Sarcoid Arthritis
Table of Contents
What is sarcoid arthritis?
Sarcoidosis is a heterogeneous multisystem granulomatous disease that primarily affects the lungs and lymphatic system, which is characterized by its pathological hallmark, the non-caseating granuloma.1 Arthritis is found in 15–25% of patients with sarcoidosis.
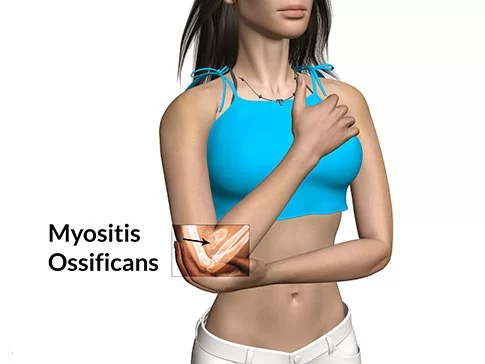
Sarcoidosis can involve the joints, bones, and muscles. This causes a wide variety of musculoskeletal complications that act through different mechanisms.
Two major types of arthritis have been significantly distinguished:
- the acute transient type
- the persistent or chronic type.
The acute form is the most general rheumatic manifestation of sarcoidosis, frequently being the presenting manifestation of the disease and generally having a favorable outcome. Löfgren first explained its presentation as a triad with bilateral hilar adenopathy & erythema nodosum. The chronic type of arthritis begins either early or late during the course of sarcoidosis, which is generally active in other organ systems.
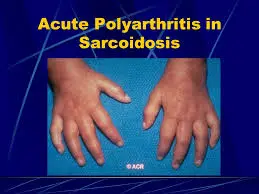
Sarcoidosis patients with acute arthritis frequently also have bilateral hilar lymphadenopathy and erythema nodosum. These three associated syndromes often occur combine in Löfgren syndrome.
The arthritis symptoms of Löfgren syndrome occur most often in the ankles, followed by the knees, wrists, elbows, and metacarpophalangeal joints. Usually, true arthritis is not present, but instead, periarthritis appears as a swelling in the soft tissue around the joints that can be seen by ultrasonographic methods.
These joint symptoms tend to occur at the same time as erythema nodosum develops. Even when erythema nodosum is absent, it is believed that the combination of hilar lymphadenopathy and ankle periarthritis can be considered a variant of Löfgren syndrome.
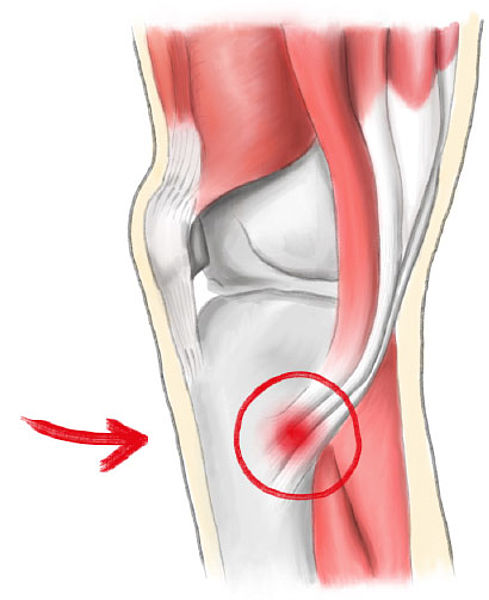
Enthesitis also occurs in about one-third of patients with acute sarcoid arthritis, mainly affecting the Achilles tendon and heels. Soft-tissue swelling of the ankles can be prominent, and a biopsy of this soft tissue reveals no granulomas but does show panniculitis similar to erythema nodosum.
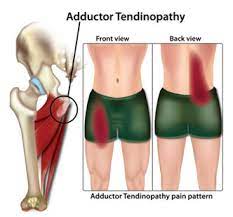
Chronic arthritis usually occurs in the setting of more diffuse organ involvement. The ankles, knees, wrists, elbows, and hands might all be affected in the chronic form and often this presents itself in a polyarticular pattern.
Dactylitis similar to that seen in psoriatic arthritis, which is associated with pain, swelling, overlying skin erythema, and underlying bony changes may also occur. Development of Jaccoud arthropathy is very rarely seen.
The most frequent areas of involvement are the hands and feet, whereas the spine is not commonly affected. around half of the patients with bony lesions experience pain and stiffness, whereas the other half stay asymptomatic. Periostitis is rarely seen in sarcoidosis and has been found to be present in the femoral bone.
