Paraplegia
- Paraplegia is a type of paralysis that harms your ability to move the lower half of your body. It happens when an illness or injury impacts the part of your nervous system which controls the lower half of your body.
- Paraplegia is the symptom of paralysis that mainly harms your legs (though it can sometimes affect your lower body and some of your arm abilities, too).
- This commonly happens because of injuries to your nervous system, especially your spinal cord, yet it can also happen with various medical conditions and diseases.
- About 1 in 50 Americans lives with a certain form of paralysis. Paraplegia is a type of paralysis that harms the lower half of your body and your ability to walk. It is sometimes caused by injury.
- There is no prevention for paraplegia but there are many treatments that can make it easier to manage.
- You might have a problem moving your legs, feet, and stomach muscles. In certain cases, this paraplegia will only affect one leg. This is known as incomplete paraplegia.
Table of Contents
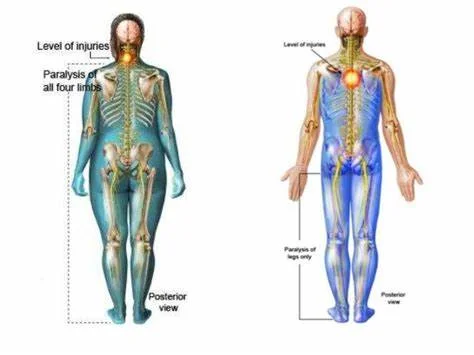
How is it various from other forms of paralysis?
- Various forms of paralysis are named for the areas of the body and how much of the body they impact. Paraplegia only impacts the lower half (1/2) of the body.
Other forms of paralysis involve:
- Monoplegia: This type affects only one limb.
- Paraparesis: This type partially affects both legs.
- Diplegia: This type effect either both arms or both legs.
- Hemiplegia: This type affects one side of the body. For ex., your left arm, and left leg.
- Quadriplegia: This type affects both arms and legs. Quadriplegia is often referred to as tetraplegia.
What is paraplegia?
- Paraplegia is a specific pattern of paralysis (which is when you can not deliberately control or move your muscles) that affects your legs. This occurs because of a difficulty with your nervous system.
- Turn on how it occurs, this paralysis may have different effects on some body systems or processes. Paraplegia is commonly a symptom, but there are rare instances where it is a specific condition on its own.
There are also two important ways that paraplegia can happen, complete and incomplete:
- Complete injury: This means a total loss of function, including the ability to feel sensations and move. Your body also can not control automatic functions that rely on your spinal cord for relaying signals, like controlling your bladder and bowels.
- Incomplete injury: This means a partial decrease in function. You might still be able to feel or move body parts below the injury, yet usually not as strongly as you could before the injury.
There are also two important ways that paralyzed muscles act in paraplegia:
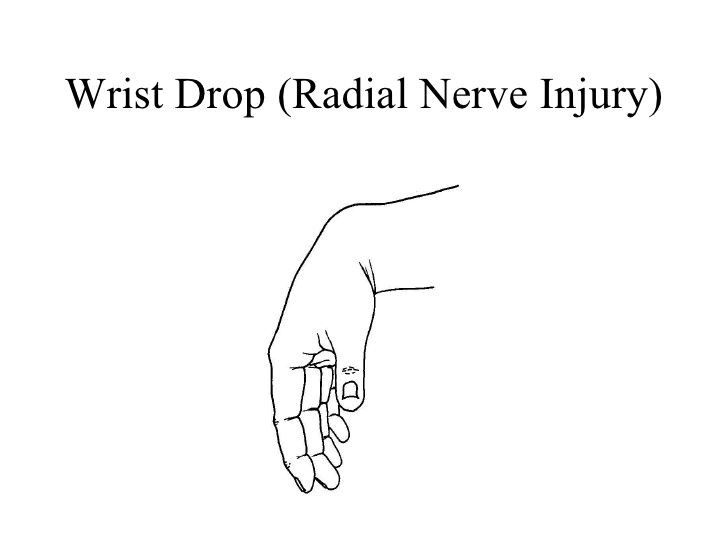
- Flaccid paraplegia: This means that muscles do not work at all and remain flaccid or limp.
- Spastic paraplegia: This is paraplegia that results in muscles that do not work by themselves and contract uncontrollably.
