PES ANSERINUS BURSITIS AND TENDINITIS
DEFINATION OF PES ANSERINE BURSITIS :
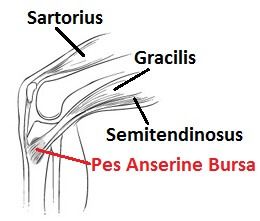
- Pes Anserine bursitis, also known as intertendinous bursa, is an inflammatory condition of bursa of the conjoined insertion of the sartorius, gracilis and semitendinosus.
- We can locate this at the proximal medial aspect of the Knee, two inches below the medial knee joint line between the pes anserinus tendons.
Table of Contents
Clinically Relevant Anatomy Related to Pes Anserine Bursitis
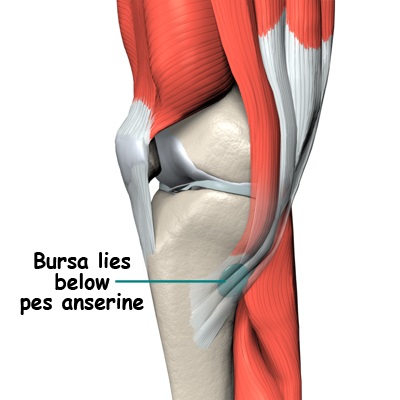
- The Pes Anserine bursa is a fluid filled vesicle. It secretes synovial fluid in order to reduce friction between tissues, and also works as a cushion for bones, tendons, and muscles. The inflammation of the bursa does not appear suddenly, but rather progresses over a period of time. Bursitis can also occur in the shoulder, knee, hip, elbow, and big toe.
- The Pes Anserine, also called the ‘Goose Foot’ is the insertion of the sartorius, gracilis, and semitendinosus muscles, which are conjoined proximally on the medial side of the Tibia.
- The three tendons of the Pes Anserine are located superficial to the medial collateral ligament (MCL) of the knee. The sartorius and gracilis muscles are adductors of the leg (i.e. they pull the leg towards the median axis of the body). The semitendinosus muscle is part of the hamstrings muscle group located at the back of your upper leg. Together, these three muscles are primarily flexors of the knee and internal rotators.
Which are common causes of Pes Anserine Bursitis?
- Pes Anserine bursitis often occurs when the related muscles are repeatedly used, by doing movements such as flexion and adduction. This causes friction and also increases pressure on the bursa.
- Bursitis can also be due to a trauma, such as a direct hit in the Pes Anserine region.
- A contusion to this area results in an increased release of synovial fluid in the lining of the bursa. The bursa then becomes inflamed and tendered or painful and underlying Osteoarthritis of the knee.
- Reports suggest that anserine bursitis is more common in overweight middle-aged females. We can explain this by the fact that women have a wider pelvis, resulting in angulation of the knee in the frontal plane, which leads to more pressure in the area of insertion of the pes anserinus by genu valgum.
- We can say that an inflamed bursa is not a primary pathology, but rather a consequence of an earlier complication. Underlying knee pathology (e.g. OA)
- Activities/sports which involve repetitive use of the sartorius, semitendinosus, and gracilis tendons such as: running, dancing, and sports that require a lot of direction changes (e.g. soccer, basketball)
- Abnormal hip, knee, or ankle biomechanics
- Inadequate warm-up and stretching prior to and following exercise
- Muscle imbalances
- Inappropriate footwear
- A sudden increase in activity level/sports training
Which Are Signs/Symptoms in Pes Anserine Bursitis?
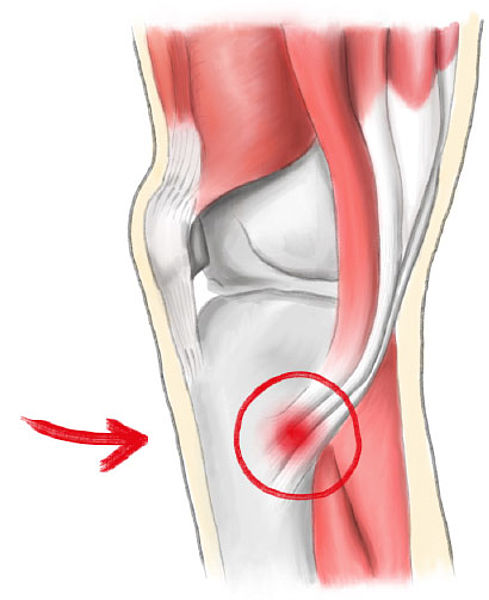
- Pes Anserine bursitis causes pain on the inside of the knee (mostly during running or taking stairs).
- The patient may experience spontaneous anteromedial knee pain on climbing or descending stairs and tenderness at the PA. As well, the region around the bursa will be swollen or tender to the touch.
- Weakness or feeling of giving way around the knee
- Swelling over the inside aspect of the knee
Other clinical presentations may include:
1) Decreased muscle strength
2) Gait deviations
3) Decreased function
4) Decreased range of motion (ROM)
- Postural dysfunction/impaired lower extremity biomechanics
- Aggravating factors include activities that require movements like flexion and endorotation, as well as exorotation and adduction.
- Pivoting, kicking, squatting or quick movements from side to side, such as in the sports mentioned above, may also cause further irritation.
Differential Diagnosis
Pes Anserine bursitis is often confused with other causes of medial knee pain.
- Stress-fracture of the shinbone on the proximedial side will cause pain in the area of the Pes Anserine.
- Patello-femoral syndrome
- Medial meniscus lesion and osteoarthritis: Pain and sensitivity would be present in the medial compartment, while in the pes anserinus bursitis they are located inferomedial to the medial joint interline. Stress maneuvers of the medial collateral ligament, with or without
instability, may contribute to the diagnosis of lesions of the medial collateral ligament. - Knee pain secondary to L3-L4 radiculopathy is associated with lumbar pain without pain on digital pressure of the anserine region.
- Panniculition: occurs in obese individuals, and causes painful inflammation of subcutaneous fat at night.
- Semimembranosus tendinitis will often occur as a running injury.
- Medial Plica Syndrome can cause pain and tenderness on the medial side of the knee.
- Extra-articular cystic lesions: synovial cyst, ganglionic cyst, parameniscal cyst, pigmented villonodular synovitis, synovial sarcoma.
- In addition to the conditions listed above, other problems to be considered include the following
- Atypical medial meniscal cysts
- Juxta-articular bone cysts
- Semimembranosus bursitis
- Tibial collateral ligament bursitis
Diagnostic Procedures:

