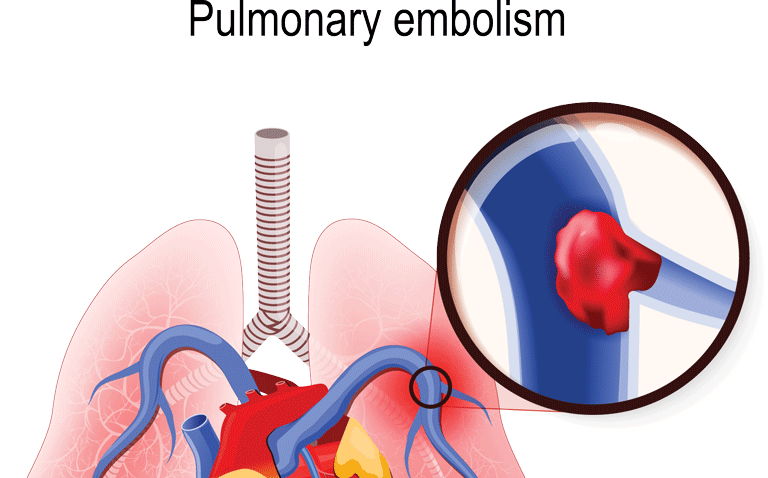
Pulmonary Embolism
Table of Contents
What is a Pulmonary Embolism?
Pulmonary embolism (PE) is a potentially life-threatening medical condition characterized by the blockage of one or more blood vessels in the lungs. It occurs when a blood clot, usually formed in the deep veins of the legs (a condition known as deep vein thrombosis or DVT, travels through the bloodstream and becomes lodged in the arteries supplying the lungs.

When a blood clot gets lodged in a lung artery and prevents blood flow to a portion of the lung, it causes a pulmonary embolism. Most frequently, blood clots begin in the legs and move up the right side of the heart before entering the lungs. Additionally known as deep vein thrombosis
A pulmonary embolism is an obstruction of one of the pulmonary arteries in the lungs. In many cases, a deep venous thrombosis forms in the leg. The thrombus becomes dislodged and travels to the lungs, blocking the pulmonary artery. The condition is a medical emergency that needs prompt diagnosis and treatment to ensure patient survival.
A pulmonary embolism is a blood clot that blocks and prevents blood flow to the artery in a lung. In many cases, the blood clot begins in a deep vein in the leg and moves to the lungs. Rarely does the clot form in a vein in another part of the human body. DVT is the term for a blood clot that develops in one or more deep veins in the body. A pulmonary embolism can be fatal because one or more blood clots prevent blood from reaching the lungs. Taking action to prevent blood clots in the legs will assist protect against pulmonary embolism, even though quick treatment considerably reduces the chance of mortality. If a person has a pulmonary embolism, their blood oxygen level will be lower than normal. A pulse oximeter is usually attached to the finger and measures the blood oxygen saturation level using red and infrared light via the tissue in the finger. A blood oxygen saturation level of less than 90 percent is unusual.
Pathological Process
Stasis in the deep veins, especially at the calf, causes thrombus development. The initial cardiorespiratory condition of the patient, as well as the size and quantity of emboli, influence how severe alterations in pulmonary blood flow and respiration are. A modest pulmonary artery blockage may not cause symptoms, but a massive embolus can be deadly.
In the second scenario, pulmonary embolism results in wasted ventilation by increasing alveolar dead space, which produces a mismatch between ventilation and perfusion as well as an increase in pulmonary artery pressures and right ventricular effort. As a result of a reduction in blood volume and coronary perfusion to the left ventricle, right heart failure eventually occurs, followed by left heart failure. The heart stops pumping blood as a result of cardiac muscle failure.
Rarely, non-thrombotic substances such as air, fat, amniotic fluid, bone, and organ pieces can obstruct the pulmonary artery.
Prevalence/Incidence of PE
PE is the third most common cause of cardiovascular mortality, behind myocardial infarction (MI) and cerebrovascular accidents (CVA). Asymptomatic patients with distal DVT make up 71.4% of patients with PE and up to 2.6% of those with PE. According to European recommendations for the diagnosis and treatment of PE, venous thrombosis and PE have yearly incidence rates of between 0.5 to 1.0 per 1000 people. A 2005 Swedish research found a nationwide incidence of 0.6/1000/year.
Risk Factors
Blood clots, or thrombi, are brought on by hypercoagulation. Typical risk elements include the following:
- serious limb damage, surgery, extended bed rest, and prolonged standing posture of the lower limbs for longer than six hours
- Injury to the spinal cord and trauma
- Smoking
- using oral contraceptives
- replacement treatment for hormones
- Cancer
- Chemotherapy
- pregnancy during the postpartum phase older age (over 40)
- Cast or immobilizer
- catheterization of the central vein
- The risk of a fat embolism is increased by being overweight and having high cholesterol.