How does the location of a problem harm paraplegia?
- People with paraplegia have various symptoms turn on how high or low the injury is in their spine. Paraplegia generally affects your legs, but may also harm your abdominal muscles, making it difficult to cough. It can also affect your chest muscles, making it various to take deep breaths.
- Your spine has so many sections. Each section has so many vertebrae (singular is vertebra). Your vertebrae are interlocking bone segments that create your backbone and protect your spinal cord.
Paraplegia can occur with injuries in any of the following sections:
- Thoracic spine (T): This part (pronounced “tho-rass-ick”) is in your upper spine. It has 12 (twelve) vertebrae and 12 spinal nerves.
- Lumbar spine (L): This is in your lower spine. It has five (5) vertebrae and five spinal nerves. Your spinal cord ends at the 1st lumbar vertebrae, but several spinal nerves continue downward and exit between the vertebrae below.
- Sacral spine (S): These vertebrae are where your spine and pelvis (hip bones) stick together. There are five (5) sacral vertebrae and nerves.
- Healthcare providers (doctors) use a letter-number combination to discuss sections of the spine and related spinal nerves. For example, T1 is the spinal nerve that runs between the 1st and second thoracic vertebra.
The harms of paraplegia generally are as follows:
- Injury between spinal nerves T1 and T6: This causes full paraplegia. Hips and legs are paralyzed and have no feeling fully, as are the abdominal muscles. This causes a decrease in bladder and bowel control. Injury at this level can cause problems with coughing and deep breathing.
- T7-T12: Complete paraplegia like above, but chest muscles are not affected.
- L1 to L2: Complete paraplegia like above, but chest and abdominal muscles are not affected. You still require a wheelchair for mobility, and you may not have bowel and bladder control.
- L3 to S5: Incomplete paraplegia becomes more common the farther down the spine an injury happens. You can usually walk with or without braces or a walker at this level. However, bowel movements and bladder function may be harmed.
Peripheral nerve problems
- Paraplegia can occur with problems of your peripheral nerves, which are the nerves that extend outside of your spinal cord. These commonly happen because of diseases and conditions that affect multiple nerves at the same time (polyneuropathies), such as Guillain-Barré syndrome or diabetes-related nerve damage (neuropathy).
What are the most common causes of paraplegia?
- The most usual cause of paraplegia is an injury to your spinal cord. Those injuries can occur in many different ways.
The most usual reasons are:
- Motor vehicle crashes,
- Penetrating injuries (especially from gunshot or stab injuries),
- Falls (especially in older adults with bone density-related conditions such as osteoporosis or osteopenia).
Other common causes of paraplegia involve:
- Spine tumors, involving cancers. This can include cancer that develops on or around your spinal cord, or that begins elsewhere in your body and spreads to your spine,
- Cysts or fluid-filled cavities within your spinal cord (SC) (syringomyelia)
- Infections that attack or compress your spinal cord (SC)
- Less blood flow (ischemia) due to a blocked blood vessel or blood vessel rupture.
- Diabetes-related nerve damage.
What are the symptoms of paraplegia?
- The symptoms of paraplegia can turn on the person and on the severity of your paraplegia. Certain symptoms will be present right away and others might develop over time.
Symptoms involve:
- lack of feeling in the lower half (1/2) of your body
- chronic pain
- phantom pain in the lower half (1/2) of your body
- bladder and bowel trouble
- difficulty walking and standing
- weight gain,
- depression
- sexual difficulties
- skin breakdowns
- infections
- high blood pressure.
How is paraplegia diagnosed?
- A medical provider (doctor) can assess you for paraplegia if you are having symptoms. They will take a detailed medical history that will include any recent accidents or illnesses.
- You will generally need medical imaging tests to look for damage that might be causing your symptoms. Imaging tests involve an MRI, X-ray, or CT scan. You might also have a test known as electromyography. This test measures how your body responds when harmed muscles are stimulated.
How is paraplegia treated?
- The treatments for paraplegia depend on what caused the issue and where it is in your spinal cord (SC). The injuries and conditions that can cause paraplegia can differ widely, and the potential to recover from them can also be difficult. Because of that, a healthcare provider (doctor) is the best person to explain the situation.
- They will offer you guidance for your specific situation, involving the possible treatments and the side effects or complications that can occur with those treatments.
