The Spinal Cord
Table of Contents
What does the spinal cord do?
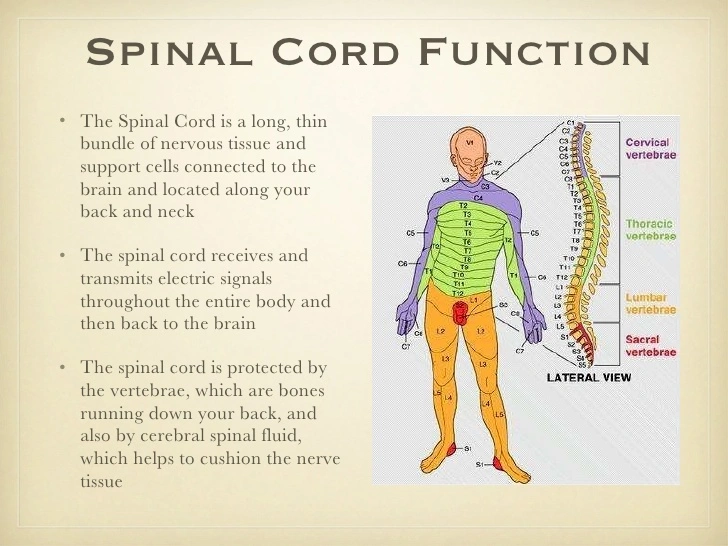
- The spinal cord is a lengthy, tissue-filled tube. It ties the brain and the lower back together. The spinal cord Relays nerve impulses from the brain to the body and the other way around. These nerve messages Enable you to move and feel your body. Movement or function may be impacted by a spinal cord disorder Or injury.
- Your spinal cord passes cylindrically through the center of your spine from the brainstem to the lower Back. It is a fragile structure made up of cells and nerve bundles that send signals from the brain to the Rest of the body. A key component of the neurological system is your spinal cord.
What differentiates the spinal cord from the vertebral column?
- The spine is often used to refer to the spinal cord and vertebral column. A bundle of cells, tissues, And nerves makes up the spinal cord. The vertebral column, a protective covering of bone, surrounds and Shields the spinal cord.
- The vertebrae (plural of one spine bone, a vertebra) make up the vertebral column. From your pelvic Bones to your brain, the vertebrae stack on top of one another. There is a spinal disc in between each pair Of vertebrae. Discs have a durable outside and a gel-like inside. They serve as a cushion and shock Absorber for the vertebrae and spinal cord.
What function does the spinal cord have?
- Transporting nerve signals throughout the body is the spinal cord’s main job. Three crucial functions are carried out by these nerve signals. One of them is having control over your body’s movements and functions. Brain signals are supplied to various parts of the body to control movement. Additionally, they regulate Autonomic (involuntary) functions like breathing, heart rate, and bowel and bladder functions.
- Inform your brain of your senses. With the help of messages from other parts of the body, the brain Registers and interprets sensations like pressure or pain.
- Control your reflexes. Some reflexes (involuntary movements) are managed by the spinal cord Independently of the brain. For instance, the spinal cord controls the patellar reflex, which causes your leg To move unintentionally when someone taps it in a specific location.
What constitutes the spinal cord’s primary components?
Three major sections make up the spinal cord:
- Neck, or cervical.
- Chest, or thoracic.
- Lower back (lumbar).
What organs and substances give rise to the spinal cord?
Like the brain, the spinal cord is covered with layers of tissue called meninges. These insulating Tissues consist of:
- Dura mater The outer layer protects against damage to the spinal cord.
- Between the epidural and subarachnoid spaces, there is a layer called the Arachnoid mater.
- Pia Mater The spinal cord is protected by the inner layer.
What are the arachnoid and epidural spaces?
- Between the dura mater and the arachnoid mater is where the epidural space is located. The epidurals, Which are used to administer anesthetic during labor, are inserted here.
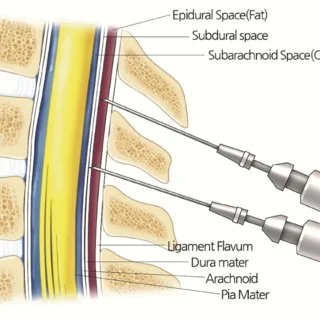
- Here, the spinal cord receives additional cushioning & protection from cerebrospinal fluid (CSF).
- To test CSF for certain infections, medical professionals occasionally poke a needle into the Subarachnoid area. A spinal tap is what is done in this situation. Extra shock absorption for the spine is provided by both the epidural and arachnoid compartments.
In the spinal cord, which nerves are present? or The spinal cord contains what types of nerves?
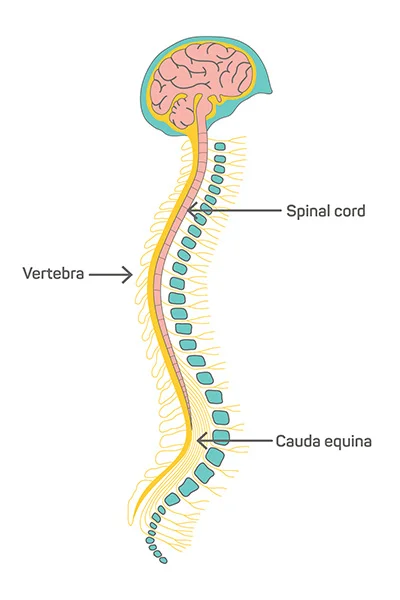
The spinal cord has 31 pairs of nerves and nerve roots. These consist of:
- There are eight cervical nerve pairs, which originate in the neck and generally go to the head and face.