Even while anybody may get blood clots that cause pulmonary embolisms, several things can make you more likely to do so.
History of blood clots
If you or any of your blood relatives, such as a parent or sibling, have previously experienced venous blood clots or a pulmonary embolism, you are at a higher risk.
Medical conditions and treatments
You are at risk for certain medical illnesses and treatments, including:
- Heart illness. Clot development is more probable in conditions affecting the heart and blood vessels, particularly heart failure.
- Cancer. Blood clot risk can be raised by some malignancies, particularly tumors that have spread, as well as cancers of the brain, ovary, pancreatic, colon, stomach, lung, and kidney. Chemotherapy raises the danger even more. If you take tamoxifen or raloxifene (Evista) and have a personal or family history of breast cancer, your risk of blood clots is also increased.
- Surgery. One of the main reasons why blood clots become problematic is surgery. That’s why medicine that helps to prevent clots may be used both before and following major surgery, such as joint replacement.
- clotting-related illnesses. Blood is affected by several genetic diseases, which increase the risk of clotting. The likelihood of blood clots can also be increased by other medical conditions, such as renal illness.
- COVID-19 is the coronavirus disease of 2019. Those who have COVID-19 with significant symptoms are more likely to get a pulmonary embolism.
- long stretches of idleness
- Blood clots are more likely to develop during extended periods of inactivity than usual, such as:
- Rest in bed: You run the risk of developing blood clots if you spend a lot of time in bed following surgery, a major illness, a heart attack, a limb fracture, trauma, or any other injury. Long durations of flat-lying cause your veins’ blood flow to slow down, which might cause blood to pool in your legs.
- Long journeys: Long vehicles or airline flights in a confined space restrict blood flow in the legs, which raises the risk of blood clots.
- Other danger elements
- Smoking: Some people, especially those who already have other risk factors, may have an increased risk of blood clots as a result of smoking, for unknown reasons.
- weighing too much. Being overweight increases the chance of blood clots, especially in people who already have other risk factors.
- More estrogen: In women who smoke or are overweight, estrogen from birth control tablets and hormone replacement therapy may cause an increase in blood clotting factors.
- Pregnancy: Blood return from the legs might be slowed by the weight of a baby resting against pelvic veins.
Sign And Symptoms of Pulmonary Embolism
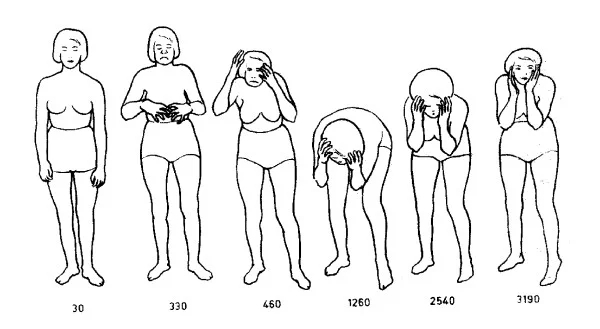
Depending on how much of the lung is affected, the size of the clots, and if you have underlying lung or heart disease, the symptoms of a pulmonary embolism can vary dramatically. Depending on the level of clotting, pulmonary embolism symptoms might differ. Most people who have pulmonary embolisms have symptoms; other people don’t. Common signs of pulmonary embolism include:
- a sudden decrease in lung capacity. Usually, this ailment shows up out of nowhere. Even when you’re at rest, it’s difficult to breathe, and it gets worse when you exercise. whether you were awake or asleep.
- ache in the chest. People could seem to be suffering from heart attacks. When you inhale deeply, the discomfort is typically severe and felt. People may not be able to breathe deeply due to the pain. Additionally, it could be felt when individuals sneeze, bend over, or lean. Sharp discomfort in the jaw, neck, arm, or chest that cannot be explained. The discomfort could potentially resemble heart attack symptoms.
- Fainting. If your blood pressure or heart rate decreases suddenly, you might lose consciousness. We refer to this as syncope.
- either cough out bloody mucous or not.
- blue, pale, or clammy skin.
- Heartbeat (pulse) that is quick.
- excessive perspiration.
- Feeling nervous, dizzy, faint, or passing out sometimes.
- Wheezing.
The signs of a pulmonary embolism typically appear rapidly, so if you see any of the following, call 911 right once.
- a cough that might be bloody
- chest pain or a feeling of weight in the chest.
- feeling ‘light-headed’ or dizzy
- Having back pain
- quick heartbeat
- breathing difficulty
- There is more sweating than normal.