I. General Management:
- Frequent changes in the patient’s posture to guard against bedsores.
- Care of the skin by certain washing with alcohol followed by talc powder. In case of urinary incontinence, certain changes of bed sheets.
- Care of the bladder: If there is confinement, use parasympathomimetic drugs. If this fails, use a catheter to assess the bladder.
II. Physical Therapy Management
- From the very start, all efforts should be concentrated on the rehabilitation of the patient. An accurate assessment of the patient is required so as to be able to institute the appropriate treatment plan.
- The physiotherapy management of the patient starts from the day patient is admitted to the hospital.
The treatment can be discussed under the Acute stage and the Chronic stage:
A. ACUTE STAGE MANAGEMENT:
The aims of treatment involve:
- avoiding chest complications
- further injury to the spine
- pressure sores
- maintaining range of movement
Goal setting:- Realistic goals should be agreed upon with the patient and the relatives and the therapist (PT) – compromises should be agreed upon.
Chest Physiotherapy:- Will mainly be prophylactic at this stage and depends on the level of injury. If prophylactic includes deep breathing exercises to maintain tidal volume and avoid atelectasis. The greater the level of injury the greater the risk of chest infections due to reduced chest mobility. Reduced vital capacity can conduct to atelectasis and infections. This can be cured by teaching the patient deep breathing exercises, assisted coughing and huffing, and doing percussions to mobilize secretions. If on a ventilator, suctioning together (join) with vibrations and percussions can be done.
Proper turning to patients:- will help prevent further spinal cord damage together with the prevention of pressure sores.
Proper positioning:- is essential to prevent further patient injury, cure spinal deformities, prevent pressure sores, and prevent contractures.
Active assisted exercises:- to facilitate recovery of harmed muscle groups and also to maintain range of movement in the partially involved muscles. To maintain and increase muscle strength in the part included muscle groups.
Passive movements:- to cure contractures and should be assisted where applicable.
Precautions with passive movements:-
- avoid the extreme range of movement – the joints are paretic
- hip flexion to be done with knee flexion – avoid lumbar or lower thoracic movement if the lesion is low.
- Avoid straight leg raising – stretches harmed neural tissue.
- Do not give combined wrist and finger flexion – injury to the extensor tendons.
- Counseling and psychological support:- can be given to the patient with very much input from the psychologist and or the social worker. Relatives should be involved as well.
B. SUBACUTE TO CHRONIC STAGE PHYSIOTHERAPY MANAGEMENT:
Bed mobility:- This includes teaching the patient how to roll, come from lying to sitting and vice-versa, bridge, and relieve pressure when in bed
Outside bed mobility:- Involves teaching the patient sitting balance, standing and standing balance, and walking where applicable.
Wheelchair use and selection:- Is done with the assistance of the Occupational therapist – involves teaching the patient transfers from the wheelchair to bed, toilet seat, car, bathroom, and also to floor. Wheelchair maneuvering is also taught for e.g. ramps and curbs. The Occupational Therapist also teaches a lot of ADLs with the patient in a wheelchair in preparation for discharge. Pressure care is also involved.
Continue with Chest physiotherapy as in the acute stage.
Aid selection and use training:- If they are low-level paraplegics and will be able to walk with the use of calipers or orthosis, they will be helped with the selection and training on the use of the aid. Backslabs/calipers can also be used to help with walking and standing.
Standing:- can be done using a tilt-table at first and then move to backslaps and other devices.
Muscle strengthening:- As is appropriate – to try and compensate for the harmed muscle groups and to strengthen those with partial innervation.
Sexual education:- Emphasis should be on the utilization of the areas still with sensation to get sexual gratification. The clinician can also suggest the use of other assistive devices e.g. sex toys
Social services;- Will be needed to help with the processing of pension etc. and social support to the patient and family. Psychological support from the Psychologist will be required throughout the rehabilitation process until the pt and relatives have accepted the disability.
Vocational training and job placement:- Can be done with the assistance of Physios, OTs, and the Social Worker.
Follow-up – at home or during workshops to continue with support and address any difficulties that may arise.
GAIT RE-EDUCATION AND SPINAL CORD INJURY:-
- T1 –T8 – swing to calipers with the rollator. Can try crutches if spasticity is not a big problem.