It is unknown whether, & to what extent, acute sarcoid arthritis can be differentiated from other forms of arthritis by its presenting clinical features.
What are the symptoms of sarcoid arthritis?
In the majority of the patients with sarcoid arthritis, the joint symptoms started symmetrically in the large joints of the leg. The arthritis was monoarticular in one patient, oligoarticular (two to four joints) in patients (87%), and polyarticular in six patients. The ankle was affected in (98%) of patients at the first visit, with the majority having to swell in both ankles. One presented with arthritis of the right wrist without ankle involvement. Arthritis of the small hand joints was also found, all of whom had symmetrical polyarthritis including bilateral ankle involvement. Half of the patients had fevers. Skin abnormalities often found were erythema nodosum in inpatients and a red-bluish discoloration around the ankles in. Enthesopathy mainly located at the Achilles tendons and heels was present in the patients. Some patients had symptoms of slight cough or dyspnoea at entry.
Articular Involvement
Up to one-fourth of patients with sarcoidosis have joint involvement. Japanese populations with sarcoidosis are a notable exception, with very few cases of sarcoid arthritis reported.
Traditionally, sarcoidosis arthritis is divided into two types: an acute, transient type, or a persistent, and chronic type. The second type is rare, occurring in only 1 to 4% of patients.
Acute sarcoid arthritis
Acute sarcoid arthritis frequently occurs in the context of Löfgren syndrome, which is defined as the triad of erythema nodosum, bilateral hilar lymphadenopathy, and the presence of arthritis or arthralgias. A seasonal association between the starting presentation of acute sarcoid arthritis has been reported. Evidence suggests that initial presentations are clustered in the springtime, a notable distinction from other arthritides, which tend to occur equally throughout the year.
Visser and colleagues proposed a set of criteria for clinicians to use as a model to help diagnose sarcoid arthritis. According to these criteria, making a diagnosis of articular sarcoidosis in patients who have three of the following four characteristics is 99% sensitive and 93% specific:
(1) erythema nodosum,
(2) symptom duration less than 2 months,
(3) age less than 40, &
(4) symmetrical ankle arthritis.
Involvement of the ankle in acute sarcoid arthritis has been reported in patients, & symmetrical involvement occurs in most of those cases. Following the ankle, the next most common sites of pain and inflammation are the knee, wrist, & metacarpophalangeal joints. Patients frequently have an increased erythrocyte sedimentation rate, but other associated findings in acute sarcoid arthritis might vary among patients. For example, erythema nodosum might or might not be present. In the literature, the incidence is wide-ranging. Similarly, fever is notable in only one-third of patients in some reports but in up to two-thirds of patients in other case series.
In the vast majority of cases, acute sarcoid arthritis has a benign, self-limited course, with minor to no joint destruction. The average time period of symptoms is approximately 2 to 3 months, and most patients go into revocation by 6 months after receiving nonsteroidal anti-inflammatory drugs or steroids.
Chronic sarcoid arthritis
Chronic sarcoid arthritis typically occurs in the setting of systemic sarcoidosis. Chronic sarcoid arthritis typically involves the knees, ankles, wrists, hands, and feet. Joint destruction or Jaccoud deformity, when it occurs, is because of persistent inflammation. Joint effusions, synovitis, or even nodular proliferation of the synovium presenting as an intraarticular knee mass might also be present. The differential diagnosis of chronic sarcoid arthritis includes reactive arthritis and rheumatoid arthritis, which should be considered, particularly if there is a symmetric disease and an elevated rheumatoid factor. Synovial fluid analysis typically discloses a milder inflammatory infiltrate in sarcoid arthritis than rheumatoid arthritis or infectious arthritis, although sometimes a synovial biopsy might be needed to definitely distinguish rheumatoid arthritis from sarcoid arthritis.
Monoarthritis, Oligoarthritis, Polyarthritis
The majority of cases of sarcoid arthritis, whether acute or chronic, are oligoarthritic or polyarthritic (eg., involving three or more joints). When patients with sarcoidosis present with symmetric polyarthritis, especially of the small joints of the hands, clinicians should check out patients for concomitant rheumatoid arthritis. Differentiating between the various types of arthritis should be based on clinical laboratory findings & radiographic imaging. Psoriatic arthritis, reactive arthritis, & gouty arthritis should also be considered in patients with sarcoidosis who present with oligoarthritis or monoarthritis. In immunocompromised patients, infectious arthritis needs to be eliminated.
