Deep Infrapatellar Bursitis
Table of Contents
What is a Deep Infrapatellar Bursitis?
Deep infrapatellar bursitis, a condition affecting the knee joint, involves inflammation of the deep infrapatellar bursa, a small fluid-filled sac located beneath the patellar tendon, close to the tibia bone.
Bursae are vital for reducing friction between tendons, muscles, and bones, facilitating smooth joint movement. When the deep infrapatellar bursa becomes inflamed, typically due to repetitive stress, overuse, or direct trauma, it can lead to discomfort, pain, and limited knee joint mobility.
This condition is often observed in individuals involved in activities that place significant strain on the knee, such as running, jumping, or kneeling. Effective management of deep infrapatellar bursitis involves a combination of rest, anti-inflammatory medications, physical therapy, and in severe cases, medical interventions. Early diagnosis and appropriate treatment can help alleviate symptoms and prevent further complications.
- There are many numbers of different types of bursae around the knee. The infrapatellar bursae are found just below the kneecap and sit around
- the patellar tendon, which is a large tendon that connects the quadriceps muscles to the lower leg.
- It is also known as a ‘Clergyman’s Knee’ which refers to an inflammation of the deep infrapatellar bursae. It causes pain and swelling at the front of the knee, just below the kneecap level.
Bursitis
- Bursitis is a painful condition that mainly affects the small, fluid-filled sacs called bursae— that cushion the bones, tendons, and muscles near your joints. Bursitis occurs when bursae get inflamed,
- The most common locations for bursitis are in the shoulder, in the elbow, and in the hip. But you can also have bursitis at your knee, heel, and at the base of your big toe. Repetitive movements or positions that put pressure on the bursae around the joints can lead to bursitis, and injury or overuse causes bursitis.
- At the knee, we can have prepatellar bursitis (housemaid’s knee) and infrapatellar bursitis.
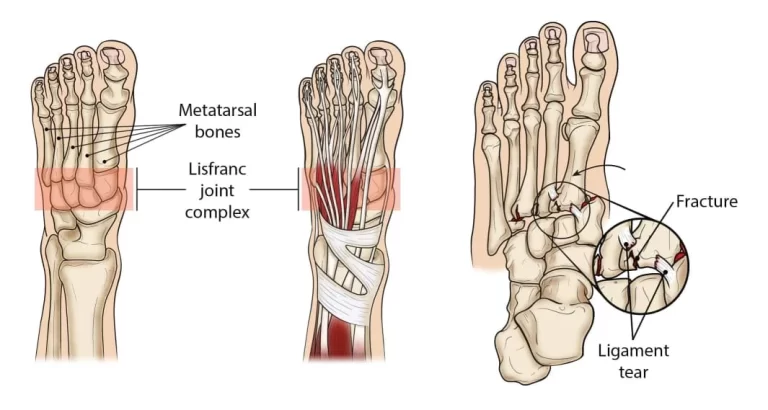
- The infrapatellar bursa is actually made up of two sacs which are
- Superficial Infrapatellar Bursa – which sits in front of the patellar tendon, between the tendon and the overlying skin,
- Deep Infrapatellar Bursa – which sits underneath the patellar tendon, between the tendon and the shin bone (tibia).
- For all intents and purposes, the superficial and deep infrapatellar bursae are treated as the one.
- The infrapatellar bursae protect the patellar tendon when you bend and straighten the knee and also allow it to glide smoothly and freely over the tibia as you move that
- Irritation, pressure on the knee, or friction on the bursa causes it to produce excess fluid as a protective mechanism to prevent damage which results in bursitis. The bursa gradually swells and if left untreated, may get thicken and harden. Later on, In extreme situations, calcifications may appear in the bursa.
Causes of Deep Infrapatellar Bursitis
- Frequent Kneeling or Crawling: when you are on your knees, excess pressure goes through the infrapatellar bursa, eg. squashing it. This causes the bursa to gradually thicken and then swell.