The following are some deep vein thrombosis (DVT) signs and symptoms:
- any spot on the arm or leg that is warm to the touch
- Leg discomfort or soreness, particularly in the calf
- Skin sensitivity on the afflicted leg or arm
- either an arm or a leg swelling
- veins that are bigger than usual in the arm or leg.
The risk of a pulmonary embolism can be reduced by doctors if a deep vein thrombosis (DVT) is identified early enough. If you have any of the aforementioned DVT (deep vein thrombosis) symptoms, you need to consult a doctor very soon. Other signs and symptoms are:
- a cough that occasionally produces blood or blood-stained mucous
- irregular or fast pulse
- dizziness or lightheadedness
- excessive perspiration
- Fever
- Typically at the back of a lower leg, there may be leg discomfort, leg edema, or both.
- Skin that is clammy or discolored, or cyanosis
Depending on the size of the embolus and how much lung tissue is impacted, vital indicators (blood pressure, heart rate, respiratory rate, and oxygen saturation) may be normal or abnormal. The stability of the vital signs decreases with increasing clot burden (or load). Abnormal vital signs may include:
- Tachycardia: elevated heart rate (tachy=fast + cardia=heart);
- Tachypnea: elevated or raised respiratory (breathing) rate (tachy=fast + pnea= breathing);
- Hypotension: decreased or reduced blood pressure (hypo=low + tension=blood pressure);
- Hypoxia: decreased SaO2. Oxygen saturation describes how many hemoglobin molecules are carrying or taking in oxygen. Normal oxygen levels are generally greater than 92%–93%.
The following is how the condition develops:
As the body strives to make up for the lung’s reduced ability to transmit oxygen, the heart rate and respiratory rate may increase. This enables the oxygen that is already there to be circulated more quickly, better meeting the needs of the body’s organs and tissues.
As a result, the body’s organs may get weak and dizzy and experience anxiety. They may also lose the oxygen they require to function.
It could be more difficult for the heart to pump blood via the obstructed pulmonary arteries if the clot burden is significant enough. This increases the amount of work the heart must perform, increasing internal pressures and taxing the heart’s own muscles.
In up to 25% of instances, sudden death is the first indication of a problem. Without any warning signs, the person falls, ceases breathing or is prevented from breathing, and has a cardiac arrest. After coronary artery disease, pulmonary embolism is the second-leading cause of sudden death. Those who experience any pulmonary embolism symptoms should seek emergency medical assistance. Discuss the risk factors with the healthcare practitioner as a blood clot can occur without any symptoms.
Types of pulmonary embolism
According to their severity and location, doctors categorize pulmonary embolisms. The likelihood of significant complications or mortality depends on how severe the pulmonary embolism is. based on a scale of low, moderate, or high. To assess the severity, doctors consider a variety of factors, including:
symptoms
lung performance
blood pressure measurements, oxygen consumption, and the outcomes of imaging tests, particularly echocardiograms
A high-risk case of pulmonary embolism may also be referred to as a “massive” case, and a case of intermediate risk as a “submassive” case. The location of the clot in the lungs is referred to as its location. By site, medical professionals divide pulmonary embolisms into three categories:
- Saddle pulmonary embolism: A clot lodges in the main pulmonary artery, one of its left major branches, or one of its right main branches in a condition known as a saddle pulmonary embolism. A central pulmonary embolism has occurred.
- Lobar pulmonary embolism: A clot becomes lodged in the lobar artery. The left and right major branches of the pulmonary arteries split into two lobar arteries. Each lung has two lobar arteries, which supply three lobes in the right lung and two lobes in the left lung. A central pulmonary embolism also exists here.
- Distal pulmonary embolism: In a segmental or subsegmental artery, a clot lodges in a distal pulmonary embolism. These are the arteries that supply one or more of the lung’s segments. The segment is a lobe’s division. The left lung has eight segments, whereas the right lung has 10 segments. Peripheral pulmonary embolism characterizes this clot.
Types of Pulmonary Embolism
- Acute or chronic pulmonary emboli are two different types of pulmonary emboli.
A recent blockage that causes sudden-onset heart strain is an abrupt pulmonary embolism. Usually, acute pulmonary embolisms have to be treated right away with blood thinners and clot-busting drugs.
A more subtle manifestation, chronic pulmonary embolism, includes heart failure and gradually worsening symptoms. An older residual blockage brought on by an undissolved clot in the pulmonary circulation from a prior acute pulmonary embolism is what leads to chronic pulmonary embolism. An uncommon form of pulmonary hypertension known as chronic thromboembolic pulmonary hypertension (CTEPH) can also result from chronic pulmonary embolism in a tiny proportion of individuals by raising blood pressure in the pulmonary arteries over time.
It is useful to comprehend the term CTEPH (chronic thromboembolic pulmonary hypertension):
A long-lasting ailment, such as one that lasts months or years, is referred to as chronic.
