Tuberculosis
- Tuberculosis is a bacterial infection that is also called TB. It can be fatal if not treated. TB (Tuberculosis) most often affects your lungs, but can also affect other organs like your brain.
- Tuberculosis (TB), once known as consumption, is a highly infectious disease that primarily affects the lungs.
- Maintaining to the World Health Organization (WHO)Trusted Source, 1.5 million people died from the disease in 2020. Tuberculosis is the 13th leading cause of death globally. Currently, it is the second main infectious cause of death, later COVID-19.
- TB is most common in developing countries, yet according to the Centers for Disease Control and Prevention (CDC)Trusted Source, over 7,000 cases were reported in the United States (US) in 2020.
- Tuberculosis is commonly curable — and preventable — under the right conditions.
Table of Contents
What is Tuberculosis?
- Tuberculosis is an infectious disease that can cause disease in your lungs or another tissue. It commonly affects your lungs, yet it can also affect other organs like your spine, brain, or kidneys. The word “tuberculosis” comes from the Latin word for “nodule” or something that sticks out.
- Tuberculosis is also called TB. Not everyone who becomes infected with TB gets sick, yet if you do get sick you need to be treated.
- If you are infected with the bacterium but do not have symptoms, you have inactive tuberculosis or latent tuberculosis infection (also called latent TB). It may seem like TB (Tuberculosis) has gone away, but it is dormant (sleeping) inside your body.
- If you are infected, develop symptoms, and are contagious, you have active tuberculosis or tuberculosis disease (TB disease).
The three stages of TB (Tuberculosis) are:
- Primary infection.
- Latent TB infection.
- Active TB disease.
How common is tuberculosis?
- About 10 million people became unwell with TB (Tuberculosis) throughout the world, and about 1.5 million people died from the disease in 2020. TB (Tuberculosis) was once the conducting cause of death in the U.S. (America) yet the number of cases fell rapidly in the 1940s and 1950s later researchers found treatments.
- Statistics view that there were 7,860 tuberculosis cases reported in the U.S. in 2021. The national occurrence rate is 2.4 cases per 100,000 people.
Are there different kinds of tuberculosis?
- In addition to active or inactive, you might hear about different kinds of TB (Tuberculosis), including the most common, pulmonary (lung) tuberculosis. Yet the bacterium can also harm other parts of your body besides the lungs, causing extrapulmonary tuberculosis (or TB outside of the lung). You might also hear about systemic miliary tuberculosis (TB), which can spread throughout your body and cause:
- Meningitis: inflammation of your brain.
- Sterile pyuria: or high levels of white blood cells (WBCs) in your urine.
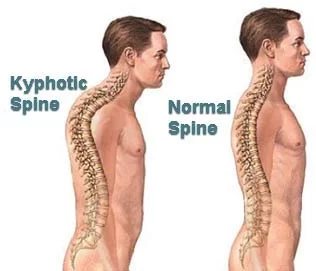
- Pott’s disease: also known as spinal tuberculosis or tuberculosis spondylitis.
- Addison’s disease: an adrenal gland condition.
- Hepatitis: a liver infection.
- Lymphadenitis in your neck is also called scrofula or TB (Tuberculosis) lymphadenitis.
What causes tuberculosis?
