Pudendal Nerve
Table of Contents
Introduction
The Pudendal Nerve is a major nerve responsible for controlling and innervating the genital and anal regions. It originates from the sacral plexus and travels through the pelvis, supplying various muscles and sensory regions in the perineal area.
The word “Pudendal” is derived from the Latin word pudenda, which means “external genitals” and is a diminutive of pudendum, which means “parts to be ashamed of.”
The primary nerve of the perineum, pelvic floor muscles, and external genitalia is known as the pudendal nerve. In 1836, Benjamin Alcock originally defined it while studying the external genitalia and the route of the internal pudendal artery.
The word “pudendal” is derived from the Latin “pudenda,” which means “external genitalia,” and “pudendum,” which means “parts to be ashamed of.” In a section on iliac arteries in Robert Bentley Todd’s “The Cyclopaedia of Anatomy and Physiology,” Alcock described the canal and pudendal nerve.
The pudendal nerve performs sensory, motor, and autonomic activities. One of the main sacral plexus nerves arises after the sciatic nerve. The nerve is bilaterally paired, which means that it may be found on both the left and right sides of the body.
What is the Pudendal Nerve?
A significant somatic nerve of the sacral plexus is the pudendal nerve.
The pudendal nerve is an important nerve in your pelvic area. This nerve transmits information about movement (motor) and feeling from your vaginal region. The pudendal nerve connects your pelvic floor muscles, which support your organs, to your external genitalia.
The majority of movement and feeling in your pelvic area, including your anus and external genitalia, come from the pudendal nerve. It is essential to your capacity to control when you urinate and excrete. This nerve injury can cause pain and interfere with your ability to engage in or enjoy sex. Pudendal nerve entrapment syndrome results from pressure on the nerve. Pudendal neuralgia, a severe, persistent pain symptom of this illness, can be incapacitating.
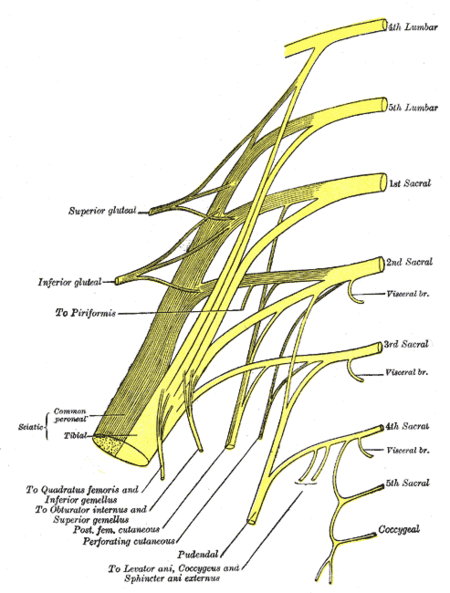
Course of Pudendal Nerve
A course of the pudendal nerve typically refers to the path it takes as it travels through the body.
- The pudendal nerve takes input from the sacral plexus’s major ventral roots of S2-S4, which merge to create the nerve next to the lateral wall of the pelvic cavity. It then divides into one, two, or three trunks before branching out; varying contributions from S1 and/or S5.
- The nerve is tightly connected with the branches of the internal pudendal artery and vein during the majority of its course.
- It subsequently exits the pelvis through the larger sciatic foramen, which is located beneath the piriformis muscle and bends around the posterior portion of the sacrospinous ligament.
- It travels through the gluteal area for a very short distance before bending around the sacrospinous ligament and entering the perineum through the minor sciatic foramen.
- The pudendal nerve is located in the gluteal area, close to the ischial spine, and is the target of a pudendal nerve block.
- Compressive nerve illnesses are often detected during the inter ligamentous phase of the nerve’s trip, which is dorsal to the sacrospinous ligament and ventral to the sacrotuberous ligament.
- The nerve exits the smaller sciatic foramen and enters the perineum via the pudendal (Alcock’s) canal, a sheath of connective tissue on the medial wall of the obturator internus muscle.
- It continues via the pudendal canal, dividing into three branches on its way to the pubic symphysis.
- As soon as the pudendal nerve reaches the canal (also known as the inferior rectal nerve), it gives rise to the inferior anal nerve.
- When the nerve reaches the canal’s distal end, it divides into two branches: the perineal nerve and the dorsal nerve of the penis/clitoris.