Monoarthritis is rare, although the incidence is variable in reports, with one prospective study citing only one of 28 patients having single joint involvement and another study reporting 21% of patients with Löfgren syndrome with single joint involvement. Similar to a polyarthritis presentation, when patients present with monoarthritis they should be evaluated for gouty arthritis & septic arthritis as well as calcium pyrophosphate (CPP)-positive arthritis.
Periarthritis
Patients with sarcoid arthritis frequently have periarticular inflammation. In spite of swelling around the joints, individuals with periarthritis generally maintain a normal range of motion.
At times it might be difficult to distinguish between arthritis and periarthritis. Kellner and colleagues performed ultrasonography on patients who presented with sarcoidosis involving the joints. Most of the patients had subcutaneous or periarticular inflammation. Although some patients had tenosynovitis, only a few had discernible joint effusions. When diagnosing peri-arthritis, it is important to eliminate lymphangitis, gonococcal infection, and human immunodeficiency virus (HIV) infection, especially in those who might be at risk for developing these infections.
What are the causes of sarcoid arthritis?
The exact cause of sarcoidosis is not known. The current working hypothesis is, that in genetically susceptible individuals, sarcoidosis is caused by an alteration to the immune response after exposure to an environmental, occupational, or infectious agent. Some cases may be acquired by treatment with tumor necrosis factor (TNF) inhibitors like etanercept.
The presence of these genetic components and disease in more than one family member is usually related to antigens of the major histocompatibility complex (MHC), especially DR alleles. The heritability of sarcoidosis varies according to nationality.
Various microorganisms like mycobacteria and propionibacteria have been associated with the disease. Possible infective etiology has been described in a few studies where sarcoidosis developed in a previously negative individual after cardiac or bone marrow transplantation, but none of the known relations is specific enough to suggest a direct causative role.
The most implicated infectious agents include mycobacteria, borrelia, fungi, and rickettsia. A meta-analysis investigating the role of mycobacteria in sarcoidosis found it was present in some cases. Still, they also detected a possible publication bias, so the results need further confirmation.
Mycobacterium tuberculosis catalase-peroxidase has been recognized as a possible antigen catalyst of sarcoidosis. The disease has also been reported by transmission through organ transplants.
Association of autoimmune disorders has been frequently observed. The exact mechanism of this relation is not well familiar, but some evidence supports the hypothesis that this is a consequence of Th1 lymphokine prevalence. Cytokines including Th1, IL-2, IL6, IL 8, IL12, IL 18, IL 27, and interferon (IFN) gamma & tumor necrosis factor-alpha are closely associated with sarcoidosis.
Some of these are implicated in granuloma formation with macrophage and epithelioid accumulation, activation, and aggregation. Some of these interleukins are believed to act like disease modifiers. Tests of delayed cutaneous hypersensitivity have been utilized to measure progression.
On histopathology, classic sarcoid granulomas are non-necrotizing with a tightly packed central area composed of macrophages, epithelioid cells, multinucleated giant cells, & T lymphocytes that are CD4 positive. The central areas are surrounded by CD8 and CD4-positive T lymphocytes, B lymphocytes, monocytes, mast cells, & fibroblasts, which in turn are surrounded by lamellar rings of hyaline collagen. The amounts of lymphocytic infiltrate & fibrosis surrounding the granulomas vary depending on the patient and disease duration. Additional histopathologic characteristics of sarcoid granulomas that might be present include asteroid bodies, Schaumann bodies, & birefringent crystalline particles.
In rare patients with necrotizing sarcoid granulomatosis, the histopathology presents perivascular masses composed of confluent granulomas and necrosis of lung parenchyma.
What are the risk factors of sarcoid arthritis?
Smoking
A highly significant negative association between sarcoid arthritis and smoking was found in the study, suggesting that smoking decreases the incidence of clinically overt sarcoid arthritis. The connection was not influenced by sex and was even stronger in the age category 25–44 years, which contained the majority of the patients with sarcoid arthritis. Surprisingly, for a disease that in most cases affects the respiratory tract, relatively small attention has been given to the possible role of tobacco smoking in its pathogenesis. The patients with sarcoid arthritis in these two studies were distinguished in two important aspects from those of the other studies: in one study the majority of the patients were black and in the other study, a considerable proportion of the patients had advanced disease. In other studies, both aspects were found to reduce the negative association between smoking and sarcoid arthritis At the same time, it is the first report on smoking behavior in patients with the acute form of sarcoid arthritis, as all previous studies were done in patients attending clinics with pulmonary sarcoidosis. These results recommend that in acute sarcoid arthritis the lung is the starting point of the disease.