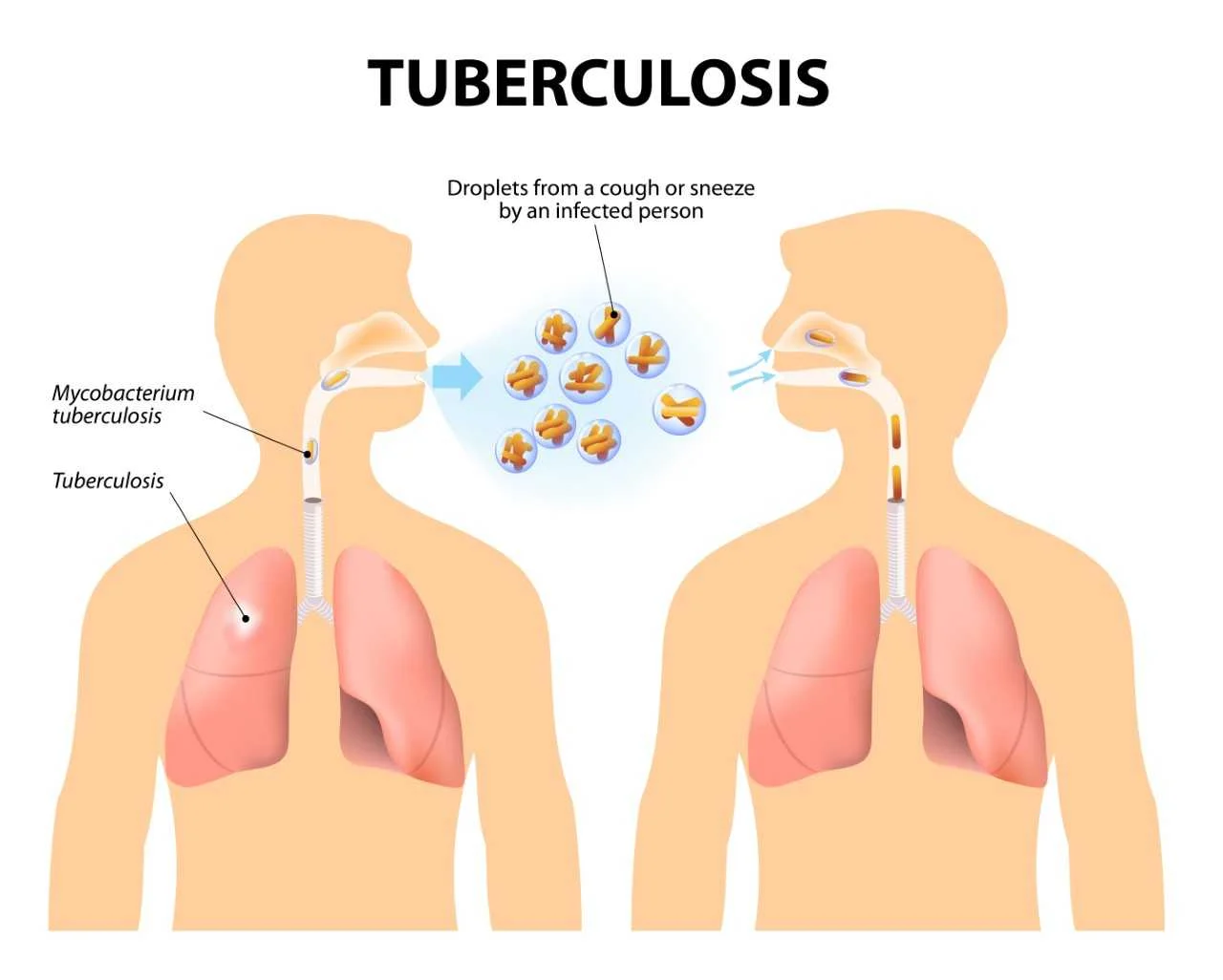
- TB (tuberculosis) is caused by the bacterium Mycobacterium tuberculosis (TB). The germs are spread through the air and commonly infect the lungs, but can also infect other parts of the body. Although TB (tuberculosis) is infectious, it does not spread easily. You commonly have to spend a lot of time in contact with someone who is contagious in order to catch it.
- Tuberculosis is spread by airborne particles called droplet nuclei (spread when infected people sneeze, laugh, speak, sing, or cough).
- In order to contract this disease, a person has to have prolonged exposure to an infected person in an enclosed space.
- It is suspected that there could be a genetic component to susceptibility and resistance, yet that has yet to be proven.
- In certain countries, it is common for bovine TB (Tuberculosis) to be spread through unpasteurized milk and other dairy products due to cattle with tuberculosis.
