Periodontal Abscess
Table of Contents
What is a Periodontal Abscess?
- A periodontal abscess is defined as a localized buildup of pus within a periodontal pocket’s gingival wall. It is more common in people who have previously had periodontal pockets and grows quickly, damaging periodontal tissues and displaying obvious signs.
- A periodontal abscess is an infected pocket that grows in your gums. Periodontal abscesses can occur in anyone, but they are more common in persons who have poor oral hygiene. Without treatment, a periodontal abscess infection can spread to other parts of your mouth and body, causing difficulties.
- A periodontal abscess (also known as a lateral abscess or a parietal abscess) is a localized collection of pus (i.e. an abscess) within the periodontal tissues. It is a form of abscess in the mouth. A periodontal abscess develops alongside a tooth, as opposed to the more typical periapical abscess, which is caused by the spread of infection from a dead tooth (i.e. one that has experienced pulpal necrosis). To represent this, the phrase “lateral (periodontal) abscess” is sometimes used. Periodontal abscesses, as opposed to periapical abscesses, are frequently connected with a live (living) tooth. Periodontal abscesses are acute bacterial infections that are categorized mostly by site.
- A periodontal abscess appears on your gums as a boil or pimple. It’s usually darker than the rest of your gums and swollen. Swelling can range from minor to severe.
Symptoms And Causes of Periodontal Abscess
What signs and symptoms indicate a gum abscess?
- A swelling bump on your gums is the most visible symptom. Many people feel pain or soreness, whereas others do not.
- Other symptoms of a periodontal abscess include:
- Toothache
- Sensitivity of the teeth to hot and cold food and drinks
Bad breath (halitosis) - Bad taste
- Lymph nodes in your neck or jaw become swollen
- Pain while chewing
- Infection (pus)
- Fever
- Loose tooth
- The major symptom is discomfort, which often arises unexpectedly and is exacerbated by chewing on the affected tooth, which may seem elevated and prominent in the bite. The tooth may be movable, and the lesion may contribute to periodontal ligament and alveolar bone deterioration. The pain is intense and throbbing. An early periodontal abscess’s oral mucosa appears erythematous (red), swollen, and unpleasant to touch. Because of the straining of the mucosa above the abscess, the surface may be glossy. The lesion will not fluctuate before pus forms, and there will be no purulent discharge. Regional lymphadenitis is possible.
- When pus forms, the pressure builds up along with the pain until it spontaneously discharges and relieves the agony. When pus leaks into the mouth, it leaves a terrible taste and smell. If the infection does not drain via the periodontal pocket, it might spread as cellulitis or a purulent odontogenic infection. The path of dissemination is determined by local anatomic features (see fascial spaces of the head and neck). There may be systemic disruption, accompanied by the development of discomfort and fever.
What is the cause of a gum abscess?
- When bacteria from your mouth infiltrate the space between your teeth and gums, a periodontal abscess occurs. Gum disease is the most common cause of this, and it is the leading risk factor for periodontal abscesses.
- If you have any of the following conditions, you are more prone to develop a gum abscess:
- Bruxism (chronic teeth grinding and clenching)
- Teeth damaged by injury or trauma
- Restorations that are broken or damaged, such as dental fillings, crowns, or bridges
Risk factors:
What are the danger signs of a gum abscess?
- Periodontal abscess risk factors include:
- Poor oral hygiene. This is the most dangerous risk factor. If you do not remove plaque and tartar from your teeth on a regular basis, your gums will become red and swollen. These symptoms are early warning signs of gum disease. Gum disease, if left untreated, can lead to dental abscesses and bone loss.
- A high-sugar diet. Sugary foods and drinks raise your risk of cavities and gum disease.
Complications:
What are the side effects of a periodontal abscess?
- A gum abscess, if left untreated, can lead to a variety of oral health problems, including:
- Damage to the ligaments and soft tissues surrounding your teeth
- Bone loss in your jaw
- Tooth loss
- According to research, bacteria from your mouth can spread to other parts of your body. Periodontal abscesses are sometimes connected with:
- Sepsis (blood infection)
- Heart inflammation
- Pneumonia
- Brain abscess
- If you suspect you have a gum abscess, contact your dentist straight away. The importance of prompt treatment in avoiding complications cannot be overstated.