- There are twelve pairs of thoracic nerves in the upper torso, which run from the chest to the upper back And belly.
- Five lumbar nerve pairs (low back nerves that travel to the legs and feet).
- There are five pairs of sacral nerves (low back nerves continue into the pelvis).
- The cauda equina, a bundle of nerves, is located near the base of the spinal cord. Because early Anatomists believed the nerve collection resembled a horsetail, the term “cauda equina,” which means “Horse’s tail,” was coined in Latin. There are nerves in the cauda equina that give the lower body Sensation.
- The brain, spinal cord, and the rest of the body receive electrical signals from the spinal nerves. These Electrical nerve signals allow you to move your body (motor nerves) and feel sensations (sensory nerves).
- The medulla oblongata, located near the base of the brainstem, is where the spinal cord starts. The spinal Cord curves into a cone shape at the base of the spine, or conus medullaris.
- The spinal cord is typically 18 inches (45 cm) in length in adults.
What diseases and ailments have an impact on the spinal cord?
- The spinal cord may be impacted by numerous conditions or wounds. Serious diseases and damage to The spinal cord exist. Any spinal cord injury might result in significant symptoms in the bodily sections Below the injured area.
- A spinal cord injury’s severe symptoms may result in paralysis or a loss of bladder control. Rapid Treatment for some illnesses can reduce the possibility of persistent or lifelong effects.
- Acute transverse myelitis inflammation in one or more spinal cord regions.
- Cervical disc disease. cervical myelopathy is the progressive degeneration of the spinal disks in your Neck, which can put pressure on the spinal cord.
- Disk herniation. when a spinal disk shifts out of position and presses against adjacent nerves as it slides Into the area around the spinal cord.
- Spine injuries. when the spinal cord is compressed (compression fracture) or ruptured (burst fracture) by One or more vertebrae.
- Atrophy of the spinal muscles. an uncommon hereditary disorder that results in the spinal cord’s motor Nerve cells dying off, weakening and atrophying muscles.
- Spinal stenosis. spinal column narrowing, causing pinched nerves and spinal cord discomfort.
The spinal cord may be impacted by several common conditions, including:
- Spinal tumors are masses that begin in the spinal column and can impose pressure on the spinal cord. They could be benign or cancerous.
- Infections of the spine. when the spinal cord is put under pressure by an enlarging abscess or the Collapse of an infected vertebra or disc.
Care
- Eat a healthy, balanced diet that contains fruits, vegetables, whole grains, lean meats, and other nutrients.
- Exercise continuously, alternating between stretching, strengthening, and aerobic exercises.
- Practice keeping a straight spine and refrain from slouching whether standing or sitting.
- Give up smoking and other tobacco use.
- Sleep in postures that support the lower back’s and neck’s natural curves.
- Take frequent breaks and go for walks.
- Drink in moderation and abstain from recreational drug use.
- By maintaining healthy habits, you can protect your spinal cord, vertebral column, and entire back.
Spinal cord injury
What causes spinal cord injury?
- Damage to the spinal cord or the nerves at the cauda equina, which are at the end of the spinal canal, can result in spinal cord injuries that permanently alter strength and feeling as well as other bodily functions Below the injured area.

- It could seem as though every part of your life has been impacted if your spinal cord has recently been Harmed. The injury’s ramifications may be felt by you mentally, emotionally, and socially.
- Many scientists are certain that future scientific developments will make spinal cord damage repairable. All Across the world, research efforts are ongoing. While waiting for recovery, many people with spinal cord Injuries can lead active, independent lives thanks to treatments and rehabilitation.
What signs and symptoms indicate spinal cord injury?
- The bodily components that paraplegia and quadriplegia affect
- Spinal cord damage brings up a pop-up menu
- Following a spinal cord injury, your capacity to control your limbs is influenced by two factors: the location And seriousness of the injury.
The neurological level of the injury is the lowest portion of your spinal cord that is unharmed following a Trauma. The “completeness” of the injury, often known as its severity, can be one of the following:
- Complete. Your injury is deemed complete if all sensation (sensory) and all motor functions are gone Below the spinal cord injury.
- Incomplete. The injury is referred to as incomplete if you still have some motor or sensory function below The affected area. Different levels of incomplete damage exist.
- Additionally, paralysis brought on by a spinal cord injury is known as:
- Tetraplegia. The spinal cord damage also referred to as quadriplegia, affects your arms, hands, trunk, Legs, and pelvic organs.
- Paraplegia. The trunk, legs, and pelvic organs are all or partially paralyzed by this condition.
- To ascertain the extent of the neurological damage, your medical team will run a number of tests.