- The organism has several unique features compared to other bacteria like the presence of several lipids in the cell wall including mycolic acid, cord factor, and Wax-D. The increased lipid content of the cell wall is thought to contribute to the following properties of M. tuberculosis (TB) infection:
- Resistance to many antibiotics,
- Difficulty staining with Gram stain and many other stains,
- Ability to survive under extreme conditions such as extreme acidity or alkalinity, decrease oxygen situation, and intracellular survival(within the macrophage).
- A reason the bacteria is able to be dormant in someone for years and is able to survive for months in phlegm that is not exposed to sunlight and is trapped within the body (primary TB (Tuberculosis)). Once the person’s resistance is lowered, the TB can become active (secondary TB (Tuberculosis)). This could be caused by advancing age, alcoholism, cancer, or immunosuppression.
How is tuberculosis spread?
- TB (tuberculosis) can be spread when a person with active TB (tuberculosis) disease releases germs into the air through coughing, sneezing, talking, singing, or even laughing. Only people with the active pulmonary infection are contagious. Most people who breathe in TB (tuberculosis) bacteria are able to fight the bacteria and stop it from growing. The bacterium becomes inactive in these individuals, causing a latent TB (tuberculosis) infection.
- As many as 13 million people in the U.S. have latent TB (tuberculosis). Although the bacteria are inactive, they still remain alive in the body and can become active after. Some people can have a latent TB (tuberculosis) infection for a lifetime, without it ever becoming active and developing into TB (tuberculosis) disease.
- However, TB (tuberculosis) can become active if your immune system becomes weakened and cannot stop the bacteria from growing. This is when the latent TB (tuberculosis) infection becomes active TB (tuberculosis). Many researchers are working on treatments to stop this from occurring.
What are the signs and symptoms of tuberculosis?
- People with inactive TB (tuberculosis) do not exhibit symptoms. However, they may have a positive skin reaction test or blood test (BT).
- Some people who acquire Mycobacterium tuberculosisTrusted Source, the bacterium that causes TB (Tuberculosis), do not experience symptoms. This condition is known as latent TB (Tuberculosis). TB (Tuberculosis) can stay dormant for years before developing into active TB (Tuberculosis) disease.
- Active TB (Tuberculosis) typically causes many symptoms. While symptoms usually relate to the respiratory system, they could affect other parts of the body, depending on where the TB (Tuberculosis) bacteria grow.
Those with active TB (tuberculosis) can show any of the following symptoms:
- Bad cough (lasting longer than two weeks),
- Pain in your chest
- Coughing up blood or sputum (mucus)
- Fatigue or weakness
- Loss of appetite
- Weight loss
- Chills
- Fever
- Night sweats.
- A chronic cough, hemoptysis, weight loss, low-grade fever, and night sweats are some of the most usual physical findings in pulmonary tuberculosis.
- Secondary tuberculosis (TB) differs in clinical presentation from primary progressive disease. In secondary disease, the tissue reaction and hypersensitivity are more severe, and patients commonly form cavities in the upper portion of the lungs.
- Pulmonary or systemic dissemination of the tubercles may be looked at in active disease. Disseminated tuberculosis (TB) may also be seen in the spine, the central nervous system, or the bowel.
- There are commonly no symptoms of tuberculosis during the first year of exposure. This is when the disease would be the most preventable.
Symptoms suggestive of TB (tuberculosis) involve:
- Productive cough that lasts longer than three weeks,
- Weight Loss,
- Fever,
- Night sweats,
- Fatigue,
- Malaise,
- Anorexia,
- Rales could be heard in the lobes of the involvement in the lungs,
- Bronchial Breath Sounds,
- Dull chest pain, tightness, or discomfort,
- Dyspnea,
- Haemoptysis (late-stage symptom),
- Systemic Involvement.
- 10%-15% of tuberculosis (TB) is extra-pulmonary. It can grow through the blood vessels from organ to organ and/or the lymphatic system.
Extra-pulmonary TB (tuberculosis) can involve the:
- Kidneys,
- Bone Growth Plates,
- Lymph Nodes,
- Meninges,
- Hip Joints – can source avascular necrosis of the hip,
- Elbows,
- Vertebrae (Pott’s Disease).
What kinds of tests are used to diagnose tuberculosis (TB)?