Diagnosis And Test:
What are the symptoms of a periodontal abscess?
- A gum abscess is diagnosed by a dentist by:
- Examining your symptoms. Your dentist will inquire about your symptoms, such as the length of time the abscess has been present.
- I’m performing a periodontal exam. They will take measurements of the pockets around the damaged tooth. This tells them whether or whether you’ve lost any bone in the area, and how much.
Having dental X-rays taken. X-rays of the affected tooth will be taken by your dentist. This demonstrates the severity of the abscess and the extent of the infection.
Classification:
Periodontal tissues can be involved in four types of abscesses:
Gingival abscess – A purulent infection that affects only the soft gum tissue around the marginal gingiva or the interdental papilla.
Periodontal abscess – A localized, purulent infection of the gum tissue that extends apically and next to a periodontal pocket.
Pericoronal abscess – A purulent infection within the gum tissue surrounding the crown of a partially or completely erupted tooth. Acute pericoronitis usually occurs around a partially erupted and impacted mandibular third molar (lower wisdom tooth).
Combined periodontal/endodontic abscess
Treatment of Periodontal Abscess
What is the treatment for a periodontal abscess?
- A periodontal abscess is a dental emergency that must be treated right away. Treatments for periodontal abscess include:
- Drainage of a periodontal abscess. The abscess may need to be drained by your dentist. They will make a small incision (cut) in your gums and then use pressure to drain the infection.
Treatment for gum disease. Your dentist may propose scaling and root planing (deep tooth cleaning) or gum surgery to treat the infection.
Antibiotics. Your dentist may prescribe antibiotics in addition to treating the infected region to lessen your chance of re-infection.
Root canal therapy. If a periodontal abscess extends to a tooth and infects it, root canal therapy may be required to save the tooth. - Extraction of teeth. In severe circumstances, your dentist may advise you to have an infected tooth extracted. If you need a tooth extracted, your dentist will discuss replacement choices with you.
A periodontal abscess cannot be treated at home. Call a dentist straight away if you suspect you have a gum abscess. - A key consideration is whether the problematic tooth should be removed or kept. Although the pulp is usually still viable, a history of recurrent periodontal abscesses and considerably weakened periodontal support indicate that the tooth has a bad prognosis and should be extracted.
- The first step in treating a periodontal abscess is to relieve discomfort and control the infection. The pus must be evacuated, which aids in both of these goals. If the tooth is extracted, drainage will occur through the socket. If pus is already draining from the periodontal pocket, it can be stimulated by moderate irrigation and scaling of the pocket while massaging the soft tissues. If this does not work, incision and drainage, as detailed in Dental abscess#Treatment, are required.
- Antibiotics are secondary to drainage, which, if successful, eliminates the need for antibiotics. Antibiotics are often reserved for serious illnesses characterized by face edema, systemic discomfort, and fever. Because anaerobic bacteria are frequently involved in periodontal abscesses, oral antibiotics such as amoxicillin, clindamycin (in penicillin allergy or pregnancy), and/or metronidazole are given (although metronidazole should be used in conjunction with penicillin due to its lack of aerobic gram-positive coverage). The results of microbiological culture and sensitivity testing of a sample of pus aspirated at the start of any treatment, ideally, dictate the choice of antibiotic, but this rarely occurs outside of the hospital setting.
- Other measures taken during the acute phase may include using a dental drill to reduce the height of the tooth so that it no longer contacts the opposing tooth when biting down, and using hot salt water mouthwashes (antiseptic) on a regular basis to encourage further drainage of the infection.
- Following the acute phase, care includes eliminating any leftover infection and treating the causes that contribute to the formation of the periodontal abscess. Typically, this will include periodontal disease therapy, such as oral hygiene training and periodontal scaling.
Prevention:
How can I reduce my chances of developing periodontal abscesses?
- The greatest strategy to lower the risk of a periodontal abscess is to practice good dental hygiene:
- Brush your teeth two times a day, at minimum.
- Take a toothbrush with soft bristles and toothpaste with fluoride for cleaning your teeth.