Injuries to the spinal cord may result in one or more of the following symptoms:
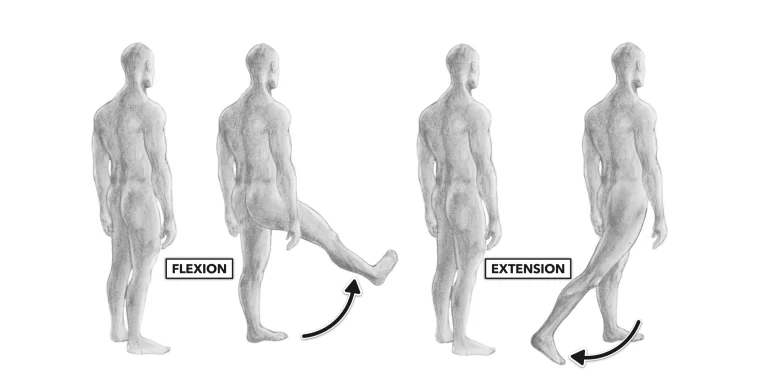
- Decline in movement
- Loss of or change in feeling, including touch, heat, and cold
- A lack of bladder or bowel control
- Hyperactive reflex actions or spasms
- Changes to sexual sensitivity, function, and fertility
- Damage to the spinal cord’s nerve fibers can result in acute pain or stinging.
- Breathing, coughing, and removing pulmonary secretions are difficult.
Symptoms or indicators of an emergency
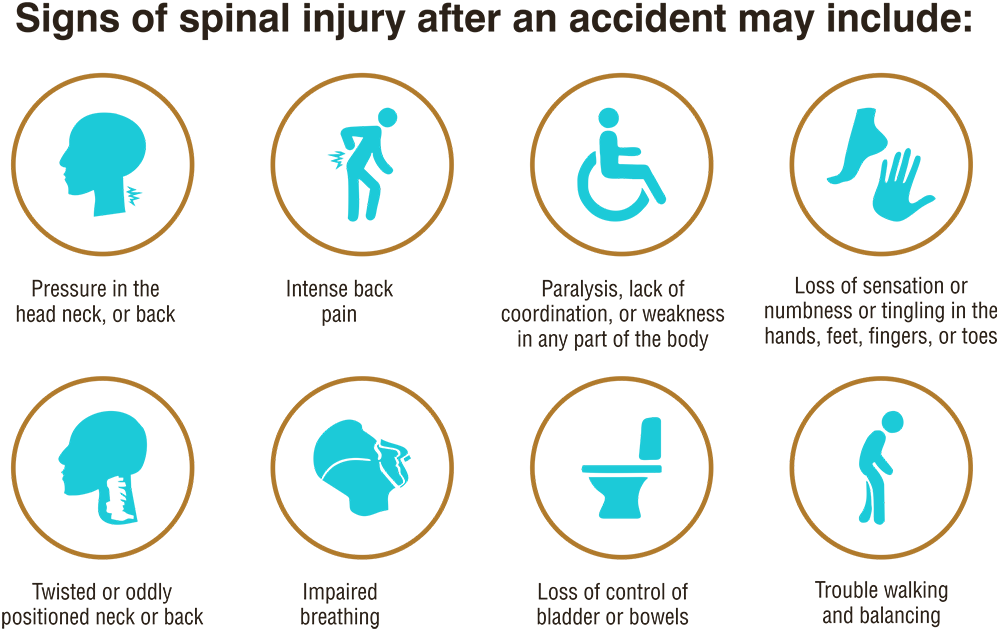
Following an accident, there are immediate signs or symptoms of a spinal cord injury including:
- Extreme neck, head, and back pressure and low back discomfort
- Paralysis, clumsiness, and weakness in any area of the body
- Loss of feeling in the hands, feet, fingers, or toes, as well as numbness, tingling, and tingling
- A lack of bowel or bladder control
- Difficulty walking and balancing
- Breathing problems following an injury
- An abnormally twisted or positioned neck or back
When have to visit a doctor?
- Anyone who sustains serious head or neck trauma has to be seen by a doctor right away to rule out spinal Injuries. In fact, it’s best to assume that trauma victims have spinal injuries until otherwise demonstrated For the following reasons: A major spinal injury isn’t often immediately apparent. If it is unknown, more Serious harm could happen.
- Numbness and paralysis may start suddenly or develop gradually.
- In deciding the amount and severity of consequences and the potential extent of expected recovery, the Interval between the injury and treatment can be crucial.
In the event that you think someone may have a neck or back injury:
- Keep the injured individual still since moving them could cause permanent paralysis and other Catastrophic problems.
- Hold the head and neck still until emergency help arrives by placing thick towels on both sides of the neck.
- Without moving the head or neck, administer basic first aid, such as halting the bleeding and keeping the patient comfortable.
What factors lead to spinal cord injury?
- The central nervous system’s anatomy.
- Damage to the spinal column’s vertebrae, ligaments, disks, and spinal cord itself can result in spinal cord Injuries.
- A quick, traumatic impact to the spine that fractures, dislocates, crushes, or compresses one or more Vertebrae can result in a traumatic spinal cord injury. The spinal cord can potentially be penetrated and cut By a gunshot or knife wound.
