Deep Vein Thrombosis (DVT)
Table of Contents
What is Deep Vein Thrombosis (DVT)?
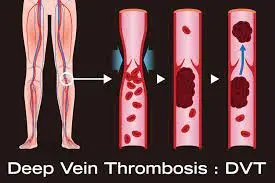
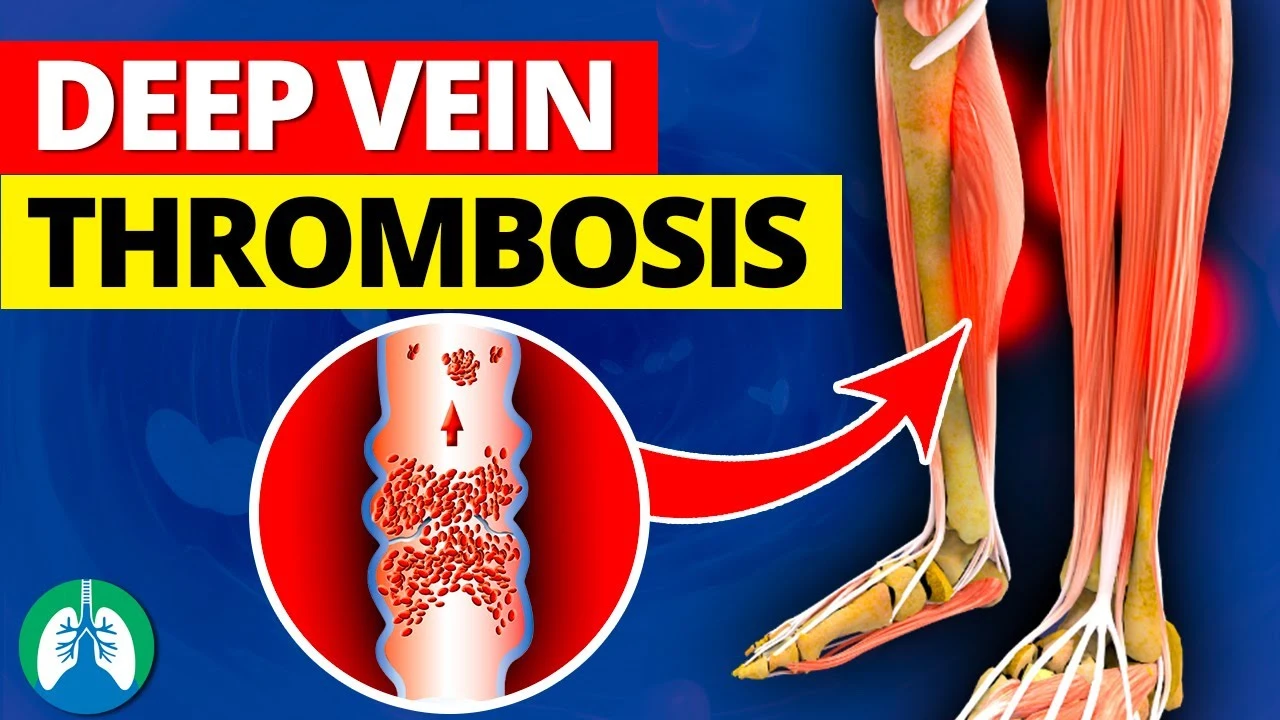
Deep vein thrombosis (DVT) refers to the formation of blood clots (thrombi) in deep veins, typically in the legs. It is a serious medical condition that can potentially lead to life-threatening complications if not diagnosed and treated promptly.
Medicines, compression stockings, and surgery are all forms of treatment. Do not rush. For two years, you might need to wear compression stockings in addition to taking medication for a few months.
When a thrombus (blood clot) forms in deep bodily veins due to a vein injury or prolonged blood flow, it is referred to as deep vein thrombosis (DVT), also known as venous thrombosis. Your vein may be entirely or partially blocked by the blood clots. The lower leg, thigh, or pelvis are where DVTs typically develop, although they can also happen in the arm, brain, intestines, liver, or kidney.