- T8 – T10- swing to and swing through gait with full calipers and crutches. Walking is not functional.
- T10- L2- swing through and 4-point gait with calipers and crutches. Requires wheelchair for part of the day. Walking can be functional.
- L2 –L4- under knee calipers with crutches or sticks. A wheelchair is not required.
- L4 – L5 may or may not need calipers. A wheelchair is not required. May need a stick or other walking aid.
A balanced exercise program includes 3 types of exercise:
(1) Stretching/Flexibility Exercises:
- slow, sustained lengthening of the muscle.
- Stretching is the most main exercise you can do.
- Stretching increases flexibility – the ability to move the parts of your body through their full range of motion.
- Stretching also can decrease muscle spasticity and cramps and may also reduce problems such as tendonitis and bursitis.
- To be effective, stretching routines must be done regularly, commonly once or twice a day.
- Stretch as far as you can and hold the stretch for ten seconds and then ease back.
- Each stretch should be performed slowly, with no unexpected jerking or bouncing.
- Stretching also should be done before and later other exercises to prevent muscle strain and soreness and to help avoid injuries.
(2) Aerobic Exercises:
- Steady exercise using big muscle groups.
- Aerobic exercise strengthens your heart and lungs and increases your body’s ability to use oxygen. It also reduces fatigue, increases energy levels, and assists you sleep better, control your weight, and lift your spirits.
- It is commonly recommended to gradually work up to three or four sessions per week, each lasting 15 to 60 minutes. Include a five-minute warm-up (including stretching) before the activity and 5 to 10 minutes of a cool down (stretching and slower activity) afterward.
- Walking, stationary bicycling, water exercises and chair exercises are excellent so many choices.
- Walking: Experts recommend walking to maintain your ability, comfort, and safety. Even short, slow walks can provide benefits. Aquatic (water) exercises: Aquatic exercises and swimming supply optimal exercise conditions. Water eliminates the harms of gravity, allowing weakened limbs to attain a greater range of motion. Water also assists support the body so there is less stress on the hips, knees, and spine.
- Exercise in the water: This can help increase muscle power and endurance and help mobilize joints and muscles. They also assist to relax muscles and improve coordination. Warm water (between 83 and 90 degrees F) can be especially best for stiff, sore joints. Exercises can be done while standing in shoulder-height water or while sitting in deep water. In shallower water, an inflatable tube, floatation vest, or belt can be used for flotation.
- Stationary bicycling: Stationary bicycling is a great way to increase fitness without putting stress on hips, knees, and feet. It can be done in any weather, and balance is commonly not an issue. Add resistance only as you are comfortable and only later warming up.
- Chair exercises: If mobility and balance are major issues, consider chair exercises. They can supply a great workout and easily incorporate strengthening and stretching exercises.
(3) Strengthening Exercises:
- Repeated muscle contractions till the muscle becomes tired.
- Strengthening exercises assist increase muscle tone and improving the quality of muscles. This enhances mobility and supplies energy and a positive sense of well-being.
- Strong hip and leg muscles are required to lift the legs to walk, and strong arm muscles are needed to carry out daily functions. Strong abdominal and back muscles assist maintain correct posture and can counter pain resulting from poor gait, poor posture, or the use of mobility aids.
Physical agents:
- Thermotherapy is used to decrease pain and spasticity. They are (i) Superficial heat: IRR, wax bath, etc. (ii) Deep heat: SWD, MWD, etc.
- Electrical therapy: is used to increase muscle power and decrease pain. e.g, TENS, EST, IFT.
Therapeutic exercises:
- Mat exercise
- Proprioceptive Neuromuscular Facilitation (PNF) exercise
- Active and passive ROM exercise
- Strengthening exercise
- Stretching exercise
- Endurance exercise
- Co-ordination exercise
- Pelvic tilting exercise
- Hamstring muscle stretching
- Spinal rotation
- Calf muscle stretching
- Neck raising exercise
- Knee rolling exercise
- Lying in extension
- Extension exercise
- Back and gluteal exercise.
III. Symptomatic Treatment:
- Analgesics and sedatives for pain.
- Muscle relaxants for the spasticity.
- Vitamins and tonics.
IV. Orthosis:
- Various orthoses are used to help patients with paraplegia.