Seasonality
An evident clustering of the starting of the disease in the months of March to July was found in the study. The peak months in all studies were the months of elevated temperatures. In one study in the United States, the seasonal variation in the incidence of sarcoidosis was found to be minimal, with a tiny non-significant peak in spring. The observed seasonality suggests that an environmental factor, infective or not, might play a part in the pathogenesis of the disease. The finding that the peak months of disease onset in most studies are the months of increasing temperatures does not spot a particular infective agent. It is interesting, nevertheless, that the seasonal variation of sarcoid arthritis onset found in this study resembles the seasonal variation of tuberculosis onset reported in the United Kingdom. The peak for tuberculosis was found to take place in June, whereas for acute respiratory disorders it was in January or February.
HLA
The present study shows a highly significant relationship between the acute form of this disease and the presence of the DQ2-DR3 haplotype. The existence of an immunogenetic predisposition to sarcoidosis is likely on the basis of both different prevalences in different ethnic populations & the occasional familial clustering of cases. Because the pathophysiology of sarcoidosis probably includes antigen recognition, processing, and presentation, many studies have searched for associations with HLA-related genes. An allele commonly found to be associated with sarcoidosis is HLA-B8, which is in linkage disequilibrium with DQ2-DR3 in our population.
It is likely that genetic factors not only play a part in the susceptibility to the disease but might also be important in defining the pattern of disease presentation & progression as well as its overall outcome. A relationship between HLA-DR3 with the acute form of sarcoidosis and with a good prognosis, spontaneous resolution, and short duration of the disease was found in several studies. The relationship between HLA and susceptibility to the acute form of sarcoid arthritis was evaluated in four studies, all using serological typing. In all these studies significant relationships were found with HLA-B8/DR3. The present study, using molecular typing for DR and DQ, affirms the findings of the serological studies. Moreover, the study shows that the susceptibility to acute sarcoid arthritis as carried by the DQ2 -DR3 haplotype, appears to be transmitted as a dominant genetic trait.
A new finding is also the highly negative relationship that exists between acute sarcoid arthritis and smoking. It is suggested that the disease results from the exposure of genetically susceptible hosts to environmental agents through the lungs.
What is the prevalence of sarcoid arthritis?
Acute sarcoid arthritis was seen in (62.3%) of patients, while chronic arthritis occurred in (21.1%) of patients. Oligoarthritis was the most common pattern of joint involvement, & bilateral ankle arthritis was the prominent characteristic. The prognosis of sarcoid arthropathy was generally favorable, as arthritis resolved within six weeks in the majority of patients.
Arthritis occurred more frequently in females. It also occurred more often in patients with erythema nodosum, another condition seen in patients that involve red lumps on the lower legs.
“Inflammatory arthritis occurs in a majority of patients with sarcoidosis. Acute arthritis with bilateral ankle involvement is the most usual pattern of sarcoid arthropathy. Sarcoidosis can mimic many primary rheumatic diseases or might coexist with them., adding that a diagnosis of sarcoid arthropathy should be considered when sarcoidosis patients have complaints concerning their musculoskeletal system.
What is the diagnostic procedure for sarcoid arthritis?
A standard diagnostic investigation was performed at the first visit, including patient history, physical examination, & laboratory and radiological examination. Symmetrical ankle arthritis was the clinical symptom with the highest diagnostic value. It had a sensitivity of 95% and a specificity of 92%, resulting in a positive predictive value of 35% & a negative predictive value of 99.7%.
The best diagnostic criteria set consists of four variables: symmetrical ankle arthritis, symptom duration of fewer than two months, age below 40 years, & erythema nodosum. When test positivity was defined as the presence of at least three of four criteria, this diagnostic set gave a sensitivity of 93%, a specificity of 99%, a positive predictive value of 75%, & a negative predictive value of 99.7%.
An elevated erythrocyte sedimentation rate was found at the first visit in patients. None of the patients were markedly hypercalcaemic.
Chest radiographs were taken in the beginning in all patients. The sarcoid lung stages were divided according to the staging proposed by James and Thomson. All patients with sarcoid arthritis had, by definition, hilar adenopathy on the chest x-ray examination routinely carried out at admission. Parenchymal lung infiltrations (stage II) were present in patients; some of them had pulmonary symptoms at presentation.