- As a result of bleeding, edema, inflammation, and fluid collection in and around the spinal cord, more Damage typically develops over the course of days or weeks.
- Arthritis, cancer, inflammation, infections, and degenerative disc disease of the spine can all result in non-traumatic spinal cord damage.
- Your central nerve system and brain
- The central nervous system includes both the brain and the spinal cord. Soft tissue and bones (vertebrae) Surround the spinal cord. It stretches downward from the base of your brain and is filled with nerve cells And tracts—groups of nerves that travel to various body regions.
- The conus medullaris, often known as the lower end of the spinal cord, is located just above the waist. Located below this region is a collection of nerve roots known as the cauda equina.
- The spinal cord contains tracts that transport information between the brain and the rest of the body. The Brain sends signals to the motor tracts to keep muscles moving. Sensory pathways transmit information About heat, cold, pressure, pain, and the posture of the limbs to the brain from various body parts.
- Injury to the nerve fibers
- No matter the cause—traumatic or not—damage affects the nerve fibers that travel through the affected area and may completely or partially disable the muscles and nerves below the site of the injury.
- An injury to the thorax or lumbar region of the back can have an impact on the torso, legs, bowel and Bladder control, and sexual function. Along with impairing arm movements and sometimes your ability to Breathe, a neck (cervical) injury affects the same areas.
- Most typical reasons for spinal cord injury
The following are the most frequent reasons for spinal cord injury in the US:
- Accidents with vehicles Nearly half of all new spinal cord injuries each year result from auto and Motorcycle accidents, which are the main cause of spinal cord injuries.
- Falls. The majority of spinal cord injuries that occur after age 65 are brought on by falls.
- A violent act Violence, typically from gunshot wounds, causes about 12% of spinal cord injuries. Knife Wounds are also frequent.
- Injury-related to sports and leisure 10% of spinal cord injuries are caused by athletic endeavors like Diving in shallow water and contact sports.
- Diseases Spinal cord damage can also result from cancer, rheumatoid arthritis, osteoporosis, and spinal cord inflammation.
What are the potential causes of spinal cord injury?
Although a spinal cord injury is typically caused by an accident and can happen to anybody, there are some things that can put you at increased risk of suffering one, such as:
- Being a man. Many men are affected by spinal cord injury. In actuality, only 20% of Traumatic Spinal cord injuries in the US occur in females. having an age range of 16 to 30. In this Age group, Spinal cord injuries occur in more than half of cases.
- Being above 65. At age 65, there is another projection of spinal cord injury. Older folks are more at risk From falls.
- Using alcohol. About 25% of traumatic spinal cord injuries involve alcohol consumption.
- Taking a dangerous action. Spinal cord injuries can result from sporting activities, diving into too shallow Water, and other activities when the required safety equipment and procedures are not used. For those Under 65, automobile accidents are the main cause of spinal cord injuries.
- Having certain illnesses. If you have an additional condition like osteoporosis that affects the joints or Bones, even a seemingly slight injury can result in spinal cord damage.
What side effects might a spinal cord injury cause?
The body’s altered physiological processes can initially feel overwhelming. However, the rehabilitation team Will suggest techniques and resources to improve your quality of life and independence in addition to helping You address the changes brought on by the spinal cord injury. Frequently impacted areas include:
Bladder management. The kidneys’ urine will continue to be stored in the bladder. Because the spinal cord, Which is the message carrier, has been damaged, the brain may not be able to control the bladder as well.
The use of a replacement for bladder control raises the risk of uTIs. Additionally, kidney infections and Kidney or bladder stones may result from the modifications. You’ll discover techniques to assist bladder Emptying throughout recovery.
Bowel control. Although the stomach and intestines still function much as they did before the damage, Bowel movement regulation is frequently changed. A diet heavy in fiber may aid in bowel regularity, and During rehabilitation, you will learn how to control your bowels.
Pressure injuries. You might have lost all or part of your skin’s feelings below the level of harm to your Nervous system. As a result, when the skin is harmed by certain things like continuous pressure, the skin is Unable to communicate with the brain.
This may increase your susceptibility to pressure sores, but frequently switching positions with assistance, If necessary, can help prevent these sores. During rehabilitation, you’ll learn how to properly care for your Skin, which can assist the patient avoid these issues.
Circulation management. Circulatory issues resulting from a spinal cord injury can include swelling of the Extremities to orthostatic hypotension, a condition where your blood pressure drops as you stand up. The Chance of forming blood clots, such as deep vein thrombosis or a pulmonary embolus, can also rise as a result of these circulation abnormalities.
An additional issue with the circulatory system or circulatory control is an increase in blood pressure That could be fatal (autonomic dysreflexia). If these issues are relevant to you, the rehabilitation team will Instruct the patient on how to handle them.
Respiratory system. If the abdomen and chest muscles are compromised by the injury, it could be more difficult to breathe and cough.
What kind of breathing issues you encounter will depend on the severity of the neurological damage. Patients who have had cervical and thoracic spinal cord injuries may be more susceptible to Pneumonia and other lung conditions. These issues can be prevented and treated with medication and Counseling.
Bone thickness. Osteoporosis and fractures below the level of injury become more likely following spinal Cord injury.