- There are two kinds of screening tests for TB (tuberculosis): the Mantoux tuberculin skin test (TST) and the blood test, called the interferon-gamma release assay (IGRA).
- For the TST (tuberculin skin test), a healthcare provider will inject a small amount of a substance called purified protein derivative (PPD) under the skin of your forearm. Later two to three days, you must go back to the healthcare provider (doctor), who will look at the injection site.
- For the IGRA (interferon-gamma release assay), a healthcare provider (doctor) will draw blood and send the sample to the lab.
Further tests to determine if an infection is active or if your lungs are infected involve:
- Lab tests on sputum and lung fluid,
- Chest X-ray,
- Computed tomography (CT) scans,
How do I know if I should acquire tested for tuberculosis?
You may want to get tested for TB (tuberculosis) if:
- You are a resident or employee in group settings where the risk is high, like jails, hospices, skilled nursing facilities, shelters, and other healthcare facilities.
- You work in a mycobacteriology laboratory.
- You have been in contact with someone who’s known or suspected to have TB (tuberculosis) disease.
- Your body’s resistance to illness is decreased because of a weak immune system.
- You think you might already have TB (tuberculosis) disease and have symptoms.
- You are from a region or have lived in a region where TB (tuberculosis) disease is prevalent, such as Latin America, the Caribbean, Africa, Asia, Eastern Europe, and Russia.
- You have injected recreational drugs.
- Your healthcare provider (doctor) recommends testing.
Others who are at risk for TB (tuberculosis) involve:
- People with immature or impaired immune systems, like babies and children.
- People with kidney disease, diabetes, or other chronic (long-term) illnesses.
- People who have received organ transplants.
- People are being treated with chemotherapy for cancer or other types of treatments for immune system disorders.
- The occurrence rates for minority groups in the U.S. (America) are higher than the incidence rates for whites.
Risk factors that increase your chance of contracting the bacteria that causes TB (tuberculosis) disease include:
- having diabetes, end-stage kidney disease, or some cancers,
- malnutrition,
- using tobacco or alcohol for long periods of time,
- a diagnosis of HIV or having other immune-system-compromising situations.
- Medications that suppress the immune system can also put people at risk of developing active TB (tuberculosis) disease. These include medications that assist prevent organ transplant rejection.
Other medications that increase your risk of active TB (tuberculosis) include those taken to treat:
- cancer
- rheumatoid arthritis
- Crohn’s disease
- psoriasis
- lupus.
- According to the WHOTrusted Source, more than 95 percent of all TB (tuberculosis)-related deaths occur in developing countries.
- Traveling to regions with high TB (tuberculosis) rates can also increase your risk of contracting the bacterial infection.
These regions involve:
- sub-Saharan Africa
- India
- Mexico and other Latin American countries
- China and many other Asian countries
- areas of Russia and other countries of the former Soviet Union
- islands of Southeast Asia
- Micronesia.
- Many lower-income U.S. households have limited access to resources, involving healthcare, needed to diagnose and treat TB (tuberculosis), which puts them at greater risk of developing active TB (tuberculosis) disease.
- People experiencing homelessness and people living in congregate settings, involving jails, prisons, and correctional facilities, have a higher risk of contracting the bacterial infection.
HIV and TB (tuberculosis)
- People living with HIV are at higher risk of contracting the infection and dying from TB (tuberculosis). In fact, TB (tuberculosis) is the leading cause of death of HIV-positive people, according to the WHOTrusted Source.
- Untreated latent TB (tuberculosis) is more likely to progress to active TB (tuberculosis) in a person living with HIV. That makes testing for TB (tuberculosis) essential for anyone with HIV-positive status.
People living with HIV can take a few important steps to assist reduce the risk of contracting this bacterial infection:
- Getting tested for TB (tuberculosis),
- Taking HIV medication as advised by healthcare professionals (doctors),
- Avoiding being in close proximity to someone with TB (tuberculosis),
- Trying to stop smoking — smoking can both raise the risk of developing TB (tuberculosis) and reduce the response to HIV and TB (tuberculosis) treatment,
- Eating a nutrient-rich, balanced diet to assist reduce the risk of complications from HIV and improve medication absorption,
- Getting regular exercise, if possible, to encourage immune system health.