A blood clot, or thrombus, develops in a blood artery in the body and travels via the arms, legs, or a vein into blood vessels in the lungs where it clogs the arteries. This condition is referred to as thromboembolic. Pulmonary embolism (PE) is the name given to a blood clot in the lung.
Lungs are referred to as pulmonary in medical terminology.
Hypertension, which is a medical term for high blood pressure, here refers to elevated blood pressure in the lungs.
Acute Pulmonary Embolism
An abrupt obstruction in the lungs’ arteries is known as an acute pulmonary embolism. The obstruction starts as a clot that moves from a vein somewhere in the body to a lung. After a heart attack and a stroke, acute pulmonary embolism is the third most frequent cause of cardiovascular disease mortality. Without prompt medical attention, between 25 to 30 percent of patients will pass away.
Acute Pulmonary Embolism’s Clinical Presentation
The acute pulmonary embolism clinical presentation is as follows:
- breathing difficulty
- chest discomfort
- irregular or fast pulse
- fainting spells
- Lightheadedness
Chronic Pulmonary Embolism and CTEPH
A chronic pulmonary embolism, also known as an undiscovered or untreated acute pulmonary embolism, is an obstruction of the pulmonary arteries that develops when previous clots in these veins do not disintegrate over time despite treatment for an acute pulmonary embolism. Chronic blood clot buildup may result in the development of scar tissue in the lungs’ blood vessels, which obstructs normal blood flow and forces the right side of the heart to contract more forcefully. Chronic thromboembolic pulmonary hypertension (CTEPH), an uncommon but often curable form of severe pulmonary hypertension (high blood pressure in the blood vessels of the lungs), is the outcome. Despite the prevalence of pulmonary emboli, only 2-4 percent of those who have them develop persistent thromboembolic pulmonary hypertension.
Clinical Presentation of Chronic PE and CTEPH
An example of a persistent pulmonary embolism clinical presentation is
- Breathlessness that is becoming worse with time
- irregular or fast pulse
- fainting spells
- Lightheadedness
- a cough that might result in bloody sputum
- Ask your doctor about getting tested for chronic thromboembolic pulmonary hypertension (CTEPH) if you have unexplained shortness of breath. A rapid, non-invasive screening method to check for chronic thromboembolic pulmonary hypertension (CTEPH) is a ventilation-perfusion scan.
Diagnoses
Because the symptoms of pulmonary embolism (PE) resemble those of several other ailments and diseases, PE is sometimes challenging to diagnose.
Tests used to search for a PE may include the following in addition to a thorough medical history and physical examination:
- A chest X-ray: The heart and lungs are evaluated with this imaging procedure. Anatomical details about the heart, lungs, bronchi (big breathing tubes), aorta, pulmonary arteries, and mediastinum (a region in the middle of the chest separating the lungs) are shown by chest X-rays.
- V/Q scans are ventilation-perfusion scans: A little quantity of radioactive material is utilized to aid in the examination of the lungs during this nuclear radiology test. Ventilation, or the flow of air into and out of the bronchi and bronchioles, is assessed using a ventilation scan. A perfusion scan analyzes pulmonary blood flow.
- lung angiography: Blood artery stenosis, aneurysms, and blockages are just a few of the problems that may be assessed using this X-ray picture of the blood vessels. Through a tiny, flexible tube inserted into an artery, a dye (contrast) is injected. On an X-ray, this dye causes the blood vessels to be visible.
- CT (also known as a CAT scan) imaging. This imaging technique creates precise pictures of the body using X-rays and a computer. On a CT scan, the bones, muscles, fat, and organs are all clearly visible. The picture of the blood vessels in the lungs appears better on a CT scan with contrast. Contrast is a chemical similar to a dye that is injected into a vein to help the organ or tissue being studied appear more clearly on the scan.
- (MRI) Magnetic resonance imaging. This imaging test creates precise pictures of the body’s organs and structures using a magnetic field, radiofrequency technology, and a computer.
- Ultrasound (US) in duplex. This kind of vascular ultrasonography examines the anatomy and blood flow within the legs. (Blood clots from the legs frequently get loose and enter the lung.) The US employs a computer and high-frequency sound waves to generate pictures of the organs, tissues, and blood vessels.
- tests in the lab. Blood tests, such as the D-dimer level test, examine the blood’s clotting capacity. Testing for genetic abnormalities that may lead to irregular blood clotting may be done as part of further blood work. Arterial blood gases can be examined to determine the blood’s oxygen content.
- (EKG) Electrocardiogram. One of the easiest and quickest tests available to assess the heart is this one. On the arms, legs, and certain locations on the chest, electrodes (tiny, adhesive patches) are applied. Lead wires are used to connect the electrodes to the EKG device. It measures, analyzes, and prints out the heart’s electrical activity.