- Origin: The pudendal nerve originates from the sacral plexus, which is a complex network of nerves formed by the anterior rami (branches) of the sacral spinal nerves. Specifically, the pudendal nerve receives contributions from the sacral spinal cord segments S2, S3, and S4. These nerve roots combine to form the pudendal nerve, which then follows a course through the pelvis to innervate the muscles and provide sensory functions in the perineal region, including the genital and anal areas.
- Pelvic Region: After exiting the sacral plexus, the pudendal nerve travels through the greater sciatic foramen, which is an opening in the pelvis.
- Re-entry into the Pelvis: The nerve then re-enters the pelvis through the lesser sciatic foramen, which is another anatomical structure in the pelvis.
- Perineum: Once inside the pelvis again, the pudendal nerve reaches and innervates the perineum. The area located between the anus and the genitals is identified as the perineum.
- Branching: Within the perineum, the pudendal nerve branches out to supply various muscles and sensory regions. It provides motor innervation to muscles like the external anal sphincter and the perineal muscles. It also supplies sensory innervation to the external genitalia, the anal region, and the perineum.
This course allows the pudendal nerve to fulfil its crucial functions in controlling the muscles and providing sensory feedback to the perineal region. Dysfunction or injury along this course can lead to various medical issues.
Nucleus:
The nerve, a significant branch of the sacral plexus, has fibers that originate in the sacral area of the spinal cord’s Onuf’s nucleus.
Variation:
The origins of the pudendal nerve can differ. For instance, the sciatic nerve may really be the place where the pudendal nerve begins. As a result, the pudendal nerve may also be impacted by sciatic nerve injury. Pudendal nerve fibers can occasionally come from S5 and the dorsal rami of the first sacral nerve.
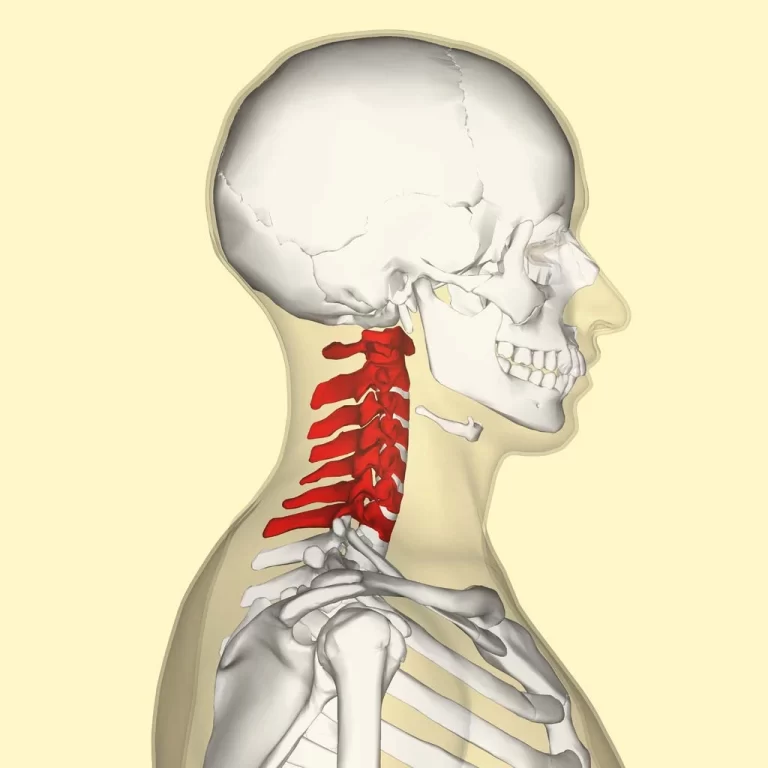
Root
- Nerve roots- S2,S3,S4
The pudendal nerve is derived from the nerve roots of the sacral plexus, specifically from the sacral spinal cord segments S2, S3, and S4. These spinal cord segments are part of the sacral region of the vertebral column and are responsible for providing the motor and sensory innervation for the structures in the perineal region, which includes the genital and anal areas.
To clarify:
- S2, S3, and S4 are the specific spinal cord segments that contribute fibers to form the pudendal nerve.