Epidemiology
- Tuberculosis (TB) is present globally. However; developing countries account for a disproportionate share of the tuberculosis disease burden. The bulk of the global burden of new infection and tuberculosis death is borne by developing countries with six countries: India, Indonesia, China, Nigeria, Pakistan, and South Africa, accounting for 60% of TB (Tuberculosis) death in 2015, Several countries in Asia, Africa, Eastern Europe, and Latin and Central America continue to have an unacceptably high burden of tuberculosis (TB).
- In more advanced countries, high-burden tuberculosis (TB) is seen among recent arrivals from tuberculosis-endemic zones, healthcare workers, and HIV-positive individuals. The use of immunosuppressive agents like long-term corticosteroid therapy has also been associated with an increased risk.
TB (Tuberculosis) in Prisons
- The level of TB (Tuberculosis) in prisons has been reported to be up to 100 times higher than that of the civilian population.
- Cases of TB (Tuberculosis) in prisons may account for up to 25% of a country’s burden of TB.
- Late diagnosis, inadequate treatment, overcrowding, poor ventilation, and repeated prison transfers encourage the transmission of TB (Tuberculosis) infection.
- HIV infection and other pathology more usual in prisons (e.g. malnutrition, substance abuse) encourage the development of active disease and further transmission of infection.
- Multi-drug resistant tuberculosis (TB) (MDR-TB) in prisons High levels of MDR-TB (Tuberculosis) have been reported in some prisons with up to 24% of TB (Tuberculosis) cases suffering from MDR forms of the disease.
Associated Co-morbidities
- HIV/AIDS – due to comprised immunosuppressive system,
- Rheumatoid Arthritis – due to immunosuppressive treatments,
- Diabetes Mellitus,
- End-stage Renal Disease,
- Gastrointestinal Disease,
- Alcoholism,
- Cancer – because of chemotherapy, radiation, or steroid therapy,
- Malnutrition.
How is tuberculosis treated?
TB (tuberculosis) infection and disease are treated with these drugs:
- Isoniazid (Hyzyd)
- Rifampin (Rifadin)
- Ethambutol (Myambutol)
- Pyrazinamide (Zinamide)
- Rifapentine (Priftin).
- You must take all of the medication your provider (doctor) prescribes, or not all of the bacteria will be killed. You will have to take these medications for as long as you are told — sometimes up to 9 months.
- Some forms of TB (tuberculosis) have become resistant to medications. It is very important and likely that your provider (doctor) will use more than one drug to treat TB (tuberculosis). It is very important to finish your whole prescription.
TB Screening
- Around 33% of the world’s population has unused tuberculosis infection (LTBI). For this reason, screening for Mycobacterium tuberculosis (TB) infection is crucial for public health. People with latent tuberculosis infection (LTBI) are at risk for developing active tuberculosis (TB) and becoming infectious.
- The greatest risk for progression occurs during the 1st two years of infection.
- The goal of testing for latent tuberculosis infection (LTBI) is to identify individuals who are at high risk of developing active TB (tuberculosis).
- The decision to test should presuppose a decision to treat if the outcome is positive.
- The tuberculin skin test (TST) and the interferon-gamma release assay (IGRA) are the present methods for screening and are based on the measurement of adaptive host immune response.
BCG Vaccine
- The Bacille Calmette-Guérin (BCG) vaccine has existed for 80 (eighty) years and is one of the most broadly used of all current vaccines, reading >80%of neonates and infants in countries where it is an area of the national childhood immunization program.
- BCG ( Bacille Calmette-Guérin) vaccine has a documented protective result against meningitis and disseminated TB (tuberculosis) in children.
- It does not cure the primary infection and does not cure the reactivation of latent pulmonary infection, the principal source of bacillary spread in the community. The clash of BCG (Bacille Calmette-Guérin) vaccination on transmission of Mtb is therefore limited.