- Overuse: Activities that require more energy or frequent bending of the knee, such as running, jumping kicking, climbing, or stairs, place a lot of friction on the bursa and cause swelling.
- Injury: A sudden, hard blow to the front of the knee can break the infrapatellar bursa directly, or cause bleeding and excess fluid around the knee which seeps into the infrapatellar bursa, causing the swelling.
- Knee Conditions: Infrapatellar bursitis mostly develops secondary to other knee problems, most commonly jumpers knee (patellar tendonitis) and Osgood Schlatters Disease(OSD), etc
- Infection: When any kind of bacteria enter the infrapatellar bursa through a cut in the skin septic bursitis occurs causing an infection at the infrapatellar lesion
Symptoms of Deep Infrapatellar Bursitis
- Infrapatellar bursitis symptoms usually come on gradually over a few weeks or months and they consist of:
- Swelling: There is always swelling at the front of the knee with infrapatellar bursitis. There may be a squeezed pocket of fluid at the front of the shin, just below the kneecap which is also tender to touch
- Knee Pain: Pain is usually felt at the front of the knee, just below the kneecap, causing pain just below the knee. Pain may spread down the front of the shin if untreated. when you bend the knee and climb the stairs the pain gets exaggerated. Kneeling will be very painful when it squashes the bursae.
- Redness & Warmth: redness is present at the front of the knee. particularly with septic infrapatellar bursitis, and the skin may feel warm to touch
- Difficulty Sleeping: Sleep is often affected by bursitis with frequent waking up due to pain surges when bending the knee or rolling over as you sleep.
- Knee Stiffness & Weakness: The pain in the clergyman’s knee leads to stiffness and weakness in the joint because it doesn’t let your knee use
- Tenderness: Localized tenderness present at the front of the knee
Diagnosis
How to diagnose deep infrapatellar bursitis:
- If only one knee is painful then compare the condition of both knees.
- Gently press on the knee to detect warmth, swelling, and the source of pain.
- Inspect the skin that has an area for redness or other signs of infection
- Carefully move your legs and knees to check your knee’s range of motion and whether it hurts to bend or flex it
imaging test
- X-ray: An X-ray can be helpful in revealing a problem with a bone or arthritis.
- MRI: MRI technology visualizes soft tissues, such as bursae.
- Ultrasound: It can help your doctor better visualize swelling in the affected bursa.
Differential Diagnosis
There are various types of other conditions that cause knee pain at the front or below the knee with similar symptoms to infrapatellar bursitis.
If there is no swelling at the front of the knee; it might be something else is going on like;
- Jumpers Knee: inflammation in the patellar tendon.
- Osgood Schlatters: It is the most common cause of knee pain, which is caused by tension and inflammation just below the kneecap. It is most common in children.
- Runners Knee: A problem with how the kneecap moves and pain around the knee(patella)
- Chondromalacia Patella: breakdown of the cartilage under the kneecap.
- Plica Syndrome: Inflammation of the lining of the knee joint which has symptoms like pain, popping, effusion, localized swelling, reduced knee range of motion
Treatment of Deep Infrapatellar Bursitis
Medical treatment
Treatment Goals are
- to decrease pain
- to improve muscle range of motion
- increase muscle strength
Treatment options for deep infrapatellar bursitis are:
- NSAIDs
- anti-inflammatory drugs
- Rest: Avoid knee movements and exercises that increase your knee pain. Bursae need time to heal so rest should be compulsory
- Ice application
- Knee pressure off: Keep as much as possible pressure on your knee and try to avoid kneeling and crawling if you have to bend your knee then place a cushion or wear knee pads.
- Corticosteroid Injections: In some cases, a doctor might administer a corticosteroid injection directly into the bursa to reduce inflammation and pain. However, these injections are usually limited in number due to potential side effects.