Branches of Pudendal Nerve
The pudendal nerve has three primary branches. As follows:
- Inferior branch of the rectus
- Perineal branch: which is separated into superficial (cutaneous) and deep (muscular) perineal nerve, which further divides into medial and posterolateral scrotal/labial nerve.
- Dorsal branch of penis/clitoris
The pudendal nerve gives rise to several branches as it courses through the pelvic region. These branches serve various muscles and sensory regions in the perineal area, including the genital and anal regions. The major branches of the pudendal nerve include:
- Inferior Rectal Nerve: This branch innervates the external anal sphincter muscles, contributing to their motor function and providing sensory innervation to the anal region.
- Perineal Nerve: The perineal nerve supplies sensory innervation to the perineal region, which is the area between the anus and genitals. It also innervates the perineal muscles, contributing to their motor function.
- Dorsal Nerve of the Penis (in males) or Dorsal Nerve of the Clitoris (in females): This branch provides sensory innervation to the penis or clitoris, respectively, and plays a role in sexual arousal and pleasure.
- Posterior Scrotal Nerves (in males) or Labial Nerves (in females): These branches provide sensory innervation to the posterior scrotum in males or the labia majora in females.
These branches play essential roles in controlling and coordinating various functions related to urination, defecation, and sexual response, as well as providing sensory feedback from the perineal area. Dysfunction or injury to these branches can lead to various medical issues, including sexual dysfunction, urinary and fecal incontinence, and chronic pelvic pain.
Function of Pudendal Nerve
What is the pudendal nerve’s function?
The pudendal nerve is essential for pelvic sensation and function, including the genitals and anus. This nerve is part of your nervous system’s peripheral nervous system. Peripheral nerves carry messages from your central nervous system (brain and spine) to your limbs and organs.
Your movement is controlled by the pudendal nerve’s motor function because:
Anal sphincter muscles aid in the retention or release of feces (poop).
Urethral sphincter muscles aid in the retention or discharge of urine (pee).
The nerve also sends sensory information to your brain regarding touch, pleasure, pain, and temperature to your:
The penis (a component of the male reproductive system).
Vagina (a component of the female reproductive system).
The skin between your anus and your vagina or penis is known as the perineum.
Anal canal and anus (a digestive system component).
70% somatic fibre (including 50% sensory and 20% motor fibres) and 30% autonomic fibres compose the pudendal nerve.
- The inferior rectal nerve, which is located below the pectinate line, sends somatic motor fibres to the external anal sphincter and returns sensations from the anal canal.
- In the urogenital triangle, the perineal nerve supplies motor and sensory fibres to the labia minora, vaginal vestibule, lower one-fifth of the vaginal canal, and posterior aspect of the labia majora in women and the external urethral sphincter and posterior scrotum in males.
- Deep (muscular) branch:
- The ischiocavernosus, superficial transverse perineal, and bulbospongiosus muscles, which are located in the superficial perineal space (pouch), are innervated by the deep (muscular) branch in both sexes. As a result, it assists with ejaculation, maximum erectile stiffness, and synchronised contractions of the pelvic diaphragm and all perineal muscles.
- The deep perineal nerve, which is present in both sexes, innervates the external urethral sphincter, which allows for the voluntary control of micturition, as well as the two deep transverse perineal muscles.
- The compressor urethrae and the sphincter urethrovaginalis are two additional skeletal muscles in the deep perineal area that are innervated by the deep perineal nerve in females.
- Deep (muscular) branch:
- The majority of the skin covering the urogenital triangle is supplied with somatic sensation by the superficial branch of the perineal nerve, which is known as the posterior scrotal or labial nerves.
- Men’s dorsal nerve of the penis, while women’s dorsal nerve of the clitoris:
- Bringing back somatic feelings from the shaft (body) and glans of the penis or clitoris, this exclusively cutaneous branch of the pudendal nerve is essential to sexual activity.
- This branch is a crucial component of the neuropathway that leads to erections. The dorsal nerve afferent fibers inside the lumbosacral spinal cord interact with the cavernous nerves (containing parasympathetic axons) that penetrate the perineal membrane to innervate and support the vasodilation of erectile tissue when triggered.