Muscle texture. Spasticity, which is an uncontrollable tightening and motion of the muscles, and flaccidity, Which is a soft and limp muscular deficiency, are two different muscle tone issues that some patients with Spinal cord injuries have.
Wellness and fitness. Muscle atrophy and weight loss are frequent in the initial stages of spinal cord injury. A sedentary lifestyle brought on by limited movement increases your chance of developing diabetes, heart disease, and obesity.
A dietician can assist the patient in maintaining a healthy weight by recommending a balanced diet. Physical and occupational therapists can assist you in creating an exercise and fitness regimen.
Sexual wellness. Following a spinal cord injury, men may feel changes in erection and ejaculation, while Women may note changes in lubrication. Options, particularly for sexual functioning & fertility, can be provided by doctors who specialize in urology & fertility.
Pain. Some people experience pain from overusing certain muscle groups, such as muscle and joint pain. After a spinal cord injury, nerve discomfort is possible, especially in those with an incomplete recovery.
Depression. overcome the changes that a spinal cord injury brings about, and living with pain can make Some people depressed.
How is diagnosed to the spinal cord injury?
In an emergency, a medical professional checks to see if breathing or heart rate are not being affected by a Spinal cord injury. The condition of the nerves will then be evaluated.
The supplier verifies:
- The capacity to move different bodily parts is known as motor function.
- Sensory ability, or the capacity for touch.
- A spinal cord injury can be identified using certain imaging tests:
- CT scan to check for blood clots, blood vessel damage, and shattered bones.
- MRI to view the soft tissues and spinal cord.
- A bone dislocation (broken bone) can be shown on an X-ray along with broken bones.
- If there are concurrent peripheral nerve injuries, a medical professional may also utilize an Electromyogram to examine the electrical activity in muscles and nerve cells.
What is the Treatment for spinal cord injury?
- If there is trauma to another portion of the body surface, you can require emergency surgery for a spinal Cord injury. Broken bones, blood clots, and damaged tissue to the spinal cord can all be treated surgically.
- According to some research, spinal cord injury may benefit from a corticosteroid injection. The drug needs To be administered within eight hours of the injury. This therapy might:
- Increasing blood flow.
- Maintain neuronal activity.
- Cut the inflammation.
Long-term therapy
Long-term objectives of spinal cord injury therapy include:
- Increasing freedom and overall quality of life.
- Lowering the likelihood of developing chronic (ongoing) health problems.
- By partially restoring nerve function, partial nerve damage is prevented.
A spinal cord injury can have the following long-term effects:
- Failure to regulate blood pressure and body temperature.
- Increased chance of lung or heart issues.
- A lack of bowel or bladder control.
- Arms or legs are paralyzed.
- Chronic discomfort.
- Joint contracture and spasm.
- Dysfunction in sexual behavior.
Will I need therapy if I sustain a spinal cord injury?
Most spinal cord injury victims will need some sort of physical therapy or rehabilitation. The patient might Require rehabilitation that is either inpatient (during a hospital stay) or outpatient (after a hospital stay). An Intervention group can assist you in:
- Learn how to use wheelchairs and walkers as assistance devices.
- Regain mobility and strength in the body’s nerve-containing regions or sections.
- Regain the abilities required for daily tasks, such as dressing and using the restroom.
What are neural prosthetics and how may they benefit someone with a spinal cord injury?
- Spinal cord injuries may benefit from using neural prostheses, or prosthetic body parts. Similar to how an Arm or leg prosthesis replaces a missing limb, a brain prosthesis restores lost nerve function. To still-Active nerves, an electrical device is attached. These nerves are used to control the prosthesis, which Allows you to move the body’s immovable regions.
What is the spinal cord injury physiotherapy regimen?
Important Physiotherapy Concepts
It’s crucial that physical therapists comprehend the following ideas and how they apply to the management Process.
- Injuries to the vertebral column (acute stage influences therapy intensity)
- Spinal Shock (three days to three months of temporary loss of reflexes)
- Spinal cord damage above T6 results in elevated sympathetic activity, causing autonomic dysreflexia
- Orthostatic hypotension (dizziness brought on by raised blood pressure as a result of shifting from a Supine to a sitting position)
- Know the symptoms and indicators of deep vein thrombosis (DVTs) and pulmonary embolism (PE) to Ensure safe treatment
- Bowel and Bladder Dysfunction
- Pressure sores (treatment sessions include pressure sore prevention)
- Consume Ossification (soft tissue calcification that can cause contractures)
- Mental and emotional distress (identify symptoms and indicators and alert the relevant team members)
Depending on the severity and kind of the spinal cord injury, the acute care and rehabilitation are Determined. People who have suffered a spinal cord injury frequently need to be treated in an intensive care Unit at first. The rehabilitation process then typically begins in an acute care setting and is continued in a Dedicated Spinal Injury Unit. The length of inpatient therapy can range from 8 to 24 weeks, with outpatient Rehabilitation in the months that follow lasting 3 to 12 months.