- The CDC and the American Academy of Paediatrics recommend that all children adopted from high (increase)-risk countries who have received the BCG (Bacille Calmette-Guérin) vaccine should act as if they have never received it. All children should be in a skin test (ST) and treated whether it is dormant or active.
- The Mantoux tuberculin skin test (ST) is executed by having 0.1ml of tuberculin purified protein derivative (PPD) injected into the inner layer of the forearm. This will decide if the body’s immune response has been activated by the presence of the bacillus. Upon injection, the skin will increase around 6-10 mm in diameter. 48 to 72 hours after, the person should have their skin test (ST) reaction read. A positive test could reveal a palpable, swollen, hardened, or raised part that should be measured in millimeters. Redness is not measured.
Physical Therapy Management
- All physical therapists (PTs) should be conscious of the proper personal protective equipment (PPE) that should be worn. There is a specialized mask that is shabby that has been sized to specifically fit your face.
- Pulmonary Tuberculosis People with pulmonary TB (tuberculosis) are typically not treated in physical therapy because medications are vital for curing TB (tuberculosis). However, therapists are able to provide percussion and postural drainage (PD) to clear secretions out of the lung.
- Extrapulmonary Tuberculosis Clients with extra-pulmonary TB (tuberculosis) are usually not seen in the physical therapy setting. However, patients may present in the clinic with musculoskeletal problems with unknown causes or arthritic pain. PTs (physical therapists) should be prepared to take a thorough history and a proper examination in order to better identify TB (tuberculosis). A patient could also be seen in physical therapy (PTs) if they have had surgery on their back, in which case normal rehabilitation protocols would be followed.
- It is very main to take a thorough history when TB (tuberculosis) is suspected. It is mainly to ask if the person has traveled outside the country lately, their occupation, or if there is any way they have possibly been exposed to someone who could have TB (tuberculosis). Acknowledge your patient’s signs and symptoms. Palpation of the lymph nodes could also be advisory during an examination.
Differential Diagnosis
- Tuberculosis (TB) is a great mimic and should be considered in the differential diagnosis of several systemic disorders. The following is a non-exhaustive list of conditions to be strongly considered when evaluating the possibility of pulmonary tuberculosis (TB).
- Pneumonia
- Malignancy
- Non-tuberculous mycobacterium
- Fungal infection
- Histoplasmosis
- Sarcoidosis.
Complications/side effects of treatment
Some people have side effects from the drugs used to treat TB (tuberculosis) that may include:
- Skin rashes and other reactions
- Nausea and stomach upset
- Itchy skin
- Yellow skin or eyes (jaundice)
- Dark urine.
- Talk to your provider about any side effects because some might mean that you are experiencing liver damage.
How soon after starting treatment for active TB (tuberculosis) will I feel better?
- It will probably take weeks before you begin having more energy and fewer days with symptoms. However, it will part longer than that to complete your treatment. You will need to take your medications for at least six to nine months.
Can TB (tuberculosis) be cured?
- Yes, TB (tuberculosis) is curable.
What can you do to prevent the spreading of tuberculosis (TB)?
- You usually have to be in contact with someone with active TB (tuberculosis) for a long time before becoming infected.
It assists to follow infection prevention guidelines like:
- Washing your hands thoroughly and sometimes,
- Coughing into your elbow or covering your mouth when you cough (phlegm),
- Avoiding close contact with other people,
- Make sure you part all of your medication correctly,
- Not returning to work or school until you have been cleared by your healthcare provider (doctor).
- In the hospital, the most important measures to stop the spread of TB (tuberculosis) are having proper ventilation and using the correct types of personal protective equipment.
Is there a vaccine to prevent tuberculosis (TB)?
- Some countries (but not the U.S.) use a TB (tuberculosis) vaccine known as Bacillus Calmette-Guerin (BCG). The vaccine is mostly given to children in countries with high rates of TB (tuberculosis) to prevent meningitis and a serious form of TB (tuberculosis) called miliary tuberculosis. The vaccine may make skin tests for TB (tuberculosis) less accurate.