Danger of DVT
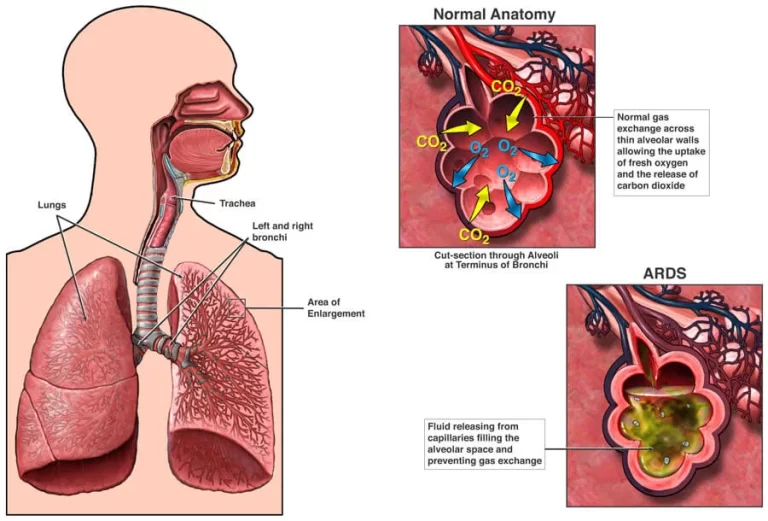
Although DVT is not lethal, blood clots can still escape and travel through your body. When circulating blood clots (emboli) get stuck in the blood vessels of your lung, it results in a pulmonary embolism (PE). You require an immediate diagnosis and course of treatment since this ailment may be life-threatening.
When a DVT occurs in the legs, up to 50% of patients experience sporadic limb discomfort and swelling that might linger for months or even years. When the veins’ valves and inner lining are harmed, blood “pools” more than it should, leading to the development of the disease known as “post-thrombotic syndrome.” This causes swelling and discomfort by raising the pressure inside your veins.
Characteristics of this condition
- bleeding in a pool.
- leg swells continuously.
- your veins are under more pressure.
- discoloration or increased pigmentation of your skin.
- Leg ulcers, also known as venous stasis ulcers, are common.
How frequent is Deep Vein Thrombosis (DVT)?
Up to 300,000 individuals each year in the United States die as a result of DVT or PE, with 1 to 3 in every 1,000 developing a DVT or pulmonary embolism each year. After strokes and heart attacks, it is the third most prevalent vascular disease. Any age can experience acute DVT or PE; however, it is more prevalent in those over 60 and less common in children and adolescents. Having surgery or being admitted to the hospital due to a medical condition accounts for more than half of all DVTs.
When to see a Doctor?
Contact your doctor as soon as you get DVT symptoms.
Seek immediate medical attention if you experience any of the life-threatening signs of a pulmonary embolism (PE), a deep vein thrombosis complication.
The signs and symptoms of a pulmonary embolism include the ones listed below:
- sudden Dyspnea (breathlessness)
- Chest discomfort or pain that gets worse when you breathe deeply or when you cough
- feeling faint or disoriented
- Fainting
- fast heartbeat
- quickly breathing
- exhaling blood
- Leg or arm swelling (this can occasionally happen quickly).
- Your arm or leg may only feel sore or painful when you’re standing or moving about.
- Your arm or leg may feel warmer than normal where it aches or is swollen.
- reddish or discolored skin.
- Your skin’s surface may have larger-than-average veins.
- When blood clots impact the deep abdominal veins, you may experience flank discomfort in addition to abdominal pain.
- severe headaches (often with a quick start) and/or seizures (caused by blood clots in the brain’s veins).
- Some individuals don’t realize they have a DVT until a blood clot in their arm or leg travels to their lungs. Acute PE symptoms include chest discomfort, shortness of breath, bloody cough, and dizziness.
If you experience DVT symptoms, you should contact your doctor immediately or visit the emergency department. Do not hold off on treating your symptoms. To avoid major problems, get treatment soon.
Why does Deep Vein Thrombosis (DVT) occur?
These ailments can make you more vulnerable to developing deep vein thrombosis:
- Your risk of blood clots is increased if you have an inherited (genetic) disorder.
- Having cancer and undergoing chemotherapy, among other therapies.
- a history of deep vein thrombosis either personally or genetically.
- a deep vein that is incapable of pumping blood because of an injury, surgery, or immobilization.