- Assistive Devices: Using crutches or a brace temporarily can help reduce pressure on the affected knee, allowing it to heal.
- Activity Modification: Adjusting your activities to avoid overuse of the knee joint can prevent further irritation of the bursa.
Physiotherapy Treatment
- Modalities: we can give a patient heating modalities like ultrasound, iontophoresis, moist heat, and cryotherapy is also used.
Stretching and strengthening exercises
- Straight leg raising
- Heel slide
- Quadriceps stretch
- Quads set
- Hip adductor stretch
Straight leg raising
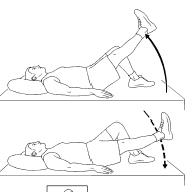
- The position of a patient: supine lying
- Bend your non-affected at 90 degrees and keep your affected leg straight on the floor.
- then stabilize your muscles on a straight leg by contracting your quadriceps.
- inhale slowly and lift slowly straight leg up to 6 inches from the ground.
- hold for 3 seconds.
- exhaling slowly and lowering the leg to the floor back.
- relax and repeat this 10 times more.
- if you do it correctly then you will feel the tension in your hip, thigh, and abdomen throughout the movement.
Heel slide

Patient position: supine lying
- Start slowly to slide your heel towards your buttocks part and keep sure your heel is in contact with the floor.
- then bend your knee until you feel pressure inside the knee.
Quadricep stretch
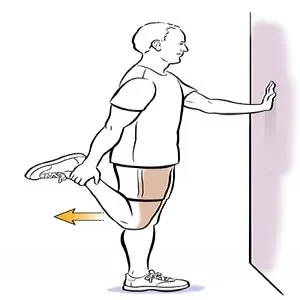
- Patient position: Stand near the wall
- Grasp your ankle and gently pull your heel upward and back towards the buttocks until you feel stretched in front of the thigh part(quadriceps muscle = anterior thigh muscle group).
Static quads

(static isometrics of quadricep muscle)
- Patient position: supine lying or long sitting
- Keep your leg straight
- Place a towel roll under your knee and then pull the toes up and press your knee to tighten the quadriceps muscle.
- this should cause your heel to slightly lift from the bed. hold for 7 seconds and repeat 10 times.
Hip adductor stretch

- Patient position: sitting
- Bend your knees and place the bottoms of your feet together then slowly let your knee down toward the floor until you feel stretched over the inner thigh muscle.
Prevention
- For preventing bursitis you should avoid direct injury or an overload of your muscles.
- Take a break between work and exercises
- avoid excessive squatting
- If you have to bend your or spend a lot of time on your knees then keep ensuring that you wear knee pads. This will help to prevent falling on the kneecap.
How long does bursitis last?
- Infrapatellar bursitis can last from a couple of weeks to a few months. If you regularly follow the recommended treatment above,
- Particularly resting from aggravating activities, then symptoms of clergyman’s knee should be decreased within a few weeks. Generally, as soon as you start treatment, the recovery will be quick.
Summary
- Deep infrapatellar bursitis is the major common cause of anterior knee pain. overuse and trauma are the main common causes. it includes swelling, stiffness, and pain while walking. With the help of a therapist and the use of medication, you may get a cure in 2-6 weeks.
FAQs
How long it take to get healed?
In most cases fully returning to normal daily activities will take from 2-6 weeks depending on the severity of the condition.
Can a patient do exercise with bursitis?
yes, they can do that. in fact, stretching and strengthening exercises are included in the treatment plan.
what are the complications of bursitis?
chronic pain
muscle atrophy
permanent thickening and enlargement of the bursaCan the patient do squats with bursitis?
long time kneeling and bending of the knee leads to inflammation of the bursae and irritate the knee. so if modifying your activities or work is not possible then try not to squat all the way down.
Which vitamin is beneficial in bursitis?
vitamin B12
Is hot water good for bursitis or not?
apply dry or moist heat like a heating pad or take a warm bath.






One Comment