Treatment of Pulmonary Embolism (PE)
Medical Management
Once diagnosed, PE can be treated using a range of medical procedures.
PE is often treated in a hospital, where medical professionals can closely watch over your health.
Depending on how severe the clot is, the length of your pulmonary embolism therapy and hospital stay will change.
An anticoagulant (blood thinner) is the principal therapy for PE.
To increase blood flow in your pulmonary arteries, you may also undergo thrombolytic treatment, surgery, or interventional procedures, depending on the severity of the clot and its impact on your other organs, such as your heart.
- Anticoagulant medications
The most common kind of therapy is blood thinners known as anticoagulant drugs. Anticoagulants lessen the capacity of your blood to clot.
Understanding how and when to take your anticoagulant is crucial, as is according to your doctor’s instructions.
The kind of medication you’ll take, how long you’ll need to take it, and what kind of follow-up monitoring you’ll require will all depend on your diagnosis. Keep all planned follow-up visits with your doctor and the lab so they can keep track of how the drug is working for you.
Your follow-up will involve regular blood tests (prothrombin time test) while taking anticoagulants to monitor how quickly your blood clots. This enables your doctor to determine if you are receiving the proper dosage.
- Compression stockings
The most common kind of therapy is blood thinners, known as anticoagulant drugs. Anticoagulants lessen the capacity of your blood to clot. This helps to prevent new clots from forming.
Understanding how and when to take your anticoagulant is crucial, as is following your doctor’s instructions.
The kind of medication you’ll take, how long you’ll need to take it, and what kind of follow-up monitoring you’ll require will all depend on your diagnosis. Keep all planned follow-up visits with your doctor and the lab so they can keep track of how the drug is working for you.
Your follow-up will involve regular blood tests (prothrombin time tests) while taking anticoagulants to monitor how quickly your blood clots. This enables your doctor to determine if you are receiving the proper dosage.
Procedures
Your doctor may advise using surgery or a catheter to remove the blood clot from your pulmonary artery if the PE is life-threatening or if previous therapies are ineffective. Another choice is thrombolytic treatment (see the section below).
- Anticoagulant Therapy
One of the most popular therapies for PE is anticoagulation. Usually, fast-acting fibrinolytic medications such as pentasaccharide, fondaparinux, or heparin are used. The purpose of prescribing these drugs is to stop blood clot progression.
- Inferior Vena Cava Placement
Patients with recurrent PE, anticoagulation contraindications, or severe bleeding problems from anticoagulation may have an IVC filter implanted. IVC filters can successfully lower the risk of PE, but they also run the risk of raising the risk of DVT.
- Thrombolytic Therapy
The use of thrombolytic treatment may be necessary in the event of a large PE. When used with anticoagulants, thrombolytic medicines improve blood flow to tissues by dissolving obstructive thrombi. The agent that is utilized the most is t-PA. Urokinase and streptokinase are further alternatives.
- Embolectomy
Embolectomy is a surgical procedure used to remove emboli when anticoagulation and thrombolytic treatments have failed or are not appropriate.
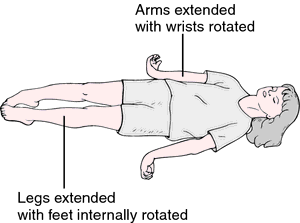
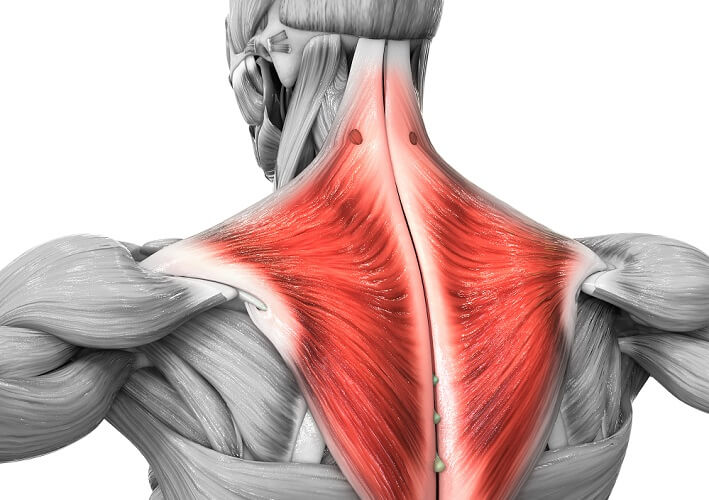
Physiotherapy Implications
After PE, mobility is essential for the patient’s recuperation. Bed rest is frequently advised after anticoagulation and thrombolytic treatments, then inpatient therapy. The main goals of physical therapy are to improve oxygen uptake and restore a clean lung field. This can be done by first engaging in chest physical therapy before progressing to endurance activities like walking or bicycle ergometry.