- Being motionless after surgery or a major injury or not moving for extended periods of time when traveling in a car, truck, bus, rail, or airline
- being a new parent or expecting a kid.
- having a DVT despite being older than 40 (any age might be affected).
- being overweight or obese.
- a condition characterized by an autoimmune illness such as lupus, vasculitis, or Crohn’s Disease (inflammatory bowel disease).
- making use of tobacco products
- a varicose vein condition.
- using hormone treatment or birth control tablets.
- having a pacemaker or central venous catheter.
- posses COVID-19.
Risk factors
Deep vein thrombosis (DVT) risk might rise as a result of several factors. Your risk of DVT increases as your risk factors increase. DVT risk factors include:
- Age. DVT risk is higher in people over 60. DVT, however, can happen at any age.
- Nothing is moving. The calf muscles do not tighten (contract) while the legs are immobile for a prolonged period of time. The contraction of muscles promotes blood flow. DVT risk is increased by sitting for an extended period of time, such as when driving or flying. Long-term bed rest, which can be brought on by a protracted hospital stay or a health condition like paralysis, also has negative effects.
- Surgery or injury. The risk of blood clots might be raised by surgery or vein injury.
- Pregnancy. The pelvic and leg veins experience increased pressure during pregnancy. Up to six weeks after a baby is born, a pregnant woman is still at risk for blood clots. Particularly vulnerable are those who have hereditary clotting disorders.
- oral contraceptives, such as hormone replacement therapy or birth control pills. Both can make the blood more likely to clot.
- obesity or being overweight. The pressure in the veins in the pelvis and legs is increased by being overweight.
- Smoking. Smoking has an impact on blood flow and clotting, which can raise the danger of DVT.
- Cancer. Certain malignancies produce an increase in blood clotting proteins. Some cancer treatments can raise the chance of blood clots.
- cardiac arrest. DVT and pulmonary embolism risk are both increased by heart failure. The symptoms brought on by even a modest pulmonary embolism are more obvious in persons with heart failure because the heart and lungs don’t function adequately.
- intestinal inflammation. DVT risk is increased by Crohn’s disease or ulcerative colitis.
- a history of PE or DVT in oneself or one’s family. You may be more susceptible to having DVT if you or a member of your family has experienced one of these disorders.
- Genetics. Some individuals have DNA alterations that make blood clot more quickly. Factor V Leiden is one illustration. One of the blood’s clotting components is altered by this genetic condition. Blood clots may not always result from a hereditary condition.
There are situations when a blood clot in a vein develops without any obvious risk factors. An unprovoked VTE is what this is.
How is DVT identified?
Your medical professional will do a physical examination and go over your medical background. Imaging tests are also required.
DVT diagnostic tests
ultrasonography of the veins. Due to its availability and non-invasive nature, this test is the most often used to identify DVTs. In this examination, ultrasound waves are used to display blood flow and blood clots in your veins. While scanning your arm or leg using a vascular ultrasound machine, pressure is applied. If the pressure doesn’t cause your vein to contract, there may be a blood clot present. If the duplex ultrasound results aren’t clear, your doctor may utilize another type of imaging.
Venography. In this invasive test, your doctor will numb the skin on your neck or groin and inject a specific dye (contrast material) into your veins using a catheter to check for any blood clots that may be partially or totally obstructing blood flow there. Venography is rarely used today, but it is sometimes necessary.
either magnetic resonance venography (MRV) or magnetic resonance imaging. Images of the organs and bodily organelles are shown during an MRI. Pictures of the veins in particular parts of your body are displayed by MRV.
A computed tomography (CT) scan is a form of X-ray that reveals inside body features. An abdominal, pelvic, or brain DVT, as well as pulmonary embolisms, may be discovered by your doctor using a CT scan.
Special blood tests may be required if your doctor suspects you have a hereditary or acquired clotting issue. This might be crucial if
Your doctor is unable to determine another explanation for the blood clots you’ve had in the past.
You have a blood clot in a strange place, such as a vein in your intestines, liver, kidney, or brain.
Blood clots run in your family quite strongly.
There is a known genetic clotting issue in your family background.