Pulmonary function tests, performed in all patients with stage II chest x-ray findings, were normal in most patients and showed slight restrictive changes in combination with a normal carbon monoxide transfer factor in a few patients.
A histological examination was carried out on patients. Transbronchial biopsies were performed in patients, yielding non-caseating epithelioid cell granulomas in most cases and insufficient material in rare cases. In the patient, a liver biopsy was performed, yielding non-caseating epithelioid cell granulomas.
What is the treatment plan for sarcoid arthritis?
Medical treatment for sarcoid arthritis:
There are no U.S. Food & Drug Administration (FDA)-accepted therapies for sarcoidosis in general, or for any of its manifestations in particular. Our proposed attitude for the management of patients with sarcoid arthritis.
After establishing a diagnosis, first-line therapies involve nonsteroidal anti-inflammatory drugs (NSAIDs), local or low-dose systemic steroids, or methotrexate. Other agents might be considered depending on the severity of the signs & symptoms as well as the radiographic progression. Periodic disease assessments are needed to determine whether the response is adequate. If the response is adequate, we continue treating the first-line agents that are working well.
Nonresponders might be attempted on a higher dose of systemic steroids, or advanced directly to second-line treatments.
Second-line therapies involve methotrexate if patients are methotrexate-naïve or, in patients previously tried failed on methotrexate or intolerant to the drug, biologic therapies, an alternate disease-modifying antirheumatic drug (DMARD) monotherapy, or a combination of these treatments. Methotrexate has been utilized as an alternative to corticosteroids in the treatment of chronic & refractory sarcoidosis for years. It has proven to effectively control the disease in many patients.
Nevertheless, no studies have focused on its role in sarcoid arthritis in particular. It is benefits to patients with rheumatoid arthritis have been well documented over the past 40 years, & it is therefore considered first-line therapy in that disease setting. In spite of the clinical utility of DMARDs, randomized studies for some e.g., sulfasalazine, leflunomide, hydroxychloroquine, azathioprine, and minocycline are lacking in the sarcoidosis setting.
Even in the circumstances of rheumatoid arthritis, the evidence for sulfasalazine and minocycline aid comes from case reports. Keeping in mind that there is a lack of large, randomized trials evaluating the utilization of DMARDs in sarcoidosis, our recommended treatment algorithm proposes these agents in the first-line setting for some patients, depending on our own clinical experience.
Of note, clinicians should monitor patients’ progress & periodically check for toxicities. An approach for toxicity monitoring before starting therapy or increasing dosages of DMARDs was recently proposed by the American College of Rheumatology based on the rheumatoid arthritis literature. baseline interpretation of patients receiving DMARDs should include complete blood count (CBC), creatinine, hepatitis B and C testing, liver transaminase, & ophthalmologic evaluations. For patients failing second-line treatment, a distinct biologic agent, a trial of high-dose systemic steroids, or enrollment in a clinical trial should be contemplated.
Physiotherapy treatment for sarcoid arthritis:
Goals
- protect joint from further damage
- reduce swelling
- provide pain relief
- prevent deformity
- prevent disability
- improve functional capacity
- improve flexibility and strength
- encourage regular exercise
- improve general fitness
Management
- cryotherapy
- TENS for pain relief
- gentle assisted movements through a normal range
- isometric (static muscle contraction) helps to maintain muscle tone without elevating inflammation
- core stability exercise
- gentle stretches to tight large muscles
regular exercise can help
- maintaining muscle strength is important for joint stability and preventing injury
- muscles can become weak following decreased activity
- pain signals from nerves & swelling can both inhibit muscles
- muscle length can be affected by prolonged positions and immobilizations and tightness can limit daily activities
relaxation therapies for generalized relaxation and stress relief
Occupational Therapy for splints and adaptive devices
Treatment should be initiated early and should be individualized.
FAQ (frequently asked questions)
Is rheumatoid arthritis the same as sarcoid arthritis?
RA and sarcoidosis are two different conditions and it is obvious that they do not have a common genetic base. Both are related to alleles that code major histocompatibility complex (MHC) class-II.
How do you know what stage of sarcoidosis you are in?
The Siltzbach classification system ranges from stage 0 to 5 based on the sites of the granulomas. The staging is determined using a chest X-ray, or radiography, an imaging test that utilizes low doses of radiation to form an image of the structures in the chest. The granulomas can be seen in this image.
Do you see a rheumatologist for sarcoidosis?
Sarcoidosis is a systemic inflammatory granulomatous condition for which rheumatologists are uniquely trained & qualified to treat.