Pulmonary Rehabilitation
Following pulmonary embolism therapy, pulmonary rehabilitation aids patients in regaining strength and stamina. In addition to exercising under the direction of respiratory therapists, patients may learn about breathing exercises, drugs, oxygen treatment, and other topics during educational seminars.
lower your risk of pulmonary embolism
When a piece of the blood clot escapes from your leg and moves up to your lungs, where it causes a blockage, this condition is known as a pulmonary embolism.
You may take steps to reduce your chance of developing a pulmonary embolism.
Your medical staff should take precautions to avoid deep vein thrombosis if you are receiving care in a hospital for another ailment.
On trips lasting longer than six hours, a deep vein thrombosis can occasionally occur.
To lessen your chance of developing a deep vein thrombosis because of travel:
Do
- Wear loose-fitting clothing, sit comfortably on the seat, and try to lie back as much as you can.
- Make sure patients have enough legroom, drink enough water, and take frequent breaks from sitting. Also, when seated, flex and straighten the legs, feet, and toes every 30 minutes.
- Flight socks should be worn while periodically pressing the balls of the feet firmly on the ground.
Don’t
- avoid remaining still for extended periods of time: Get up and move around frequently instead of sitting down for longer than two hours at a time. Don’t cross your legs when you sit down if you have a deep vein thrombosis in one of your legs. Your circulation may be impacted by that posture. When you are on lengthy flights or long drives, keep this in mind.
- don’t consume alcohol
- Limit your intake of coffee and other beverages that contain caffeine.
- avoid using sleeping medications.
Home treatment of Pulmonary embolism?
For pulmonary embolism initial therapy, home remedies are not advised. However, it is crucial to do so in order to avoid more clots from forming and deep vein thrombosis, which can result in recurrent pulmonary embolism. The following actions lower the chance of getting a deep vein thrombosis:
- Follow the directions on your prescription anticoagulant medication.
- Exercise. Stretching the calves while relaxing the toes up toward the head can help keep the blood flowing through the legs. Repeat. When you spend a lot of time sitting down, such as during long car journeys or airplane flights, this exercise is extremely crucial.
- As soon as you can following surgery or sickness, get out of bed. It is crucial that everyone move as soon as they are able. Exercise your legs every hour if you are unable to get out of bed to maintain the blood flowing through your legs.
- Give up smoking.
- If you have a higher risk of developing deep vein thrombosis in your legs, you should use compression stockings to help avoid the disease.
Exercise following a pulmonary embolism: Things to keep in mind
Here are some crucial factors to take into account and tips to keep in mind if someone is healing from a pulmonary embolism and wondering whether they may start exercising:
- Obtain medical approval: It’s important to obtain approval from a healthcare provider before beginning an exercise program. When you push yourself too hard, your body needs time to repair, which might be hampered.
- Observe your body: Reduce the intensity if exercising is difficult for you. This will guarantee that you are working out at a tempo that you can endure safely.
- Start out slowly: Although it could be alluring to get right back into rigorous exercise, your body might require more time to heal before it can take prolonged periods of physical exertion.
- Every action counts: Don’t worry if you can just walk for a short while before getting tired. Your body will benefit from any movement, and they all add up.
- Be patient: the body has just experienced a severe and stressful event. To let it heal, use patience.
- Ingest your medication: It is crucial to take any medication that a medical practitioner recommends, such as a blood thinner. Deep vein thrombosis and pulmonary emboli are conditions for which exercise is not sufficient therapy.
- Putting on compression socks: The lower extremities’ blood flow is improved with compression stockings. Occasionally, a medical practitioner could advise putting on compression socks, whether you’re exercising or not.
Differential Diagnosis
PE can be mistaken for various illnesses that affect the cardiopulmonary system. These circumstances include:
- sudden cardiac failure
- Pneumonia
- Exacerbation of chronic obstructive pulmonary disease
- Heart fibrillation
- Myocardial infarction acute
Complications
A pulmonary embolism may endanger life. A pulmonary embolism that is undetected and untreated results in around one-third of patients dying. But when the problem is identified and treated right away, that number drastically decreases.
Additionally, pulmonary embolisms can cause pulmonary hypertension, a disease in which the right side of the heart and the blood pressure in the lungs are both excessively high. When the arteries in your lungs are blocked, it takes more effort from your heart to pump blood through them. This raises blood pressure and weakens your heart over time.
Rarely, tiny clots called emboli stay in the lungs, and over time, scarring in the pulmonary arteries occurs. As a result, blood flow is constrained, leading to persistent pulmonary hypertension.