Treatment of Deep Vein Thrombosis (DVT)
Because DVT can develop following a significant fracture or surgery, many patients are already in the hospital when the illness is identified. The objectives of DVT therapy are to:
- Prevent the blood clot from expanding.
- Prevent the clot’s fragment from escaping and making its way to the lungs, where it can cause a pulmonary embolism.
- lessen the likelihood of getting another clot
- and reduce the possibility of generating further issues
- DVT is often treated nonsurgically.
Nonsurgical Treatment
Anticoagulants. Anticoagulants are blood-thinning drugs that help dissolve existing clots and prevent new clots from forming as part of nonsurgical therapy. As soon as a clot is identified, anticoagulant drugs are started.
Anticoagulants must be used carefully, whether you are in the hospital or at home since if the dosage is too high, it might lead to bleeding issues. Your doctor may want frequent blood tests to monitor how quickly your blood clots, depending on the medicine you’re taking. Make sure your blood medication level is high enough to prevent blood clots but not so high that it results in excessive bleeding.
Heparin, low molecular weight heparin (LMWH), Xa inhibitors, and warfarin (Coumadin) are the most commonly used anticoagulants to treat DVT.
inhibitors of Xa. These more recent anticoagulants are taken by mouth. They don’t need dosage adjustments, don’t require blood test monitoring, and are simple to apply. They are frequently recommended as a consequence.
Heparin. Heparin or LMWH therapy may be used as the first line of DVT treatment. While LMWH is administered via subcutaneous injection beneath the skin, standard heparin is administered intravenously (into a vein). LMWH has a brief half-life and leaves the body in under 12 hours. Dosage is determined by body weight. In contrast to normal heparin, which often changes dosages based on clotting times, each dose is the same for most individuals.
LMWH can be administered on an outpatient basis because it doesn’t need an intravenous line or dosage monitoring. Either a visiting nurse administers the injections or the patients administer the shots themselves.
Warfarin. Warfarin is often administered orally for 3 to 6 months after heparin or LMWH treatment. Warfarin takes between 4 and 5 days to achieve its peak potency and at least 36 hours to begin functioning. This is why heparin and warfarin are both administered at the beginning of therapy; heparin safeguards the patient by keeping blood anticoagulant until warfarin “kicks in.” Because Xa inhibitors do not require regular blood testing as warfarin does, warfarin has become less popular since the development of Xa inhibitors. Every form of anticoagulant has advantages and disadvantages. The optimal prescription for you will be discussed with you by your doctor.
Serial ultrasonography and observation. Depending on your personal risk factors, your doctor may choose to use serial duplex ultrasound scans for observation and monitoring rather than anticoagulant treatment to treat an isolated DVT below the knee or in the calf.
Thrombolytics. Your doctor could advise utilizing thrombolytics in particular circumstances. These clot-dissolving drugs are only used when there is a very high risk for pulmonary embolism and are delivered via a catheter straight into the blood clot.
Surgical Treatment of Deep Vein Thrombosis
The major vein leading to your heart may be surgically inserted with a tiny device known as a vena cava filter if anticoagulants are unable to prevent your blood clot from growing or if you have a medical condition that prevents you from taking anticoagulation drugs. Before they may travel through your bloodstream and create a pulmonary embolism by reaching your lungs, most blood clots will be caught by this filter. Rarely, a blood clot in the veins or lungs may require surgery to be removed.
Activity Guidelines
Your mobility may initially be hampered by a DVT due to leg discomfort and edema. However, you’ll be able to gradually resume your regular activities. If your legs feel sluggish or swollen, lie in bed with your heels up by 5 to 6 inches. This reduces edema and enhances circulation.
In addition
- If you spend a lot of time sitting immobile, work your calf muscles.
- Every hour while awake, especially on a lengthy flight or road journey, get up and take a little stroll.
- Put on a pair of knee-high compression socks. If worn every day, they reduce leg discomfort and edema by at least 50%.
- Avoid engaging in activities that might seriously hurt you.
- Always stay hydrated, but more so when traveling.
What therapies are accessible to sufferers of deep vein thrombosis?
A hospital stay may be necessary for some DVT patients to receive treatment. Some people could qualify for outpatient care.
