Boutonniere Deformity
Table of Contents
Introduction
Boutonniere deformity is a clinical condition that primarily affects the fingers, particularly the middle and proximal interphalangeal joints. This deformity is characterized by a specific pattern of flexion and extension abnormalities in the finger joints, resulting in a distinctive appearance that resembles the buttonhole of a garment (hence the name “boutonniere,” which means buttonhole in French).
This deformity can be caused by various underlying conditions, including traumatic injuries, rheumatoid arthritis, and congenital anomalies. Understanding the pathophysiology and treatment options for boutonniere deformity is crucial for healthcare professionals in order to provide effective care and improve patients’ quality of life.
- This deformity is characterized by flexion of the proximal interphalangeal joint (PIP) and hyperextension of the distal interphalangeal joint (DIP) due to volar subluxation of the lateral bands.
Definition
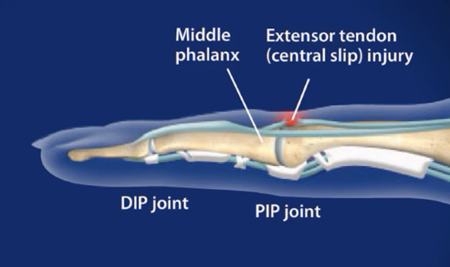
- Boutonniere deformity is a finger deformity in which the proximal interphalangeal joint (PIP) is flexed and the distal interphalangeal joint (DIP) is hyperextended. This is an extensor tendon injury. This is also called the “buttonhole deformity”.
Clinically relevant anatomy
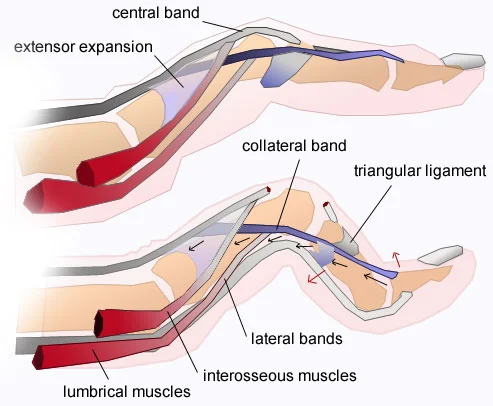
- The extensor digitorum communis (EDC) tendon in each finger is divided into three groups or slips, namely the medial tendon/slip, which inserts at the root of the middle finger, and two lateral tendons/slips, which join to form the terminal tendon/ to slide base of the distal phalanx.
- To achieve an actively interphalangeal stretch, the EDC muscle requires the assistance of two intrinsic muscle groups, the interossei, and psoas, which also have attachments to the extensor hood and lateral bands/glides.
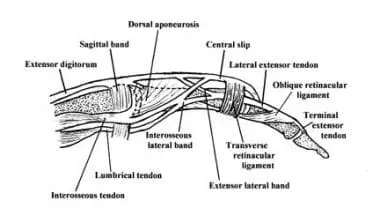
- The EDC tendon and all of its complex active and passive movement at the metacarpophalangeal joint and beyond are collectively known as the extensor mechanism. The base of the extensor mechanism is formed by the tendons of the EDC muscle (extensor indices and extensor digiti minimi) and the extensor tendon, medial tendon/glide, and lateral bands/glide that fuse with the terminal tendon/glide.
- The triangular bandage helps to stabilize the ligaments on the back of the finger. The triangular ligament provides stability to the collateral ligaments, preventing palmar subluxation during flexion of the proximal interphalangeal joint.
Cause
- Boutonniere deformity (BD) can occur secondary to extensor mechanism trauma (including direct extensor mechanism tear), rheumatoid arthritis (RA), and burns. There have also been documented reports of congenital Boutonniere malformations. The pathogenesis of BD varies according to its etiology.
- Patients with traumatic BD may have suffered a direct injury to the central slip or a force causing stretching of the central slip causing failure of the extensor mechanism. If tears prevent environmental sliding, immediate injuries can occur. Key injuries can also occur with passively forced flexion of an actively extended PIP joint. In another scenario, a volar dislocation of the PIP joint can impinge on the dorsal lip of the base of the middle phalanx and cause central slip disease.
- Boutonniere deformities develop in patients with rheumatoid arthritis and progress when the soft tissues of the finger are damaged. The extension mechanism is stressed as a result of the synovial proliferation of the proximal interphalangeal joint (PIP). As a result, the mid-slip is compromised and unable to achieve full extension, resulting in a slight delay in extension. When the PIP joint is slightly flexed, the collateral ligaments are subluxated and attached to the axis of rotation. In addition, the oblique ligaments of the retinaculum contract, resulting in hyperextension and limited flexion at the DIP joint. In the early stages of rheumatoid arthritis, the joints continue to be passively repaired, but as the disease progresses and the capsular tissues contract and fibrosis occurs around the PIP joint, the deformity is corrected.
Boutonniere deformities that occur after burns can result from direct trauma or from a central slip or infection.