This nerve serves several important functions in the human body, primarily related to the innervation of the perineal region, which is the area between the anus and the genitals. There are the key functions of the pudendal nerve:
- Motor Function: This nerve controls and innervates the muscles of the perineum, including the external anal sphincter, the perineal muscles, and the muscles responsible for erection and ejaculation in males. These motor functions are essential for maintaining continence, controlling genital function, and facilitating sexual activity.
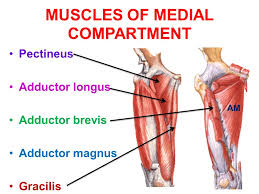
- The motor function of the pudendal nerve primarily involves controlling and innervating the muscles of the perineum, which is the region between the anus and the genitals. Specifically, the pudendal nerve plays a key role in the motor control of the following muscles:
- Muscles of the perineum and pelvic floor are innervated by the perineal nerve:
- Bulbospongiosus
- Ischiocavernosus
- muscles of the levator ani (including the puborectalis, iliococcygeus, and pubococcygeus).
- Another source of direct innervation for the levator ani muscles is the anterior ramus of the S4 nerve root.
- External Anal Sphincter: This nerve provides motor innervation to the external anal sphincter. This muscle surrounds the anus and is responsible for voluntary control over bowel movements. When the external anal sphincter contracts, it closes the anus, preventing the passage of feces or gas. Defecation is made possible by this muscle relaxation.
- Perineal Muscles: The pudendal nerve innervates various perineal muscles, including the bulbospongiosus and ischiocavernosus muscles in both males and females. In males, it also innervates the superficial and deep transverse perineal muscles. These muscles play a role in sexual function and urinary control.
- Muscles for Sexual Function (in males): In males, the pudendal nerve controls the muscles responsible for erection (ischiocavernosus and bulbospongiosus) and ejaculation (bulbospongiosus). These muscles are vital for sexual arousal and reproductive function.
- Sensory Function: The nerve provides sensory innervation to various regions, including the external genitalia (clitoris and penis), the anal region, and the perineum. This sensory input is crucial for sexual arousal and pleasure, as well as for detecting sensations related to pain, pressure, and temperature in these areas.
- The sensory function of the pudendal nerve involves transmitting sensory information from various regions of the perineum, which is the area between the anus and the genitals, as well as the genital and anal regions. Here are the key sensory functions of the pudendal nerve:
- Genital Sensation (Clitoris and Penis): The pudendal nerve provides sensory innervation to the external genitalia. In females, it supplies sensory information from the clitoris, while in males, it innervates the penis. This sensory input is crucial for sexual arousal and pleasure.
- Anal Sensation: The pudendal nerve also carries sensory signals from the anal region, providing feedback related to sensations like pain, pressure, and temperature. This sensory input aids in controlling bowel movements and detecting sensations related to defecation.
- Perineal Sensation: The nerve supplies sensory innervation to the perineal region, which includes the area between the anus and genitals. This sensory feedback is essential for various functions, including sexual response and pain perception in the perineal area.
- Urinary Sensation: While the primary role of the pudendal nerve is not urinary sensation, it can indirectly influence urinary control by providing feedback from the perineal region. Changes in perineal sensation can sometimes affect the awareness of bladder fullness and the timing of urination.
- Urinary Control: The pudendal nerve plays a role in controlling the urinary sphincters, including the external urethral sphincter. It contributes to maintaining urinary continence and the ability to voluntarily control the release of urine.
- Defecation Control: The external anal sphincter, which is innervated by the pudendal nerve, allows for voluntary control over bowel movements. This control is vital for maintaining fecal continence and preventing incontinence.
- Sexual Function: The pudendal nerve’s role in controlling the muscles of the perineum is essential for sexual function, particularly in males. It contributes to achieving and maintaining an erection, controlling ejaculation, and facilitating sexual pleasure.
- Pain Perception: While it is primarily involved in transmitting sensory information related to pleasure and function, the pudendal nerve can also transmit pain signals. Dysfunction or irritation of the pudendal nerve can lead to conditions like pudendal neuralgia, characterized by chronic pelvic pain.
What causes Pudendal Nerve dysfunction?
Pudendal nerve injury can be caused by a variety of factors, including:
Accidents and traumatic events.
Pelvic surgical complications, such as a prostatectomy or surgery to repair pelvic organ prolapse.
Diabetes and diabetic neuropathy.