Compression stockings, elevating the afflicted leg(s), and taking anticoagulant drugs (blood thinners) at certain points during the day are all forms of treatment. In rare instances, when the DVT is severe, intrusive procedures (catheter-based operations) may be needed.
The primary objectives of therapy are to:
- Avoid preventing the clot from expanding and affecting other veins.
- Stop the clot from separating in your vein and traveling to your lungs.
- minimize the possibility of another blood clot.
- Prevent the blood clot’s long-term side effects, such as chronic venous insufficiency.
- Important details about prescription drugs
- Take your medications precisely as prescribed by your doctor.
- Follow all planned laboratory appointments and submit to any blood tests your doctor prescribes.
- Never change your pharmaceutical regimen, including over-the-counter drugs and dietary supplements, without first seeing your doctor.
- Disclose your diet to your healthcare provider. Depending on the medicine you take, you might need to alter it.
DVT treatments
Blood-thinning agents (anticoagulants)
The blood clotting process is hampered by this kind of drug. Anticoagulants also block blood clots from growing larger and migrating. Anticoagulants do not “melt” or eliminate blood clots. Clots may be broken up by your body on their own, but occasionally they don’t totally go away. If not, they often diminish and transform into tiny “scars” inside your veins. These “old” clots can occasionally cause leg edema, although they frequently have no symptoms.
There are several forms of anticoagulants, including oral Xa inhibitors, heparin, and warfarin. The ideal sort of medication for you will be discussed with you by your doctor.
If you need to take an anticoagulant, you might only need to do so for a short period of time (often three to six months), or you could need to continue doing so continuously. The length of your therapy may vary based on the unique circumstances of each person, such as if:
Clots are nothing new to you.
You’re receiving therapy for a different condition, such as cancer or an autoimmune disease (if you have an increased risk of blood clots, you may need to take an anticoagulant).
Compression Stockings
Graduated elastic compression stockings will probably be necessary to reduce or eliminate leg edema. This swelling is typically brought on by damage to the tiny valves inside your veins. As a result of the DVT obstructing blood flow in your vein, you can also experience edema. Most people use compression stockings just below the knee. As they move away from your ankle, these stockings loosen up around it. Your leg feels a little compressed as a result. Some patients have up to two years to utilize them. Compression stockings reduce leg discomfort and swelling by at least 50% when worn every day from dawn to night (but they don’t have to be). This is according to several clinical investigations.
After surgery, your healthcare providers could put compression devices on your calves to create pressure. While you are laying in bed, these machines squeeze and release the fabric-covered devices around your calves. If you’re in the hospital, these devices can help avoid a DVT, but they are not recommended for use outside of the hospital. Additionally, you shouldn’t use these devices for DVT prevention if you already have a DVT, in contrast to compression stockings that you may use with safety while a leg DVT is present.
DVT Treatment Procedures
A surgeon may need to perform an operation to implant an inferior vena cava (IVC) filter if you are unable to take blood-thinning drugs or if blood clots develop when you are taking blood thinners without missing doses. The IVC filter is implanted by your surgeon by a catheter into a big vein in your neck or groin, which is then sent into your vena cava, the largest vein in your body. The IVC filter is intended to stop big blood clots (emboli) from reaching your lungs and creating a pulmonary embolism if blood clots in your leg veins break off and travel. Although a pulmonary embolism can be avoided with the use of an IVC filter, additional blood clots can still develop.
Complications of Deep Vein Thrombosis
DVT complications may include:
PE, or pulmonary embolism: It happens when a blood clot (thrombus) from the leg or another part of the body dislodges and lodges in a blood artery in the lung.
Get medical attention right once if you get PE symptoms. They include chest pain while coughing or breathing in, quick breathing, rapid heartbeat, feeling dizzy or faint, and coughing up blood.
syndrome after phlebitis. The blood clot’s damage to the veins lowers blood flow in the afflicted locations. Leg discomfort, swelling, skin changes in color, and sores are some of the symptoms.
difficulties with treatment. DVT is frequently treated using blood thinners. Blood thinners can have dangerous adverse effects, including bleeding (hemorrhage). While using blood-thinning medications, it’s crucial to get routine blood testing.
Prevention
What can I do to lower my risk?
