This segment of your spine connects your backbone to your pelvis. It contains five vertebrae (which typically fuse by the time you reach adulthood) and five pairs of spinal nerves. Your sacral spine and pelvic bones together resemble a butterfly. Your sacral spine serves as the butterfly’s main body, while the pelvic bones form the wings.
- Coccygeal spine (pronounced “cah-kij-ee-ul”): These form your tailbone (coccyx). It has four vertebrae (which typically fuse by the time you reach adulthood) and one pair of spinal nerves.
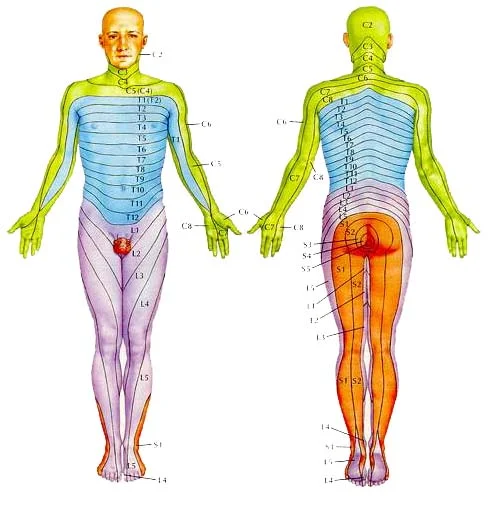
Healthcare providers refer to the spinal nerves by a letter-number combination. For example, the eighth spinal nerve is abbreviated as C8. These letter-number combinations can also identify the affected dermatomes.
Dermatomes related to the cervical spine
Nerves in the cervical section of your spine communicate with dermatomes in your head, neck, shoulders, arms, and hands. The nerve dermatomes in your cervical spine are as follows:
- C1: People who do not have a C1 spinal nerve are more likely to lack a C1 dermatome. This dermatome is located in the center of the back of the head.
- C2 to C3: Upper neck, a small area of your jaw beneath each ear, and the back of your head
- C3 to C4: Lower neck region, upper chest, and upper back.
- C4 to C5: Shoulders and upper arms.
- C5 to C6: Thumb side of upper arm and forearm, as well as the thumb itself.
- C6 to C7: Index and middle fingers, as well as the thumb side of your forearm.
- C6 to C8: The pinky side of your lower forearm and wrist, as well as the ring and pinky fingers.
Dermatomes related to the thoracic spine
The dermatomes of your thoracic spine are primarily located on the trunk of your body, which includes your chest, belly, and back. The only thoracic-connected dermatomes not located on your trunk are T1 (which is entirely on your arms) and T2 (which is on both your arms and trunk). The dermatomes T3–T12 form rings around your body’s trunk.
The locations of the dermatomes are:
- T1-T2: The pinky side of your upper forearm and upper arm, as well as the chest and back just above your armpits.
- T2 to T3: The pinky side of your upper arm, upper chest, and upper back (just above the armpits and shoulder blades).
- T3-T4: Chest and back at the same level as your armpit and the center of your shoulder blades.
- T4-T5: Lower edge of pectoral muscles and lower part of shoulder blades.
- T6–T7: At the same level as the bottom edge of your sternum (also known as your breastbone).
- T7–T8: At the same level as the lower edges of the lowermost part of your ribcage.
- T8–T9: Upper belly, which includes the top parts of your abdominal muscles.
- T9 to T10: The area immediately above and level with your belly button (navel) and the upper-middle section of your back.
- T10 to T11: The area just below your belly button and in the center of your middle back.
- T11-T12: The lower part of your abdomen just above your hip bones (pelvis) and the lower section of your middle back.
Dermatomes of the lumbar spine
Dermatomes in your lumbar spine connect to areas of your hips, legs, and feet. The dermatomes’ locations are as follows:
- L1 to L2: The upper part of your hips, pubic area, the upper part of the small of your back, and the sex organs[Men and people assigned male at birth have penis and testicles, while women and people assigned female at birth have a vagina]
- L2 to L3: Muscles in your upper thigh and groin, as well as the middle of your lower back.