Labour and delivery were difficult.
Prolonged nerve pressure caused by activities such as cycling.
Radiation treatment.
Tumours and cysts.
Pudendal nerve problems can be caused by various factors, and they typically result from damage or compression of the pudendal nerve. The pudendal nerve is responsible for providing sensation to the genital and perineal areas, as well as controlling certain pelvic muscles. When the pudendal nerve is compromised, it can lead to a range of symptoms and conditions. Some common causes of pudendal nerve problems:
- Prolonged or repetitive pressure: Sitting for long periods on hard or narrow surfaces, such as bicycle seats, can put pressure on the pudendal nerve and lead to nerve compression or irritation. This is a common cause of pudendal neuralgia.
- Trauma or injury: Direct trauma to the pelvis or perineum, such as a fall or childbirth, can damage the pudendal nerve.
- Infections and inflammation: Infections, such as herpes or pelvic inflammatory disease, and inflammatory conditions can cause irritation and damage to the pudendal nerve.
- Pelvic surgery: Certain surgical procedures in the pelvic area, including surgery for prostate, rectal, or gynecological conditions, can inadvertently injure the pudendal nerve.
- Tumors or masses: Growths or tumors in the pelvic region can compress or damage the pudendal nerve.
- Pregnancy and childbirth: The pressure and stretching that occur during pregnancy and childbirth can sometimes lead to pudendal nerve injury.
- Nerve entrapment: In some cases, the pudendal nerve can become entrapped or compressed as it passes through tight or constricted areas of the pelvis.
- Idiopathic causes: In some cases, the exact cause of pudendal nerve problems may not be clear, and the condition is termed idiopathic pudendal neuralgia.
The symptoms of pudendal nerve problems can vary but often include pain, numbness, tingling, and discomfort in the genital, anal, or perineal areas. These symptoms can be disruptive to a person’s daily life and may require medical evaluation and treatment.
Clinical relevance
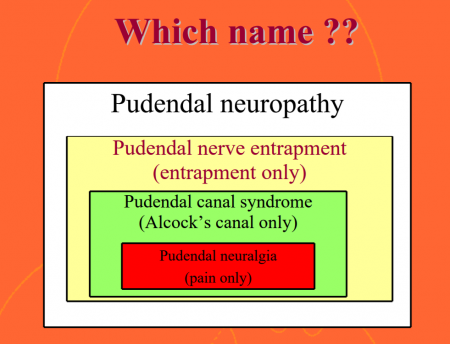
- Pudendal neuralgia:
- It is a chronic pain disorder characterized by persistent and often severe pain in the genital, anal, and perineal regions. It is typically caused by compression or irritation of the pudendal nerve. Symptoms may include burning, shooting, or stabbing pain, as well as numbness or tingling. Pudendal neuralgia can significantly impact a person’s quality of life and sexual function.
- Pudendal nerve block
- A local anesthetic is injected during this surgery close to the pudendal nerve. This method can be used to relieve discomfort during obstetric operations, particularly during childbirth in women who are unable to receive spinal anesthesia, as well as to aid in the diagnosis of pudendal nerve entrapment.
- To temporarily stop nerve transmission, the block is achieved by giving a single injection close to the pudendal nerve. In these treatments, the ischial spine serves as a marker to help determine where to deliver the anesthetic.
- It is also beneficial in the treatment of interstitial cystitis, haemorrhoids, anorectal, vaginal, and perineal surgery, labour, episiotomies, prostate biopsy, and prostate brachytherapy.
- Pudendal nerve iatrogenic injury
- Pudendal nerve damage is especially dangerous during obstetrical, perineal, and proctological operations.
- Pudendal Nerve Entrapment:
- This condition occurs when the pudendal nerve becomes trapped or compressed, often within the Alcock’s canal or along its course. Entrapment can lead to pudendal neuralgia and associated symptoms.
- Pelvic Floor Dysfunction:
- Dysfunction of the pelvic floor muscles, which are innervated by the pudendal nerve, can lead to conditions such as pelvic floor muscle spasm or hypertonicity. These conditions may result in chronic pelvic pain, urinary and fecal incontinence, and pain during sexual intercourse.