You should take the following steps to lower your chance of developing another DVT or PE clot:
taking your medications precisely as directed by your doctor.
observing your doctor’s and the lab’s follow-up visits. These inform your healthcare practitioner about the efficacy of your treatment.
altering one’s way of life by giving up smoking and adopting a healthier diet and exercise habits.
If you have a higher chance of having a DVT but have never had one, be sure to:
If you must remain stationary for an extended period of time, stretch your calf muscles. Get up and walk at least once every 30 minutes if you’re on a long trip. Or, if you’re on a lengthy road trip, get out of the vehicle every hour.
After being ill or having surgery, get out of bed as soon as you can and start moving about. The sooner you begin moving, the lower your risk of getting a DVT.
Use compression stockings or take medication after surgery if your doctor advises it to reduce your risk of blood clots.
Follow up with your healthcare practitioner as instructed, and do what they advise.
Deep vein thrombosis may be prevented with lifestyle modifications. Try the following tactics:
Get your legs moving. Try to get up and about as soon as you can if you have had surgery or were placed on bed rest. Never sit with your legs crossed. This may inhibit blood flow.
When you’re on the road, stop frequently to stretch your legs. Get up and move around sometimes while flying. If you’re driving, stop every hour or so and go for a walk. Exercise your lower legs if you are unable to walk. Keep your toes on the ground while raising and lowering your heels. Then, while maintaining your heels on the ground, lift your toes.
Avoid smoking. DVT risk is increased by smoking.
Manage your weight. DVT is at risk due to obesity. The chance of blood clots is decreased by regular exercise. As a general rule, strive to get in at least 30 minutes of moderate physical activity each day. If you want to lose weight, keep it off, or achieve certain fitness goals, you might need to exercise more.
Prognosis
You must continue taking blood thinners as directed and wearing compression stockings until your healthcare professional instructs you to cease doing so since a DVT can take many months to a year to dissipate. To ensure you’re receiving the proper dosage of blood thinners, you might require blood tests. In order to determine if your blood clot is improving, moving, or staying in the same location, your doctor may order further ultrasounds in the future.
FAQs
Laying flat on your back while extending the knee in the suspicious leg is known as the Homan’s Test. Squeeze the calf while having a friend or family member elevate the outstretched leg to a 10-degree angle. DVT could be present if there is severe calf discomfort.
DVT can occur at any age, even though it is more frequent in persons over 60, especially if you have any health-related risk factors. If you are overweight or obese, have a family history of deep vein thrombosis, pulmonary embolisms, or clotting abnormalities, or if you smoke, you run a higher risk of having a deep vein thrombosis.
Blood clots can develop when the veins’ blood flow stops or is obstructed. Having one or more of these risk factors increases your likelihood of developing DVT: becoming sedentary as a result of prolonged bed rest or prolonged periods of inactivity, such as when traveling. blood clots run in the family.
Anticoagulants, a kind of medication, are the primary therapy for DVT. Anticoagulants stop both the growth of the current blood clot and the formation of future blood clots. Usually, you’ll need to continue taking them for at least three to six months.
One of the best strategies to avoid DVT is regular exercise. Exercise lowers your risk by assisting you in maintaining a healthy weight, enhancing circulation, building muscle, and improving lung function.
95 percent of deep vein thromboses that develop in the prominent veins above the knee are effectively detected by duplex ultrasonography. The big veins above the knee may be used by duplex ultrasonography to identify DVT, and if the test is positive, no more testing is required before treatment can begin.
Age. After 60 years of age, DVT risk increases.
lack of movement When the legs are stationary for a prolonged length of time, the calf muscles do not contract (squeeze).
injury or operation.
Pregnancy.
Oral contraceptives or hormone replacement therapy are available for contraception.
being fat or overweight.
Smoking.
Cancer.
a few medications, including erythropoietin, tamoxifen, thalidomide, birth control pills, hormone replacement therapy, and cancer chemotherapeutic medicines. When one of these drugs is used in combination with other risk factors, the chance of a blood clot is considerably elevated.
About 6% of DVT cases and 12% of pulmonary embolism cases end in death within a month after diagnosis. Early mortality following venous thromboembolism is significantly correlated with advanced age, underlying cardiovascular disease, malignancy, and pulmonary embolism upon presentation.





8 Comments