Lateral x-ray views of the patient’s knee are very useful for ruling out a stress fracture, arthritis, or even Osteochondritis Dissecans.
An MRI is needed to clarify damage caused to other regions of the medial side of the knee. An MRI could prevent unnecessary arthroscopy. MRI findings should be compared with those of a physical examination. Sinography (radiography of a sinus following the injection of a radiopaque medium) is the best method for establishing the diagnosis when other imaging modalities, including MRI and CT, are not feasible.
Examination
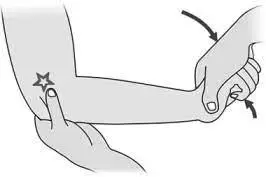
The pes anserine bursa can be palpated at a point slightly distal to the tibial tubercle and about 3-4 cm medial to it (about 2 fingerbreadths)
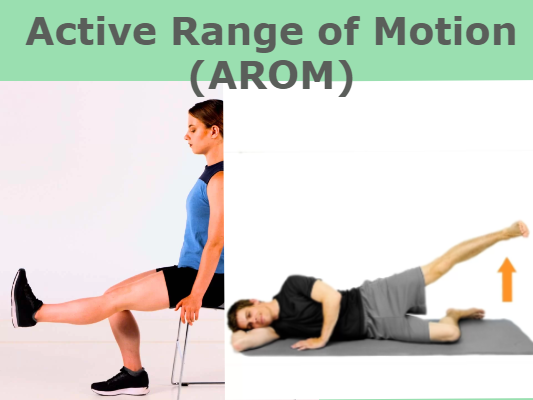
Examine hamstring length with the patient in the supine position. Bend the patient’s hip 90° and then extend the knee as far as possible. How far the knee can be extended will indicate hamstring length and tightness. If the patient’s knee can be straightened completely then the hamstrings are not tight.
With the sports-related variant of pes anserine bursitis, symptoms may be reproduced by means of resisted internal rotation and resisted flexion of the knee. With the chronic variant in older adults, flexion or extension of the knee usually does not elicit pain
Treatment
Medical Management
The initial treatment of pes anserinus bursitis should include the relative rest of the affected knee. To temper the pain caused by the bursitis, the most important thing of all is rest. Avoid stairs, climbing, or other irritating activities to quiet down the bursa and the related pain
Nonsteroidal anti-inflammatory drugs (NSAID) can be taken to alleviate the pain.
Additional modalities, including local injection of a corticoid such as methylprednisolone, are indicated in some cases.
An elastic bandage can be wrapped around the knee to reduce any swelling or to prevent swelling from occurring Intrabursal injection of local anesthetics, corticosteroids, or both constitutes a second line of treatment.
Surgical treatment is indicated in cases with failure to conservative treatments.
Simple incision and drainage of the distended bursa can improve symptoms in some reported cases.
The bursa may be removed if chronic infection cannot be cleared up with antibiotics. After surgery, if the bursa is removed, follow the same steps of rehabilitation and recovery outlined under physiotherapy management.
If the bursitis becomes infected and standard antibiotic treatments are ineffective, A surgical decompression of the bursa may be a solution in this case.
Physiotherapy Treatment in Pes Anserine Bursitis :

Restrict movement and alternately apply ice during the inflammatory phase. An ice massage of 15 minutes every 4-7 hours will reduce the inflammation. Be careful not to increase friction. Teach the patient muscle-conditioning exercises.
Many patients with pes anserinus bursitis and tendinopathy start to feel better within a few weeks of the injury. Your physiotherapy treatment will aim to:
- Reduce pain and inflammation.
- Normalize joint range of motion.
- Stretch tight muscles around the knee
- Strengthen your knee: especially quadriceps (esp VMO) and hamstrings.
- Strengthen your lower limb: calves, hip, and pelvis muscles.
- Improve patello-femoral (knee-cap) alignment
- Normalize your muscle lengths
- Improve your proprioception, agility, and balance
- Improve your technique and function eg. walking, running, squatting, hopping, and landing.
- Minimize your chance of re-injury.
However, we strongly suggest that you discuss your knee injury after a thorough examination from a knee injury clinician such as a sports physiotherapist, sports physician, or knee surgeon.
The closed-kinetic chain exercises are also a recommended method to prevent the development of collateral knee instability, which occurs to be a risk factor for Pes Anserine bursitis.
The majority of people with pes anserinus bursitis and tendinopathy will make a full recovery with conservative physiotherapy treatment.

Kinesio-Taping Also Helps to Reduce Pain,Swelling and knee joint mobility.
An injection into the site of inflammation is sometimes also required to decrease pain and inflammation.
How to Prevent Pes Anserinus Bursitis/Tendinopathy?
There are a variety of ways to reduce your risk of developing pes anserinus bursitis/tendinopathy. These include:
- Correction of exercise technique
- Adequate warm-up and cool-down before and after exercise
- Correction of muscle imbalances
- Appropriate footwear during exercise
- Gradual increase in training intensity/quantity





3 Comments