- Urinary Incontinence:
- Damage or dysfunction of the pudendal nerve can lead to urinary incontinence, which is the involuntary leakage of urine. This can occur due to weakened pelvic floor muscles, impaired control of the external urethral sphincter, or altered sensory feedback from the bladder.
- Fecal Incontinence:
- Similar to urinary incontinence, damage to the pudendal nerve can result in fecal incontinence, where individuals have difficulty controlling bowel movements. This can lead to the involuntary passage of stool.
- Perineal Trauma:
- Injury or trauma to the perineal area, such as during childbirth or pelvic surgery, can sometimes affect the pudendal nerve. This can lead to pain, numbness, or other sensory and motor issues in the perineal region.
What function do pudendal nerve blocks play during childbirth?
- Pudendal nerve blocks are occasionally used to relieve discomfort during delivery. If you are unable or unable to receive an epidural (spinal anesthesia) or require additional pain management during your repair, your specialist may recommend a nerve block.
- A pudendal nerve block has a rapid onset of action. It alleviates discomfort during the second (pushing) stage of labor or before an episiotomy. However, it does not alleviate the pain and discomfort of contractions.
Assessment
History:
The following are some of the most common causes of pudendal nerve injury:
Long periods of sitting (for example, seamstresses, computer operators, judges, concert pianists, locomotive engineers)
Repetitive hip flexion (sports, exercise, running, and cycling)
Direct trauma includes falls, car accidents, vaginal deliveries, and pelvic procedures, particularly when mesh is used (e.g., surgery for urine incontinence, complete abdominal hysterectomy).
Radiation therapy, particularly in men with prostate cancer and women with rectal and gynecological malignancies.
Pain Assessment:
The patient suffering from pelvic discomfort (particularly perineal and genital) with or without accompanying sexual, bladder, or bowel complaints
Except for acute injuries, pain develops gradually.
Pain is less severe in the morning and grows during the day. The most common type of pain is burning, but you may also feel tingling, aching stabbing, and shock-like pain.
Pain increases by sitting and is reduced by standing, lying down, or sitting on the toilet.
Pain can be distributed in a variety of ways, including the vulva, vagina, clitoris, perineum, and rectum in females, and the glans penis, scrotum, perineum, and rectum in men.
Urinary frequency, urgency, symptoms resembling interstitial cystitis, painful ejaculation, dyspareunia, painful nocturnal orgasms, and prolonged sexual desire are all indications of PN
Sensation of a foreign body
How to diagnose pudendal nerve problems?
Diagnosing pudendal nerve problems can be complex and may involve a combination of medical history, physical examination, and diagnostic tests. If you suspect you have pudendal nerve problems or are experiencing symptoms such as chronic pelvic pain, genital discomfort, or perineal pain, it’s crucial to seek evaluation and diagnosis from a healthcare provider, preferably one with expertise in pelvic pain and nerve disorders. Here’s an overview of the diagnostic process for pudendal nerve problems:
- Medical History and Symptoms Assessment:
- Your healthcare provider will begin by taking a detailed medical history, including information about your symptoms, their duration, and any relevant medical conditions or injuries.
- Be prepared to provide information about the location, nature, and intensity of your pain or discomfort. Describe any activities or situations that worsen or alleviate your symptoms.
- Physical Examination:
- A thorough physical examination of the pelvic area and perineum will be conducted. Your healthcare provider will assess for tenderness, muscle strength, and any signs of nerve compression or irritation.
- It may be necessary for your provider to perform a digital rectal examination to assess the condition of the pudendal nerve and surrounding structures.
- Diagnostic Tests:
- Electromyography (EMG): EMG tests can measure the electrical activity in muscles controlled by the pudendal nerve. This test can help identify nerve dysfunction or injury.
- Nerve Conduction Studies: These tests evaluate the speed and strength of electrical signals traveling along the pudendal nerve. Abnormal results may suggest nerve damage.
- Imaging Studies: Imaging techniques like MRI (Magnetic Resonance Imaging) or ultrasound may used to visualize the pelvis and assess the anatomy of the pudendal nerve and surrounding structures. These tests can help identify potential causes of nerve compression.
- Pudendal Nerve Block:
- A pudendal nerve block is a diagnostic procedure where a local anesthetic is injected near the pudendal nerve. If the pain is significantly relieved following the injection, it can confirm that the pudendal nerve is involved in your symptoms, helping to confirm the diagnosis.