A pulmonary embolism may endanger life. Pneumonia emboli are fatal in around one-third of undiagnosed and untreated patients. On the other hand, that number drastically decreases when the illness is identified and treated quickly. A condition known as pulmonary hypertension, which is marked by elevated blood pressure in the lungs and on the right side of the heart, is another consequence of pulmonary embolisms. When the arteries in the lungs are blocked, the heart has to work harder to force blood through the obstructions. This increases blood pressure and weakens the heart over time. Rarely, tiny clots called emboli stay in the lungs, and over time, scarring in the pulmonary arteries occurs. Due to these restrictions on blood flow, persistent pulmonary hypertension develops.
Lung tissue damage from a pulmonary embolism (PE) might result from a lack of blood supply. Low blood oxygen levels can result, which can harm not just the heart but also other bodily organs. Large or many pulmonary emboli, in particular, can quickly result in major life-threatening issues and even death. Blood thinners or anticoagulants are routinely used to treat pulmonary embolism. If these medications thin the blood too much, it might put patients at risk for severe bleeding. When bleeding continues after 10 minutes of pressure application, it is considered excessive bleeding. The indicators of bleeding in the digestive tract include another bleeding symptom to look out for:
- Vomit that is bright crimson or resembles coffee grounds
- Blood in the stool that is bright crimson or viscous, dark stools
- Continent pain
- signs of cerebral hemorrhage include:
- terrible headache
- sudden alterations in eyesight
- sudden loss of sensation or mobility in the arms or legs
- lack of memory or confusion
- If you experience any of these, you must seek medical attention immediately.
How to Prevent Pulmonary Embolism (PE)?
Among the ways to avoid a pulmonary embolism are:
- Regularly moving about. Move your arms, legs, and feet for a few minutes every hour if you are unable to walk. Wear compression stockings if you anticipate needing to sit or stand for extended periods of time to promote blood flow.
- Water is important, but alcohol and caffeine should be kept to a minimum.
- Avoid using any tobacco products.
- Do not cross your legs.
- Avoid wearing clothes that are too tight.
- If you are overweight, lose weight.
- Elevate the feet twice daily for 30 minutes.
- If you or a member of your family has ever experienced a blood clot, bring it up with your doctor so they can discuss ways to lower your risk factors. Pulmonary embolisms are mostly caused by deep vein thrombosis. Therefore, the primary method of pulmonary embolism prevention is the prevention of deep vein thrombosis. The doctor could advise the following if you are at risk for either condition:
- When you are sleeping, lift the bottom of the bed and elevate the legs as often as you can.
- Maintain a healthy weight.
- Walking is a great way to begin moving and exercising right after surgery.
- Give up smoking.
- For problems from surgery, a heart attack, a stroke, or cancer, take the anticoagulant.
- Use pneumatic compression when you need to be immobile for a while.
- Put on some compression socks.
Drinking lots of water, using support stockings, taking regular pauses to stand or walk, and performing calf and ankle exercises in the seat can all be helpful for extended sitting or travel. The physicians may also advise taking aspirin before flying if you are more likely to develop deep vein thrombosis, such as after orthopedic surgery. The doctor could also suggest an interventional treatment in which a filter is inserted into the biggest vein in the body. Before they reach the lungs, clots are stopped by a vena cava filter. Pulmonary embolisms can be avoided by preventing blood clots in deep leg veins. Due to this, the majority of hospitals are vigorous in their efforts to prevent blood clots.
- Blood thinners: People who are at risk of blood clots frequently get these medications both before and after surgery. Additionally, they are frequently administered to patients who are hospitalized to the hospital due to specific medical disorders, such as heart attack, stroke, or cancer-related difficulties.
- Compression stockings: Legs are steadily compressed by compression stockings, which helps veins and leg muscles flow blood more effectively. They provide a straightforward, low-cost method for preventing blood from accumulating in the legs before and after surgery.
- Leg elevation: When feasible especially at night, elevating the legs can be quite beneficial. Blocks or books can be used to extend the base of a bed by 4 to 6 inches (10 to 15 cm).
- Physical activity: After surgery, getting up and moving about can help prevent pulmonary embolism and speed up healing in general. This is one of the major reasons the nurse might encourage you to stand up and move even on the day of surgery in spite of the discomfort at the site of the incision.
- Pneumatic compression: In this type of therapy, thigh-high or calf-high cuffs are worn; they automatically inflate and deflate every few minutes. This increases blood flow by massaging and constricting the veins in the legs.
stretching when traveling
- If you can, get up and move about every few hours if you’re on a lengthy flight. Flex your ankles by drawing your toes closer to you if you are unable to stand up.
- Here are some other stretches that folks may attempt while seated:
- With one hand, raise the leg toward the chest.
- With the other hand, hold the bottom of that leg.
- After holding this position for 15 seconds, try the opposite leg.