- L3 to L4: This includes the front and outer sides of your thigh muscles (quadriceps), your kneecaps, the outer edge of your leg just above your knee, and the middle-lower section of your back.
- L4-L5: The kneecap and front of your lower leg, the inner sides of your calf muscles, and the inner front surface of your feet, which includes your big toe, and second and third toes.
Dermatomes of the sacral and coccygeal spine
Sacral spine dermatomes include the areas around your buttocks and the back of your legs. As a result, the coccygeal section of your spine contains only one spinal nerve and a single connected dermatome.
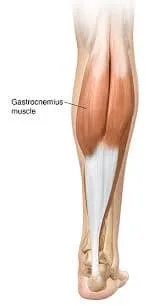
- S1-S2: The uppermost section of your buttocks (including the gluteal cleft, which separates your buttocks), the middle and outer sections of the back of your thighs and calf muscles, the outer side of your ankles, and your 4th and 5th toes.
- S2-S3: A vertical area in the middle of your buttocks that extends downward through the inner-middle section of your back thigh and the upper-middle section of your calf muscles.
- S3 and below: Every spinal nerve from S3 down (including your coccygeal spinal nerve) connects to an area containing your genitals and the skin between them (known as the perineum).
Purpose
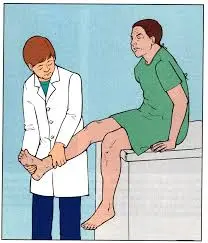
The neurological examination involves dermatome testing. They are primarily used to determine whether a limb’s sensory loss corresponds to a single spinal segment, implying the lesion is of that nerve root (i.e., radiculopathy), & to assign the neurologic “level”.
Technique
Dermatome testing is best done with a pin and cotton wool. Asking the patient to close their eyes & give the therapist feedback on the various stimuli. Testing should focus on specific dermatomes and be compared bilaterally.
- Light Touch Test: Dab a piece of cotton wool on an area of skin.
- Pinprick Test: Pain Sensation – Gently touch the skin with the pin, asking the patient if it feels sharp or blunt.
During the system review, asking the patient to describe the pattern, and distribution of sensory symptoms (e.g.- tingling, numbness, diminished or absent sensation) provides the therapist with preliminary information to guide the examination and identify the affected dermatome(s) and nerves.
Light-touch dermatomes are bigger than pain dermatomes. When only one or two segments are affected, pain sensibility tests are more sensitive than light touch tests.
Controversies
Dermatomes are distributed in segments throughout your body. The exact dermatome pattern can differ from person to person. There may be some overlap between neighboring dermatomes. There are some differences between published dermatome maps based on the methods used to identify skin segment innervation.
In a clinical commentary, Downs and Laporte discuss the history of dermatome mapping, including the variations in methodologies used, and the inconsistencies in the dermatome maps used in education and practice.
Clinical significance
Dermatomes are important because they can be used to assess and diagnose a wide range of conditions. Neurological screening of dermatomes aids in identifying patterns of sensory loss that may indicate specific spinal nerve involvement. For example, symptoms along a specific dermatome may indicate a disruption or damage to a specific nerve root in the spine.
- Nerve Entrapment
- Radiculopathy
- Spinal Cord Injury
- Herpes Zoster
Radicular Pain and Radiculopathy
Radicular pain, also known as nerve root pain, is defined as radiating pain caused by damage or irritation to a single posterior root or spinal ganglion. It is commonly caused by spinal stenosis or a herniated disc and is characterized as shooting, burning, or lancinating pain that travels down the limb.
Radicular pain is not the same as radiculopathy, though the two are frequently associated. Radiculopathy is the objective loss of sensory and/or motor innervation caused by impaired impulse conduction along a spinal nerve or its roots. It manifests as numbness and/or weakness limited to the dermatome and/or myotome of the damaged dorsal root and is not accompanied by pain.
Lumbar radicular pain is also known as sciatica. This pain originates in the lower back and travels down the back of the thigh and leg, following the path of the sciatic nerve. Radicular pain is typically treated and managed through physical therapy, medication, and spinal procedures. If these methods are ineffective, surgeries such as discectomy (removal of an intervertebral disc) or laminectomy (removal of a vertebra’s lamina) can help relieve pain.