- These are a crutch, walker, cane, lumbosacral brace, and wheelchair.
V. Gait training:
- It is an important part of the rehabilitation program balance can be achieved through proper gait training. Gait training can be done by following methods:
- Pre-ambulation MAT program:
- Rolling, prone on the elbow, prone on hand, quadruped, pelvic tilting, setting, and standing balance.
- Parallel bar progression
- Advanced parallel bar activities.
- Assistive device: Ex. Cane, crutches, walker
What can I do at home to handle paraplegia?
- Paraplegia is a key symptom of a spinal cord injury or a condition that harms your nervous system. These injuries and conditions are almost every times medical emergency.
- The only exceptions to this are when a healthcare provider (doctor) diagnoses you with a medical condition that can conduct to paraplegia. In those cases, a healthcare provider (doctor) will provide guidance on what to do if and when paraplegia develops.
- The patient is advised to use the lumbosacral orthosis to support the back during traveling.
- The patient is advised to hot fomentation at home.
- The patient is advised to lie in the prone position for at least 15 minutes duration twice a day.
- The patient is explained about the proper sitting, standing, lying and lying to standing, and doing the household activity in a proper way.
- the patient is advised to take rest and to avoid forward bending as much as the patient can avoid.
- Home adjustments:-usually done with the help of Occupational Therapists. A home assessment will have to be done and advice on the necessary changes and adjustments to be undertaken given before the patient is discharged from the hospital.
IMPORTANT: If you are with someone who has an injury that could affect their spine, it is very important to avoid doing anything that could make the injury worse.
- Moving someone with a possible spinal cord injury (SCI) in the wrong way can cause permanent damage. Because of this, only trained professionals should move someone with a suspected spinal cord injury (SCI). The ONLY exception to this is if the person is in immediate danger if you do not move them (such as from a motor vehicle crash where the vehicle the person is in may catch fire).
How can paraplegia be prevented?
- Paraplegia is sometimes preventable, yet it also happens unpredictably, and in ways, you can not prevent it. The best things you can do to cure paraplegia or decrease your risk of developing it are:
- Wear safety equipment, involving safety restraints (like seat belts) as recommended. Seat belts and other restraints can assist avoid injuries that could lead to paraplegia.
- Be attentive when using firearms. Gunshot wounds are one of the most usual causes of spinal cord injuries (SCIs) that lead to paraplegia. You should always treat firearms with the greatest caution, no matter the circumstance. Act as if they are loaded even if you are absolutely certain they are not. You should store firearms unloaded, secured with a trigger lock, and out of reach of children. It is wise to store ammunition separately under lock and key.
- Take cues to avoid falls. Use safety equipment, especially safety harnesses, when working on a roof or other elevated environments. You should also give steps to avoid falls in the home, especially with stairs or in bathrooms. This can involve installing handrails, using non-slip footwear and floor surfaces, and keeping stairs clear of tripping hazards.
- Miss misusing prescription medications, recreational drugs, and alcohol. These can harm your immune system’s ability to fight infection. They can also improve your risk of injury from falls, car crashes, etc.
- Unfortunately, most cases of paraplegia are caused by accidents and conditions that are not preventable.
- You can take steps to decrease your risk of accidents, such as practicing safe driving. However, there is no way to cure all accidents and completely prevent any chance of paraplegia.
What are the common risk factors for developing paraplegia?
- There are certain risk factors for developing paraplegia.
These involve:
- playing high-effect sports such as football or wrestling,
- participating in sports such as gymnastics, diving, or surfing,
- a history of cancer (Ca),
- a family history of a condition that harms your nervous system,
- Detecting care for paraplegia.
If you or a loved one have paraplegia, these organizations can assist find the care and support you need:
- This foundation has support to assist find physicians, rehabilitation facilities, therapists, and more.
- The United Spinal Association: This association can join you with support groups, accessibility resources, and more.
- This organization can assist you to find medical care, financial assistance, disability advocacy, assistive technology, and more.
When should paraplegia be treated by a doctor or healthcare provider (doctor)?
- A healthcare provider (doctor) should always examine and treat paraplegia.
What is the difference between paraplegia and tetraplegia?
- Paraplegia is paralysis that harms your legs. Tetraplegia — also known as quadriplegia — is paralysis that harms your arms and legs.