- Up to 10 times every hour, perform this.
- If you’re traveling a long distance, stop every hour to walk about.
- Additionally, remember to increase your fluid intake to help you keep hydrated.
- alterations in way of life
You can also keep your weight in a healthy range.
Consult your doctor about the possibility of blood clots if you want to use hormones, such as those used in birth control or replacement treatment.
Take your medications, keep an eye on your diet, and discuss any changes with your doctor if you have any other health problems, such as diabetes or heart trouble.
Consult your physician if you have a history of renal illness, certain autoimmune disorders, or blood clots in your family.
Quit smoking if you do.
The doctor may choose to provide thrombolytic medications to you in life-threatening pulmonary embolism instances in order to dissolve the blood clot. Surgery may even be required to complete it or separate it, though this is uncommon.
- Drink a lot of water: Dehydration can lead to the formation of blood clots, hence water is the best beverage to avoid it. Avoid alcohol since it might cause fluid loss.
- Take a seat for a while: Once per hour or so, go around the cabin of the flight. When you’re driving, pull over sometimes and do a few laps around the vehicle. Make a couple of extended knee bends.
- Get up from your seat: Every 15 to 30 minutes, bend over, rotate your ankles in circles, and lift your toes. Put on support socks. To aid in promoting circulation and fluid mobility in your legs, your doctor may advise using these. A variety of fashionable colors and textures are offered in compression stockings: To assist you in putting on the stockings, there are even gadgets called stocking butlers.
While still minimal, the danger of blood clots growing while flying increases with the amount of long-haul travel.
Can pulmonary embolism result in fatalities? rate of survival
The likelihood of a patient surviving a pulmonary embolism depends on a number of factors, including the patient’s overall health, the burden of blood clots caused by the embolism, the impact it has on the heart’s ability to pump blood to the body’s organs, the stability of vital signs, the cause of the embolism, and the ability to diagnose the condition quickly and begin treatment.
A pulmonary embolism is a highly severe ailment that, if left untreated, might result in permanent sickness or even death. The prognosis after therapy relies on the size of the blood clot and any obstructions, as well as the patient’s general health and the heart’s ability to pump blood.
Depending on the individual, recovery from a pulmonary embolism might take a certain period of time. After several weeks or months, many people can fully recover and resume their usual level of activity. As patients receive therapy and their bodies heal, some of the symptoms could become better.
FAQs
breathlessness that emerges out of nowhere.
You may believe you are experiencing a heart attack if you have severe chest discomfort that becomes worse as you breathe in.
Due to a quick drop in blood pressure, one may experience lightheadedness, dizziness, or fainting.
Cough, which might be bloody.
Deep vein thrombosis (DVT), which is the most typical cause of a pulmonary embolism, is the breaking off of a blood clot in your leg’s deep veins. Air bubbles are an additional, less common cause of a pulmonary embolism. An upper body DVT.
Even though an ECG cannot be used to diagnose a PE, it might indicate cardiac conditions that might be a sign of a PE, especially if the patient also exhibits other symptoms. It could specifically indicate issues with the right ventricle of the heart.
Treating shock and administering oxygen therapy are the primary steps in treating the majority of embolisms. Heparin, enoxaparin, or warfarin are common anticoagulant drugs used to thin the blood and prevent additional clotting from occurring.
A pulmonary embolism may endanger life. A pulmonary embolism that is undetected and untreated results in around one-third of patients dying. But when the problem is identified and treated right away, that number drastically decreases.
The underlying reason will determine how long the therapy will last. After a PE, the majority of patients fully recover, but others may endure persistent symptoms, including breathing difficulties. Depending on the PE’s severity and the patient’s general condition, the healing time may vary.
The duration of the therapy will depend on the underlying cause. The majority of PE patients fully recover, although some may experience lingering symptoms, including breathing problems. The recovery period may differ based on the severity of the PE and the patient’s overall health.
clotting agents.
While your body attempts to dissolve the clots, these blood-thinning medications called anticoagulants stop existing clots from growing larger and prevent new clots from developing. Anticoagulant heparin is widely prescribed and can be administered intravenously or topically.
A pulmonary embolism (PE) occurs when a lung artery abruptly gets clogged. It frequently happens when a blood clot breaks loose and moves through the bloodstream to the lungs. Lung damage from the risky illness known as PE may not be able to be healed.
Other therapies may be required in more severe pulmonary embolism situations in order to dissolve or remove a clot. This may be accomplished with thrombolytic medications, which aid in dissolving the blood clot, or, less frequently, by removing the clot surgically.
In the deep veins of the lower extremities, thrombi are where the majority of PEs start. The iliac veins experience thrombosis less commonly than the femoropopliteal veins or the calf veins.




3 Comments