- At least once a day, floss in between your teeth.
- Constantly visit your dentist for checkups and cleanings.
- If you suffer from dry mouth, consult your dentist about treatment options.
- Consult your dentist about a mouth guard if you grind or clench your teeth.
Prognosis
- Will a periodontal abscess heal on its own?
A periodontal abscess will not resolve on its own. It necessitates medical attention. - What is the severity of a periodontal abscess?
Most periodontal abscesses are not fatal. However, because the illness might spread, it is critical to treat it as soon as possible. Though uncommon, an untreated periodontal abscess can lead to sepsis and other potentially fatal complications.
Having to deal with:
- When should I arrange an appointment with my doctor?
- Schedule an appointment with a healthcare provider if you have a swelling, painful bump on your gums. They can confirm your diagnosis and make therapy recommendations.
- When should I go to the hospital?
- If you experience any of the following symptoms, dial 911 or go to the nearest emergency room:
- Fever
- Chills
- Nausea and vomiting
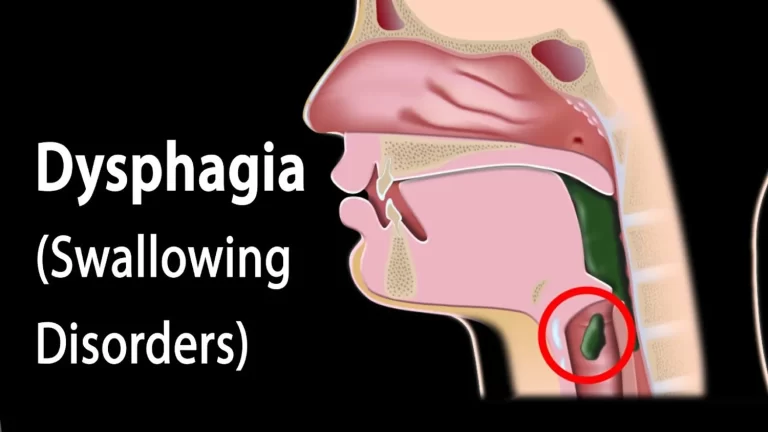
- Difficulty breathing
- Difficulty swallowing
- Pain that does not better with over-the-counter pain medications
- What questions should I ask my physician?
- Here are some questions to ask your dentist if you develop a periodontal abscess:
- What is the location of the abscess?
- How widespread is the infection?
- Do I require antibiotics?
- What are my therapy alternatives?
- How can I avoid this from happening again?
FAQs
Although an abscess in and of itself is not communicable, the bacteria that cause it can. Through direct contact with infected saliva, bacteria can spread. Avoid sharing cups, dining utensils, and other personal belongings if you have a periodontal abscess.
Under no circumstances should you attempt to pop a periodontal abscess. Call a dentist straight away if you believe you have a periodontal abscess.
A periodontal abscess cannot be treated at home. While some natural cures (such as warm saltwater rinses) can reduce discomfort, the infection cannot be cured.
A periodontal abscess is an infection that begins in your gums. A gum abscess can spread to other parts of your mouth and body if it is not treated, which can lead to additional problems. Better results come from solving the issue as soon as possible. A dentist can help if you believe you have a periodontal abscess.
Dental Abscess: How to Take Care of It
Your dentist will typically prescribe medications to stop the illness. In order for the infection to drain, he or she might need to cut open (lance) the abscess. Your pain should subside as a result. In order to repair bone damage brought on by the abscess, you could also require additional dental care, such as tooth extraction or oral surgery.
A fever and intense tooth pain are two symptoms of an abscess. Additionally, it might harm your teeth and gums over the long term. The teeth could become loose and disappear. It’s possible for the illness to spread to different bodily parts.
How Long Do Abscesses in Teeth Last?
In the same way, maintaining good dental health is essential for avoiding painful problems like abscesses in the first place. But it’s important to stress that if left untreated, dental abscesses can persist for weeks, months, or even years.
References:
1 Professional, C. C. M. (n.d.). Periodontal Abscess. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24573-periodontal-abscess
2 Periodontal abscess. (2023, July 6). Wikipedia. https://en.wikipedia.org/wiki/Periodontal_abscess