An individualized interdisciplinary strategy is necessary for the difficult and lifelong management of a person With a spinal cord injury. The purpose of an interdisciplinary, functional, goal-aligned rehabilitation program is To let the person with a spinal cord injury lead as full and independent a life as possible. Occupational Therapy, speech and language therapy, and physiotherapy, Under the direction of a physiatrist or Rehabilitation physician, rehabilitation nurses, social workers, psychologists, and other health and social Care specialists collaborate to set goals with the patient and create a discharge plan that is suitable for their Level of injury and circumstances.
The following are the top five steps in the care of those with spinal cord injury:
- Evaluating disabilities, activity limits, and participation limitations
- Setting objectives that are in line with activity restrictions and participation restrictions
- Recognizing the main limitations that prevent the achievement of goals
- Locating and administering physiotherapy interventions (pain control, cardiovascular fitness, joint mobility, Motor skill improvement, and strengthening)
- We are evaluating the effectiveness of therapy.
- There are three phases to the care of those with spinal cord injuries;
The function of physical therapy in avoiding respiratory difficulties:
Respiratory performance.
- The most frequent secondary consequences are pneumonia, atelectasis, secretion retention, and Hypoventilation.
- The impairment of the spinal cord related to the neurological degree of the spinal cord injury affects Respiratory function.
- The levels of innervations are C3-5 Diaphragm, C3-8 Scalenes, C5-T1 Pectoralis, T1-11 Intercostalis, and T6-12 Abdominals.
- People with C1-3 tetraplegia need artificial ventilation, however, most people with C4 tetraplegia can Breathe on their own. Despite being able to breathe on their own, people with spinal cord injuries C4 to T12 may still have diminished vital capacity and have trouble raising intra-abdominal pressure.
- Secretion clearance and improved ventilatory procedures should always be a part of physical therapy Interventions. Techniques for clearing secretions include postural drainage and suctioning, as well as Percussions, vibrations, and shaking. Treatments to improve ventilation include abdominal binders, Posture, deep breathing exercises, incentive spirometry, and inspiratory muscle training. Continuous Positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP) are two further medical Devices frequently used to enhance ventilation.
- Launching a respiratory muscle training program
- Instruction on how to use a coughing and blowing apparatus
- Aggressive chest physical therapy
- Patients with spinal cord injuries can lessen their need for artificial ventilation by using a new technique called diaphragm pacing. Promoting neuromuscular plasticity, enhancing respiratory function and Spontaneous diaphragmatic activation, and improving breathing, speaking, and quality of life for persons With spinal cord injuries are further advantages.
The function of physical therapy in guarding against cardiovascular issues:
- Prophylaxis for deep vein thrombosis (DVT): early limb mobilization, intermittent compression
- Management of bradycardia, autonomic dysreflexia, and postural hypotension
The function of physical therapy in avoiding musculoskeletal complications
- Consider the joints in your ankle, knee, hip, and shoulder to allow for wheelchair positioning, bed mobility, Transfers, and dressing (ankles, knees, shoulders, hips) to prevent lower and upper extremity Contracture.
- Encourage wrist extension in C6 spinal cord injury patients and elbow extension in C5/6 spinal cord injury Patients.
- Inform patients about the best sleeping and wheelchair positions for easing spasticity
- Encourage proper posture by placing one cushion under the neck or none at all while lying flat, and make An early assessment for wheelchair seating and alignment.
- The patient should be in pronation with their fingers extended and their wrists flexed. The position for Functional shortening of the long finger flexors to promote tenodesis grip.
Due to immobility and improper placement, reduced ROM can cause contractures as well as an increase in Tone and spasticity.
Passive stretching, placement in the lengthened posture, and other standard hypertonic treatment methods Like compression, heat, and continuous deep pressure should all be used in the course of treatment.
Maintaining and enhancing innervated muscles
Clinical studies have shown that functional strength training and progressive resistance training are effective Methods for keeping innervated muscle groups strong and healthy.
Defending against Pressure Ulcers
When resting supine, the occiput, scapulas, sacrum, and heels are vulnerable areas for pressure ulcers. While the malleoli and greater trochanter are more prone to side
Interventions in the acute period include passive pressure treatment, such as routine rolling and mobilizing, As well as sufficient skin hydration, nutrition, and monitoring.
Later, during the sub-acute & long-term phases, people will learn how to regularly self-lift objects to reduce Strain.
The importance of physiotherapy in bed transfers and mobility
C6 and below level 5 motor abilities can be acquired after spinal cord damage;
- Using momentum to move
- Moving from lying flat to long-sitting
- Short- and Long-Term Unsupported Sitting
- Vertically lifting
- Transfers
These five motor abilities can still be used with certain changes even though C6 tetraplegia presents some Difficulties. Rolling requires C6 tetraplegia to rotate their shoulders and swing their arms outside Their bodies rather than overhead.
C6 tetraplegia should externally rotate their shoulders and lock their elbows in extension while sitting Unsupported to keep their balance. Individuals with C6 tetraplegia may be able to elevate themselves Vertically by passively extending their elbows, externally rotating their shoulders, and depressing their Shoulders to bear weight with their hands placed anterior to the pelvis.