- Other Tests:
- In some cases, your healthcare provider may order additional tests or consultations to rule out other potential causes of pelvic pain or discomfort.
- Specialized Evaluation:
- It’s important to consult with healthcare providers who specialize in pelvic pain, pelvic floor disorders, or pudendal nerve conditions, as they have the expertise to accurately diagnose and manage these complex issues.
Management of pudendal nerve problems may include physical therapy, medications for pain management, nerve blocks, and, in some cases, surgical interventions to address nerve compression or entrapment. The particular strategy of treatment will depend on the underlying cause and severity of your ailment.
How can I protect my pudendal nerves?
These actions can help keep your nervous system in good form:
- Don’t sit for lengthy periods of time.
- When riding, take frequent rests.
- Stress can manage with meditation, walking, or other healthy activities.
- Eat a balanced diet to keep your weight at a healthy level.
- Manage nerve-damaging illnesses such as diabetes and high blood pressure.
- Seek assistance in quitting smoking. Tobacco consumption reduces blood flow to the nerves.
When should I consult a physician?
If any of the following occur, contact a doctor right away:
- You have persistent pelvic discomfort.
- sitting down makes the pain worse.
- malfunction in sexual behavior.
- Incontinence of the urine or feces.
Treatment for pudendal nerve problem:
The treatment for pudendal nerve problems depends on the underlying cause and the severity of your condition. Pudendal nerve problems can manifest as pudendal neuralgia, nerve entrapment, or other related issues. Here are some common treatment approaches for pudendal nerve problems:
- Conservative Management:
a. Physical Therapy: Pelvic floor physical therapy can be highly effective in managing pudendal nerve problems. A trained physical therapist can help you perform exercises to relax and strengthen pelvic floor muscles, release muscle tension, and improve posture and alignment.
b. Lifestyle Modifications: Avoiding activities that exacerbate symptoms, such as prolonged sitting or cycling, can be helpful. Lifestyle changes, including dietary modifications and stress reduction techniques, may also be recommended.
c. Oral Medications: Your healthcare provider may prescribe medications to manage pain and inflammation, such as non-steroidal anti-inflammatory drugs (NSAIDs), neuropathic pain medications (e.g., gabapentin or pregabalin), or muscle relaxants.
- Nerve Blocks:
a. Pudendal Nerve Block: A pudendal nerve block involves injecting a local anesthetic and/or a corticosteroid near the pudendal nerve. This provides temporary relief from pain and also used for diagnostic and therapeutic purposes.
- Neuromodulation:
a. Peripheral Nerve Stimulation: In some cases, peripheral nerve stimulation can consider. This involves the implantation of a device that delivers electrical impulses to the pudendal nerve to help alleviate pain.
- Surgery:
a. Pudendal Nerve Decompression: Surgical decompression of the pudendal nerve may be necessary if there is evidence of nerve entrapment or compression. During this procedure, the surgeon releases any structures or tissues that are compressing the nerve.
b. Neurosurgery: In severe cases or when other treatments fail, neurosurgery may be considering. This may involve more extensive procedures to address nerve compression or damage.
- Alternative Therapies:
a. Acupuncture: Some people find relief from pudendal nerve-related symptoms through acupuncture, which may help with pain management and relaxation.
b. Biofeedback: Biofeedback training can teach you how to control and relax pelvic floor muscles, which can be beneficial for managing pudendal nerve problems.
- Psychological Support:
a. Counseling or Therapy: Chronic pain conditions like pudendal neuralgia can be emotionally challenging. Psychological counseling or therapy can help individuals cope with the emotional aspects of their condition and develop strategies for managing pain.
- Dietary Modifications:
a. Some individuals find relief from pudendal nerve-related symptoms by making dietary changes, such as reducing foods that can irritate the pelvic region, like caffeine or spicy foods.
Pudendal nerve problems can be complex and may require a multidisciplinary approach, involving specialists such as urologists, gynecologists, pain management specialists, and physical therapists, among others.
FAQs
The pudendal nerve is a major nerve responsible for controlling and innervating the genital and anal regions. It originates from the sacral plexus and travels through the pelvis, supplying various muscles and sensory regions in the perineal area.