Spinal cord injury & Trauma
Dermatomes are particularly useful in determining the site of damage in spinal cord injuries. Doctors examine one dermatome at a time.
Herpes Zoster
Herpes Zoster (shingles) is a peripheral nervous system infection caused by the reactivation of the Varicella-Zoster virus. Because this virus causes chickenpox, only those who have had it can develop shingles. After a person recovers from chickenpox, the virus moves to a single spinal ganglion and usually remains inactive.
Reactivation of the virus is possible because cell-mediated immunity declines with age, and it typically affects people over the age of 50. The reactivated virus can leave the spinal ganglion and affect the skin’s sensory neurons. The dermatome of the infected dorsal root is characterized by discoloration, pain, rash, and a line of blisters. The most affected dermatomes are the thoracic and lumbar areas.
Antiviral medications (acyclovir, famciclovir, or valacyclovir) and analgesics are commonly used to treat shingles pain. Pain typically lasts three to five weeks, but can last for years if postherpetic neuralgia (PHN) develops as a complication. The best way to avoid contracting chickenpox or shingles is to get vaccinated.
Conditions and Disorders
While dermatomes are skin areas, the conditions that affect them are usually caused by deeper-level issues in your body. Dermatome issues arise because they affect specific spinal nerves or the spinal cord in that region. As a result, any condition affecting your spinal cord or spinal nerves can cause symptoms related to dermatomes. In these cases, the damage is very localized, but the effects vary depending on which dermatomes are affected.
The following conditions can result in this type of damage or effect:
- Injuries: A spinal nerve root or spinal cord injury can affect one or more dermatomes. The most common causes of these injuries are car accidents, penetrating trauma (such as knife or gunshot wounds), and spinal fractures caused by falls. This can also be caused by injuries sustained during birth or in the first few weeks of life (for example, cerebral palsy).
- Spinal tumors, including cancer: This could be cancer that develops on or around your spinal cord, or cancer that begins elsewhere in your body and spreads to your spine.
- Cysts are fluid-filled cavities: Syringomyelia is a condition in which these form around the spinal cord.
- Infections: These can directly attack your spinal cord and nerve roots, causing inflammation and swelling. Because there isn’t much space for swelling around your spinal cord, it can put too much strain on your spinal nerves or the spinal cord itself.
- Ischemia, or a lack of blood flow: As with all other body tissues, your spinal cord and nerves require blood flow. A blocked or ruptured blood vessel can cause blood flow to stop.
- Congenital conditions: These are the conditions you have at birth. Some congenital disorders affect the structure of your spine, spinal cord, or spinal nerves. Examples of this include myelomeningocele and spina bifida.
Common signs or symptoms of dermatome-related conditions
Dermatome conditions result from nerve or spinal cord disruptions. Disruptions like this can cause a variety of symptoms. These symptoms are classified into 3 categories:
- Motor (movement-related)
- Sensory (touch-related)
- Autonomic (bodily processes that occur automatically)
Motor symptoms:
- Muscular weakness or paralysis
- Uncontrolled muscle movements (whether inactive or uncontrollably active)
- Muscle atrophy is the wasting and shrinking of muscles caused by inactivity
Sensory symptoms:
- Symptoms include tingling, numbness, and pain.
Autonomic symptoms:
Autonomic processes are bodily functions that operate without conscious awareness. These functions are important because they allow your body to maintain and regulate itself. If you have damage to a dermatome that interferes with autonomic functions, you may experience symptoms indicating that your body is unable to automatically control processes in that area. Examples include:
- Sweating excessively (hyperhidrosis) or not enough (anhidrosis).
- Problems controlling muscles in your bladder or bowels, affecting your ability to pee(urinary incontinence) or pop(fecal incontinence)
- Sexual dysfunction.
Some common tests to check for problems with dermatomes
Several tests can identify or diagnose problems with your spinal nerves and dermatomes. The most common are imaging and nerve signal detection tests, including:
- Computed tomography (CT) scans
- Magnetic resonance imaging (MRI) scans
- Cisternogram scan
- Electromyogram (EMG) tests
Treatment is available for dermatome-related conditions.