Physiotherapists can assist patients with spinal cord injuries in avoiding UTIs and overfilling their Bladders by:
- Patient’s being urged to drink enough water
- Working with an occupational therapist to determine the best tools (a wheelchair cup holder with a cup And a long drinking straw) to enable independent hydration
- Maintaining the catheter off the floor while receiving treatment, and adhering to aseptic standards with Catheter care
- Keeping to the plan to perform catheterizations on time
Mobility in a wheelchair
- Tetraplegic patients with C1-4 need powered WCs. These wheelchairs can be operated with head Motions, chin movements, and sip-and-puff actions.
- The most prevalent usage of powered WCs operated by hand movement is for those with C5 tetraplegia.
- The majority of people with C6–8 tetraplegia can move around independently using a manual WC; However, they may also use a hand-controlled WC.
- With a manual WC, people in particular those with spinal cord injuries lower than C8 will be able to move Around independently.
- Those with SCI need to be introduced to their new mode of mobilization. To maintain safe & independent Mobility, it’s crucial to practice turning, opening & closing doors, climbing stairs, moving around & over Obstacles, and moving indoors & outdoors.
- The latest study’s findings imply the necessity for the structure and content of future fall prevention efforts For wheelchair users. Participants with SCI forecast the importance of initiatives to avoid falls that go Beyond the ones now provided. By gathering input from community-dwelling wheelchair users with spinal Cord injuries, additional study is needed to assess the effectiveness of particular fall prevention efforts.
Gait and posture
- The three types of physical treatment that were used the most frequently on patients with AIS D spinal Cord injuries were gait training, strengthening exercises, and balancing exercises. Across all severity Levels & types of spinal cord injury, general strengthening was the most frequent group therapy activity.
- The ability to stand and walk depends on a variety of conditions, but even if independent standing is Unlikely to ever be possible, standing has several advantages. Orthostatic hypotension, bone mineral Density, spasticity, emotional well-being, and bladder and bowel function are all advantages. Using aids Like tilt tables, standing toilets, and/or standing frames, one can stand up. Those who have paraplegia Could have the strength to use knee extension splints or orthoses to stand on parallel bars.
- Using orthoses and walking aids like knee-ankle-foot, hip-knee-ankle-foot, and total paraplegia to partial Paralysis of the lower extremities, gait training is possible.
- The management of pain and cardiovascular fitness are additional crucial components of rehabilitation.
Phase of Subacute Care (Rehabilitation)
- The optimum place to address the rehabilitation needs of people with spinal cord injuries is a specialized Spinal Cord Injury Unit, however, rehabilitation frequently gets started in an acute care hospital while the Patient is awaiting transfer to a spinal injuries unit. During rehabilitation, the whole person must be considered, including their physical, psychological, occupational, and social backgrounds.
- The International Classification of Functioning, Disability, and Health (ICF) includes several domains, Including body function and structure, activity limitation, and participation, and physiotherapy is a crucial Part of the rehabilitation process after spinal cord injury. Many interventions are aimed at preventing rather Than treating impairments, activity limitations, and participation restrictions. The primary management Focus has shifted to Quality of Life, which includes engagement in the community, productive work, Interpersonal connections, and leisure activities.
Long term Phase
- Depending on the severity and type of the lesion, people with spinal cord injuries may have a wide range Of complex needs and long-term limitations in their ability to live independently, drive or use public transportation, go back to work or school, and engage in recreational and social activities. Coordinated Community rehabilitation programs and long-term support are necessary to fulfill the long-term & and Ongoing needs of people with spinal cord injuries to ensure successful long-term management. To coordinate care post-initial rehabilitation and ensure continued tailored case management for Patients with complicated or ongoing needs, best practices in long-term management include active case Management with case managers who have the necessary training, clinical skills, and knowledge of Services.
- Low self-efficacy of the patients/family members appears to be a risk factor for accommodation problems In people with spinal cord injuries, according to a prospective longitudinal study, which points to the need For webbing of cases and their family members’ efficacity to help particular and family adaptation Problems.
Treatment during the phase of rehabilitation includes:
- To create an integrated procedure that is patient-centered, thorough, and coordinated
- Early intervention & and management to address physical motor functional tasks in order to address Subsequent difficulties
- To increase a person’s independence in daily tasks like washing, eating, dressing, grooming, and mobility
- To achieve functional independence, whether verbal or physical tools to support this independence
- To achieve and maintain successful community reintegration.
- Physiotherapists use a variety of remedial ways grounded on the inflexibility and kind of the injury Throughout recovery. For patients with high levels of tetraplegia, range of motion/stretching, Strengthening, and transfers were the three most frequent therapeutic activities; for patients with low levels of tetraplegia, transfers took up more time than strengthening.
- Similar to this, transfers were the most popular individual physiotherapy exercises among paraplegic Patients, followed by a range of motion/stretching and strengthening.
- It’s crucial for physiotherapists to comprehend which functions are achievable and pertinent to the level of Spinal cord injury because people with varying levels of SCI do various motor tasks differently. To complete Jobs flawlessly, all motor tasks should be broken down into smaller tasks. Individuals must Possess the necessary strength, balance, range of motion (ROM), knowledge, or skill related to a Particular motor Activity in order to perform motor tasks successfully. Through consistent, progress-Oriented training, all These aspects are attainable.