- According to the WHOTrusted Source, people with active TB (tuberculosis) can transfer the bacteria that causes the infection to between 10 and 15 people through close contact per year, if they do not take precautions.
These steps can help prevent the transmission of TB (tuberculosis):
- Get tested if you have a higher risk of TB (tuberculosis) or think you may have been exposed.
- If you test positive for latent or active TB (tuberculosis), take all the medication prescribed.
- If you have been diagnosed with active TB (tuberculosis), avoid crowds and close contact with others until you are no longer contagious.
- Wear a mask if you have active TB (tuberculosis) and have to spend time around others.
- Follow any other instructions provided by your doctor.
What is the outlook (prognosis) for someone with tuberculosis (TB)?
- If you have tuberculosis (TB) and you are treated, your outlook is good if you have followed directions and taken your medications for as long as you should and in the way you were told.
- Treatment for tuberculosis (TB) can be successful, given a person takes all the medication as directed and has access to proper medical care.
- If someone living with TB (tuberculosis) has other diseases, treating active TB (tuberculosis) may be more difficult. HIV, for example, affects the immune system and weakens the body’s ability to fight off TB (tuberculosis) and other infections.
- Other infections, diseases, and health conditions can also complicate a TB (tuberculosis) infection, as can not having adequate access to medical care. Generally, early diagnosis and treatment, involving a full course of antibiotics, offer the best chance of curing TB (tuberculosis).
- The majority of patients with a diagnosis of TB (tuberculosis) have a good outcome. This is important because of effective treatment. Without treatment mortality rate for tuberculosis (TB) is more than 50%.
The following group of patients is more susceptible to worse outcomes or death following TB (tuberculosis) infection:
- Increases in age, elderly, infants, and young children
- Lately in receiving treatment
- Radiologic verification of extensive spread
- Severe respiratory compromise needing mechanical ventilation
- Immunosuppression
- Multi-drug Resistant (MDR) Tuberculosis (TB).
When should I see my healthcare provider (doctor)?
- If you have been exposed to TB (tuberculosis), you should talk to your healthcare provider (doctor) right away. They can assist you to make a decision about getting tested.
- That decision is more important if you have developed any symptoms of illness that could mean you are contagious. Remember, even though tuberculosis can be treated, it can also be fatal if it is not treated.
NOTE
- Tuberculosis (TB) is an infection that is spread through the air. Even though it can be treated, it is still responsible for many deaths around the world. Make sure you contact your healthcare provider (doctor) if you think you have been exposed or have symptoms of TB (tuberculosis).
- Also, make sure to follow instructions if you are treated for TB (tuberculosis). Ask your healthcare provider (doctor) if you have any questions.
FAQs
Tuberculosis (TB) is a disease caused by germs that are spread from person to person through the air. TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, the kidneys, or the spine. A person with TB can die if they do not get treatment.
Tuberculosis (TB) is caused by a bacterium called Mycobacterium tuberculosis. The bacteria usually attack the lungs, but TB bacteria can attack any part of the body such as the kidney, spine, and brain. Not everyone infected with TB bacteria becomes sick.
With treatment, TB can almost always be cured. A course of antibiotics will usually need to be taken for 6 months. Several different antibiotics are used because some forms of TB are resistant to certain antibiotics.
Researchers have found that people who have survived active tuberculosis disease through successful treatment may have a lower life expectancy than people with latent infection, estimating a loss of 3 to 4 years of life.
Groups at High Risk for Developing TB Disease
Children younger than 5 years of age.
People with a history of untreated or inadequately treated TB disease.
TB is spread through the air from one person to another. The TB germs are passed through the air when someone who is sick with TB disease coughs, laughs, sings, or sneezes. If you breathe air that has TB germs, you may get a TB infection. This means you have only dormant (sleeping) TB germs in your body.
What if I have a positive test for TB infection? If you have a positive reaction to the TB blood test or TB skin test, your doctor or nurse will do other tests to see if you have TB disease. These tests usually include a chest x-ray. They may also include a test of the sputum you cough up.




12 Comments