- because of a condition like rheumatoid arthritis.
- A strong blow to the back of the middle joint of the finger.
- Wound wound in the middle of the slide.
- Finger fractures.
- Osteoarthritis.
- Sports-related injuries.
- PIP joint dislocation.
- Trapped finger, tendon injury and can cause boutonniere deformities. Secondary burn.
Mechanism
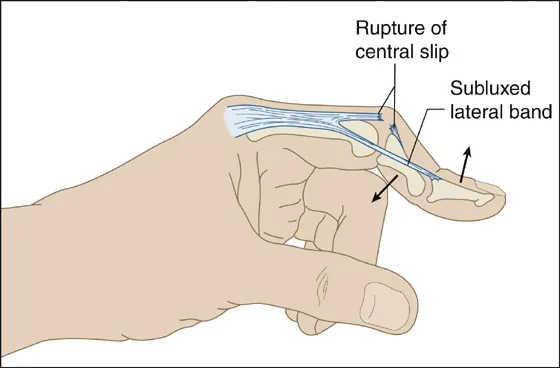
- If the medial slider of the digital extension tears, there is minimal deformation as long as the transverse fibers of the extension remain intact. If they are also torn, a deformity occurs in the PIP joint.
- In this case, all the extensor force is transmitted to the distal end through the intact collateral ligaments, causing hypertension of the DIP joint. The PIP joint compresses to flex and extends through the slot in the extension cap. The two lateral bands now run at the palmar aspect of the PIP joint and exaggerate flexion.
Signs and symptoms
Signs of classic boutonnière deformity may appear immediately after injury to the finger or 10–14 days after the initial injury.
- Loss of PIP joint extension and DIP joint hyperextension
- The middle joint (PIP) cannot be extended and the tip of the finger (DIP joint) cannot be bent
- Weak grip and inability to grasp and manipulate small objects with the tip of the digit
- Swelling and pain occur and persist at the top of the middle joint of the finger.
- Pain and discomfort persist over the middle joint of the finger.
- The patient may experience swelling. Stiffness can occur if the deformed posture is not treated. The middle joint cannot be straightened. The fingertip cannot be bent. Difficulty washing your face, writing, grabbing clothes, reaching into your pocket to remove your phone or wallet, etc.
Pathology
- Boutonniere deformity occurs when the central gliding of the tendon is interrupted. This tendon tear causes volitional movement of the collateral ligaments. This results in forced flexion of the finger, which limits the range of motion of the DIP joint. It could develop as a result of a burn or rheumatoid arthritis (RA). In inflammatory arthritis, such as rheumatoid arthritis, inflammatory cells accumulate in the synovial fluid of the joint and form a layer of fibrous tissue that leads to bone erosion that causes cartilage and ligament damage. This causes the joints to gradually deform, leading to loss of function and pain.
Diagnosis Of Boutonniere Deformity
- X-rays
- An x-ray is needed to see if it is an avulsion fracture.
.There are two specific tests to identifying injury to the extensor mechanism:
Elson’s test – Fix the PIP joint at a 90° angle and ask the patient to extend the DIP joint. A loose DIP joint even when the patient tries to extend is a negative or normal finding (if the medial slip is intact, loose lateral bands/slips in PIP flexion prevent DIP extension). A positive finding is a stiff DIP joint due to increased unrestrained traction through the collateral ligaments/glides.
Boyes Test – Extend PIP and request flexible DIP; positive cannot actively flex DIPThe Boyes test can become positive only at a late stage.
Treatment of boutonniere deformity
Treatment of Boutonniere deformities associated with rheumatoid arthritis
- Treatment options include long-term immobilization or surgery for patients who need to be evaluated for a chronic injury such as rheumatoid arthritis.
| Step | PIP joint | DIP joint |
| 1 – light, Passively repairable, Normal articular surface. | Splint Injection and/or synovectomy | Extensortonotomy |
| 2 – moderate, Passively repairable, Normal articular surface. | Treat as step 1 ± extensor tendon reconstruction | Extensortonotomy |
| 2 – moderate, Partially passively repairable, Normal articular surface. | Treat as step 1. Convert to repairable for extensor tendon reconstruction | Extensortonotomy |
| 2 – moderate or strongly fixed, Normal articular surface. | Treat as above if repairable → extensor reconstruction if not repairable → salvage → rarely releasing | Extensortonotomy |
| 3 – destruction of joints | Arthrodesis or arthroplasty | Extensortonotomy |
Conservative treatment Of Boutonniere deformity
Medicine:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), glucocorticoids, pain relievers, etc. NOTE: The medicine should not be taken without a doctor’s permission.
Immobilization
- In the case of a central gliding injury resulting from a simple detachment of the tendon from the bone, a splint for the PIP joint is recommended for 6 weeks thereafter, with the splint worn at night for several weeks. The splint allows movement in the DIP joint so exercises can be done to prevent stiffness. Some splints are similar to springs and can be used to gently stretch the PIP joint for several weeks to prevent contracture. The spring continuously applies gentle pressure that helps slowly straighten the PIP joint.