Pudendal nerve functions include both motor and sensory functions. It controls the muscles of the perineum, including the external anal sphincter, and provides sensory innervation to the external genitalia, anal region, and perineum. It plays a crucial role in sexual function, urinary and fecal continence, and pain perception.
Symptoms may include chronic pelvic pain, sexual dysfunction, urinary and fecal incontinence, pain during bowel movements, and sensory disturbances in the genital and perineal areas.
Pudendal neuralgia is a condition characterize by chronic perineal pain due to pudendal nerve irritation or compression. Diagnosis often involves a thorough medical history, physical examination, and diagnostic procedures like pudendal nerve blocks or electromyography (EMG).
Treatment may include physical therapy, medications (such as pain relievers or nerve modulators), nerve blocks, lifestyle modifications, and in some cases, surgical interventions to address nerve compression or entrapment.
Pudendal nerve dysfunction can result from various factors, including trauma (e.g., childbirth or pelvic surgery), repetitive pressure (as in cycling-related issues), infections, inflammation, or anatomical abnormalities.
Preventive measures may include maintaining good pelvic health, avoiding prolonged pressure on the perineal area, practicing safe sex to prevent infections, and seeking prompt medical attention for pelvic trauma or pain.
The outcome of treatment for pudendal nerve-related conditions depends on the underlying cause and the individual’s response to therapy. Some people experience significant improvement or resolution of symptoms with appropriate treatment, while others may have ongoing issues.
If you experience persistent symptoms such as chronic pelvic pain, sexual dysfunction, or urinary/fecal incontinence, it is advisable to consult a healthcare provider for a proper evaluation and diagnosis.
Yes, pudendal nerve-related conditions can affect individuals of all genders. While some symptoms may vary between males and females, both can experience pudendal nerve dysfunction and related issues.
Alcock’s canal, also known as the pudendal canal or pudendal tunnel, is a narrow passageway in the pelvic region where the pudendal nerve travels. Compression or entrapment of the pudendal nerve within Alcock’s canal can lead to pudendal neuralgia and related symptoms.
Physical therapy, often called pelvic floor physical therapy, can be instrumental in treating pudendal nerve dysfunction. Therapists use specialized techniques to address muscle imbalances, improve pelvic floor muscle function, and alleviate pain in the pelvic region.
Lifestyle modifications such as avoiding prolonged sitting, using cushioned seats, practicing relaxation techniques, and maintaining a healthy diet can help manage symptoms and reduce discomfort associated with pudendal nerve issues.
Prolonged pressure on the perineal area during cycling can contribute to pudendal nerve-related problems. To prevent these issues, cyclists can use anatomically designed saddles, wear padded shorts, adjust their bike setup for comfort, and take regular breaks during long rides.
Depending on the particular illness and its severity, the prognosis varies. Many individuals with pudendal nerve issues experience improvement or relief of symptoms with appropriate treatment.
Yes, there are support groups and patient advocacy organizations. That provide resources, information, and community for individuals dealing with pudendal nerve-related issues. These groups can offer valuable support and information for those seeking help and connection.
In some cases, surgical interventions may consider to address underlying issues such as nerve compression or entrapment. However, surgery is typically reserve for cases where conservative treatments have not been effective, and the benefits outweigh the risks.
Living with chronic pain or pelvic dysfunction can have emotional and psychological effects. Individuals with pudendal nerve-related conditions may experience anxiety, depression, or stress. It’s essential to address these aspects of well-being as part of a comprehensive treatment plan.
Seeking care from healthcare providers with expertise in pelvic pain or urogynecology can be beneficial. Referrals from primary care physicians or online resources from reputable medical institutions can help you find specialists in your area.
Reference
Pudendal Nerve. (n.d.). Physiopedia. https://www.physio-pedia.com/Pudendal_Nerve
The Pudendal Nerve – Anatomical Course – Functions – TeachMeAnatomy. (2019, December 4). TeachMeAnatomy. https://teachmeanatomy.info/pelvis/other/pudendal-nerve/
Professional, C. C. M. (n.d.). Pudendal Nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22000-pudendal-nerve#:~:text=The%20pudendal%20nerve%20provides%20most,to%20have%20or%20enjoy%20sex.
Pudendal nerve. (2023, July 11). Wikipedia. https://en.wikipedia.org/wiki/Pudendal_nerve