Treatments for conditions affecting your spinal nerves and dermatomes vary depending on the underlying cause and circumstances. Because treatment options can vary so greatly, a healthcare provider is the best person to inform you about the available treatments and what they recommend.
Care
Dermatomes are indicators of how well your spinal cord and nerves are functioning, so taking care of them begins with taking care of your spine. Remember the following facts about your spine and spinal nerve health:
- Wear safety equipment, such as seat belts, as recommended: Motor vehicle collisions are among the leading causes of spinal injuries. Seat belts and other restraints can protect you from serious injuries.
- Lift safely: Lifting with your legs rather than your back can help you avoid spinal cord and nerve injuries (like a herniated disk). If you have a history of back problems, you may need to wear a back support brace, especially if your job requires a lot of lifting or you regularly lift weights for physical activity.
- Be cautious when using firearms: Gunshot wounds are one of the leading causes of spinal cord injuries. You should ALWAYS treat firearms with extreme caution, regardless of the circumstances. Act as if they are loaded, even if you know they aren’t. Firearms should also be stored unloaded, with a trigger lock, and out of reach of children. It is also a good idea to keep ammunition separate and locked up.
- Take precautions to prevent falls: When working at heights, safety equipment, particularly safety harnesses, is essential. You should also take precautions to avoid falls at home, particularly on stairs or in the bathroom. This may include installing handrails, using nonslip footwear and floor surfaces, and keeping stairs free of tripping hazards.
- Make bone health a priority: Bone-loss conditions such as osteoporosis and osteopenia can result in vertebral fractures. These fractures can cause severe spinal cord and nerve damage.
- Posture is important: Poor posture while sitting or standing can put unnecessary strain on your back. This can cause pressure on your spinal cord and nerves. Pinched nerves are one example of this.
Summary
Dermatomes are skin areas that are connected to a single spinal nerve. These areas work together to create a surface map of the body.
Dysfunction or damage to a spinal nerve can cause symptoms in the associated dermatome. Nerve damage or dysfunction can result from infection, compression, or traumatic injury.
Doctors may use the severity of symptoms in a dermatome to determine the extent and location of nerve damage. They then work to determine and treat the root cause of the damage.
FAQs
A dermatome is a skin area that receives sensory input from a specific spinal nerve root. There are 30 dermatomes in total, classified as cervical, thoracic, lumbar, sacral, and coccygeal levels. Eight cervical levels cover the skin from the scalp to the arms.
Infection, compression, or traumatic injury can all cause dysfunction or damage to a spinal nerve root, resulting in symptoms in the corresponding dermatome.
Somatosensory and autonomic nerves supply the human skin. The former terminates in the dermis, forming various morphotypes of sensory corpuscles and free nerve endings (dermal and epidermal), or contacts specialized epithelial cells, such as Merkel cells.
T9–T12 vertebrae Thoracic Spinal Cord Injury – SpinalCord.com
The thoracic spine
The thoracic spine’s base is made up of the vertebrae T9, T10, T11, and T12. The thoracic spine consists of 12 segments connecting the cervical and lumbar levels. Sections T9–T12 are referred to as transitional vertebrae due to their proximity and similarity to the lumbar vertebrae.
Upper limb dermatomes are upper-limb skin areas supplied by a single posterior spinal nerve root. For example, more caudally: T7 Xiphisternum. T10 level
A dermatome is a section of skin innervated by a single dorsal nerve root. Sir Henry Head, Otfrid Foerster, 2 Jay Keegan, Frederic Garrett, and others all contributed to our understanding of dermatomes.
REFERENCES
- Dermatomes. (n.d.). Physiopedia. https://www.physio-pedia.com/Dermatomes
- Professional, C. C. M. (n.d.). Dermatomes. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24379-dermatomes
- Dellwo, A. (2024, January 19). What Dermatomes Are and Why They’re Important. Verywell Health. https://www.verywellhealth.com/dermatomes-5186825
- Dermatomes. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/dermatomes
- Johnson, J. (2023, April 25). What and where are dermatomes? https://www.medicalnewstoday.com/articles/what-are-dermatomes