The physiotherapist can participate in the extra activities listed below to help prevent Gastrointestinal coexisting:
- Help with bowel routine to avoid constipation and avoid abdominal distension
- To balance intake with exercise level, provide education.
- Patient education for obesity prevention
- Monitors calorie counts
- Getting Ready for the Job
Early physiotherapy therapies introduced during the acute period of spinal cord injury rehabilitation Should concentrate on the following functions:
- Teaching trick motions for people with C5/6/7 spinal cord damage, such as tenodesis grasp and elbow Extension without triceps
- Enhancing the function of partly and fully innervated muscles
- Facilitation of paralyzed and weak muscles
- Preserving complete joint range of motion
- Inform patients about how to carry out daily tasks and the value of muscular strengthening, posture, and Skill development for vision.
- Inform patients about their condition, potential side effects, expected duration of stay, and desired Outcomes. As patients are not always prepared to hear the information offered, this requires frequent Repetition.
- Verify that the patient has the cognitive abilities necessary for the educational task or level being Delivered. For those who cannot read, pictures should be provided. Language (mother tongue or Competent translator) and education should be matched to the patient’s educational level.
- Helping to control spasticity
Functional Strategy
The following guidelines should be taken into account by the clinician while directing a patient’s functional Ability:
- Treat the afflictions
- Instead of concentrating on the patient’s usual functional levels (such as rolling before sitting up), pay attention to their current abilities.
- Activities can be used as an exercise
- Recognize all the elements of an activity that a patient needs to perform a certain function.
- Divide projects into manageable chunks and go to work on them.
- Range of motion maintenance, strengthening, and stretching are essential for optimal performance.
- Utilize the encouragement of the patient’s peers.
- Make patients feel like they accomplished something during a session by concluding with a skill or activity They enjoy.
- To improve or smooth out the function, the following resources might be used:
- To aid in mobility, tilt tables, standing frames, parallel bars, long-leg orthoses, treadmills, and Lokomats Are used.
- Functional Electrical Stimulation (FES) is used to help muscles regain function.
What does spinal cord injury prevention entail?
This guidance could lessen the possibility of a spinal cord injury:
- Drive carefully. One of the most frequent situations that might result in spinal cord damage is car Accidents. Every time you are in a moving car, buckle up.
- Make sure your kids use a child safety seat that is suitable for their age and weight or a seat belt. Children Under the age of 12 should always ride in the rear seat to protect them from airbag injuries.
- Before diving, check the water’s depth. Don’t dive into an above-ground pool unless it is at least 12 feet (Approximately 3.7 meters) deep, and never dive into water if you don’t know how deep it is.
- Avoid falling. To reach elevated objects, use a step stool with a grab bar. Place railings on the stairs. Install non-slip mats in the shower or hogshead and on pipe flooring. Use safety gates to restrict stairs for Young children, and think about putting window guards.
- When participating in sports, use caution. Wear any safety equipment that is advised. In athletics, refrain From taking the initiative. For instance, in baseball and football, avoid sliding headfirst and tackling with The top of the helmet. Use surveillance to look for new gymnastics moves.
- Never drink and drive. Driving while intoxicated or under the influence of drugs is not advised. Don’t ride With a motorist who has consumed alcohol and is operating a vehicle.
FAQ
Spinal cord physiotherapy is a type of physical therapy that helps people who have suffered a spinal cord injury to improve their function and quality of life. It is a complex and lifelong process that requires A multidisciplinary approach, involving physiotherapists, doctors, nurses, and other healthcare Professionals.
The specific requirements for spinal cord physiotherapy will vary depending on the individual’s injury Level, completeness, and other factors.
Swedish massage works to relax the soft tissues by repeatedly using lengthy strokes, kneading, and Elongating motions to loosen the tissues and improve blood flow.
While you are sleeping, let your spine actually relax
Exercise your core to strengthen your back and abs
Enjoy the advantages of massage
When sitting, use excellent ergonomics and try to keep your sitting duration to a minimum.
Natural Treatments for Spinal Cord Injury Pain Acupuncture. Acupuncture focuses on particular body Regions, and doctors are finally acknowledging how it might help with spinal cord damage and long-term pain management
Vitamins and dietary supplements
Aromatherapy
Massage treatment
Yoga.
Within a month, more than 90% of individuals with lumbar muscular strains or sprains are fully Recovered. Unexpected flare-ups of low back pain should be managed at home with “as needed” heat And ice therapy in addition to anti-inflammatory medications.
Reference
- P. (2022, October 23). Spinal cord. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/spinal-cord-anatomy/
- V. (2022, January 28). The spinal cord. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/the-spinal-cord/
- Hirpara, D. (2023, February 14). Spinal cord injury. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/spinal-cord-injury/
- Spinal cord. (2023, October 4). In Wikipedia. https://en.wikipedia.org/wiki/Spinal_cord
- Spinal cord anatomy. (n.d.). Physiopedia. https://www.physio-pedia.com/Spinal_cord_anatomy
- Spinal cord | Nerves, Reflexes, Pathways. (2023, September 15). Encyclopedia Britannica. https://www.britannica.com/science/spinal-cord



9 Comments