Surgical and Non-surgical Treatment of Boutonniere Deformity
- There are both surgical and non-surgical treatments. After surgery, a splint or brace is used for several weeks to keep the proximal interphalangeal joint straight, often followed by physical therapy. Casting is also a non-surgical treatment used for immobilization followed by exercises to improve the strength and flexibility of the affected finger. The aim of physiotherapy treatment is to restore full mobility and strength of the affected finger. If the injury occurs as a result of sports, the injured area may receive a splint or tape to protect it during the activity.
Although non-surgical treatment of Boutonnière’s deformity is preferred, surgery is possible in certain cases, such as:
- The deformity is caused by rheumatoid arthritis. The tendon breaks. There is a significant bone fragment out of place. The condition does not improve with a splint. Surgery can reduce pain and improve function, but it may not completely correct the condition and return the finger to normal. If a boutonniere deformity is left untreated for more than 3 weeks, it is much more difficult to treat.
Physical therapy treatment
Treatment of an acute injury is continuous loading of the PIP at full length for 6 weeks. Extensor laxity greater than 15° is a sign of a DIP joint tear with slight flexion for several weeks to allow healing. After 6 weeks of immobilization, exercises begin. The exercise includes two consecutive movements. The first is PIP joint extension with active assistance. This stresses tight volar structures, causes the collateral ligaments to run dorsally at the PIP joint, and places longitudinal stress on the collateral ligaments and oblique retinal ligaments. Another measure is maximal active forced flexion of the DIP joint, keeping the PIP joint at 0° or as close to this position as PIP allows. This gradually stretches the lateral bands and oblique retinal ligaments to their physiological length. Continue loading for 2-4 weeks if you are not training. If a full extension of the PIP joint can be maintained during the day, only a night splint is appropriate. The duration of treatment and loading can be several weeks.
Physiotherapy care of boutonniere deformity
- A physical therapist recommends exercises designed to work the hand and fingers so that work tasks and daily activities can be performed easily. They also help you find ways to do tasks in a way that doesn’t put too much stress on your knuckles.
Exercise interval training
Range of motion
A gentle range of motion can help maintain range of motion, flexibility, and mobility.
Strengthening exercises
Strengthening exercises usually occur 8-10 weeks after surgery. A variety of resistance movement exercises such as a push-up ball, gel balls, etc. can be recommended.
Stretching exercises
Stretching exercises are performed in a PIP contracture before repair or reconstruction. To increase the fingers’ strength and flexibility, stretching activities are performed.
MCPJ flexion and extension
Bend your fingers at the knuckles, making sure to keep your fingers straight. Hold this position for 5 seconds and then stretch. Repeat this 10 times and repeat for 1-2 hours.
DIPJ flexion and extension
Bend the fingertip over the edge of the splint and hold for 5 seconds, extend the fingertip and hold for 5 seconds. Hold the splint with your other hand and keep the splint straight. Repeat this 10 times and do this for 1-2 hours.
PIPJ flexion and extension
When using a splint, bend the finger at the middle joint and allow the splint to return the finger to a straight position. Repeat 10 times and do this for 1-2 hours.
Patient Education
Pain can be reduced and function can be improved with surgery, but the condition may not be completely cured. If a deformity is not treated for more than 3 weeks, it can become much more difficult to treat.
FAQ
Boutonnière’s deformity is a type of joint damage that mainly occurs in the fingers, but can also occur in the toes. This can be caused by injuries such as burns cuts or rheumatoid arthritis. The medial joint becomes immobilized and the articular end hyperextends.
The French term for “buttonhole flower” is where the word “boutonnière” originates. Like wedding bouquets, boutonnières were also used in the 16th century to ward off bad luck and evil spirits. It was also used to ward off bad odor and was thought to protect against disease.
The mainstay of nonoperative treatment of boutonnier malformations is loading. If the patient has an acute closed central slide injury, it has been recommended that PIPJ be extended to six weeks full-time and an additional six weeks at night.
Recovery from a boutonniere deformity takes anywhere from three weeks to several months, depending on the severity of the condition. If the first treatment is ineffective, the doctor may prescribe additional treatment, such as a night splint or support.
Reference
Boutonniere Deformity. (n.d.). Physiopedia. https://www.physio-pedia.com/Boutonniere_Deformity
What is Boutonniere Deformity? Symptoms, Causes, Diagnosis & Physiotherapy Treatment of Boutonniere Deformity. . .. . . (n.d.). Cbphysiotherapy. https://cbphysiotherapy.in/condition/boutonniere-deformity
Boutonniere Deformity of the Finger. (n.d.). https://www.galenasport.com/Injuries-Conditions/Hand/Hand-Issues/Boutonniere-Deformity-of-the-Finger/a~283/article.html
Clinic, M. P. (2023, August 1). Boutonniere Deformity. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/boutonniere-deformity/