What is the difference between paraplegia and hemiplegia?
- Paraplegia and hemiplegia have a certain similarity, but they commonly happen in very different ways and for different reasons.
- Paraplegia: This is paralysis that harms your legs and sometimes the lower half of your body.
- Hemiplegia: This is paralysis that harms one side of your body, either left or right. It can include your arm, leg or one side of your face, or a combination of these three.
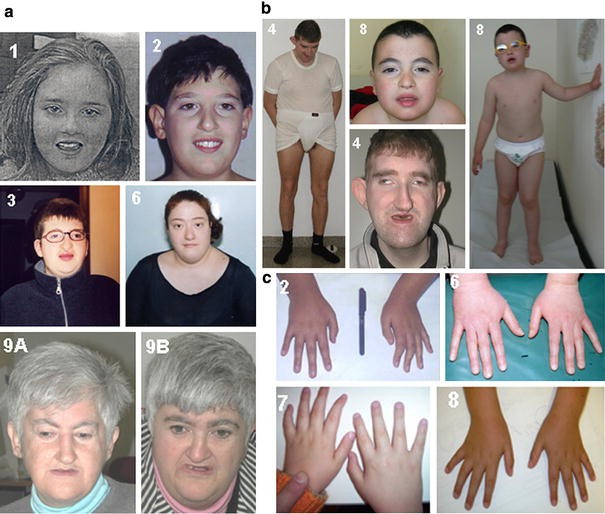
What is hereditary spastic paraplegia?
- This condition mansions to a group of disorders inherited from one or both parents. These disorders disturb your nervous system, causing paralysis in your legs.
- Paralysis includes constant muscle movements that a person can not control (which is why the word “spastic” is part of the name). This condition can occur on its own, or it can happen along with other medical conditions. It is also progressive, meaning it gets worse over time.
What is the outlook for people with paraplegia?
- Paraplegia is a lifelong condition that can conduct to other issues with time.
This might include:
- overactive muscle responses are known as spasticity,
- the trouble with digestion,
- constipation or loss of bowels,
- incontinence,
- muscle weakness,
- infections.
- Over time, paraplegia can conduct in a decline in a person’s function and independence as symptoms become worse. Your medical team will assist you to reduce these possible complications. If they do develop, you might require additional medications or treatments.
NOTE
- Paraplegia is paralysis that harms your legs, but not your arms. This symptom is most likely to occur with injuries, but can also happen because of diseases or medical conditions.
- The paraplegia that happens with injuries is a medical emergency and needs immediate medical care. Preventing further injury is serious to reducing the risk of permanent paralysis.
- While paraplegia can be frightening, there are also many options to assist people to recover from or adapt to it. Even when paraplegia occurs because of permanent damage, it is possible to adapt and find ways to live independently and have a fulfilling and enjoyable life.
- Paraplegia is a type of paralysis that harms the lower half of your body. It harms your ability to walk, stand, and do other actions that require control of your legs, feet, pelvic muscles, and stomach.
- Paraplegia is commonly the result of an injury, but it can also be caused by conditions that damage your spinal cord or brain. There is no cure for paraplegia, yet treatment can help you manage your condition.
FAQs
Paraplegia is a spinal cord injury that paralyzes the lower limbs. It is a result of severe damage to the spinal cord and the nervous system. Paraplegia mainly affects the trunk, legs, and pelvic region, resulting in loss of movement.
Paraplegia is a type of paralysis that affects the lower half of your body and your ability to walk. It is often caused by injury. There is no cure for paraplegia but there are many treatments that can make it easier to manage.
Paraplegia is a type of paralysis that affects your ability to move the lower half of your body.
When paraplegia strikes, the brain or spinal cord is unable to send or receive signals to the lower half of the body. Due to this, paraplegics cannot move their body parts below the waist and lose sensation in that area too. At times there is a tingling feeling too in the legs and feet.
The major difference between paraplegia and quadriplegia is that: Paraplegia is a paralysis of the legs. Quadriplegia is the paralysis of the legs and arms. Both conditions are typically the result of injuries or diseases affecting the brain and spinal cord.
Physical therapy can prove to be an excellent tool for helping paraplegics improve their health and even help alleviate some paraplegia symptoms.




2 Comments