Lisfranc Injury
Table of Contents
What is a Lisfranc Injury?
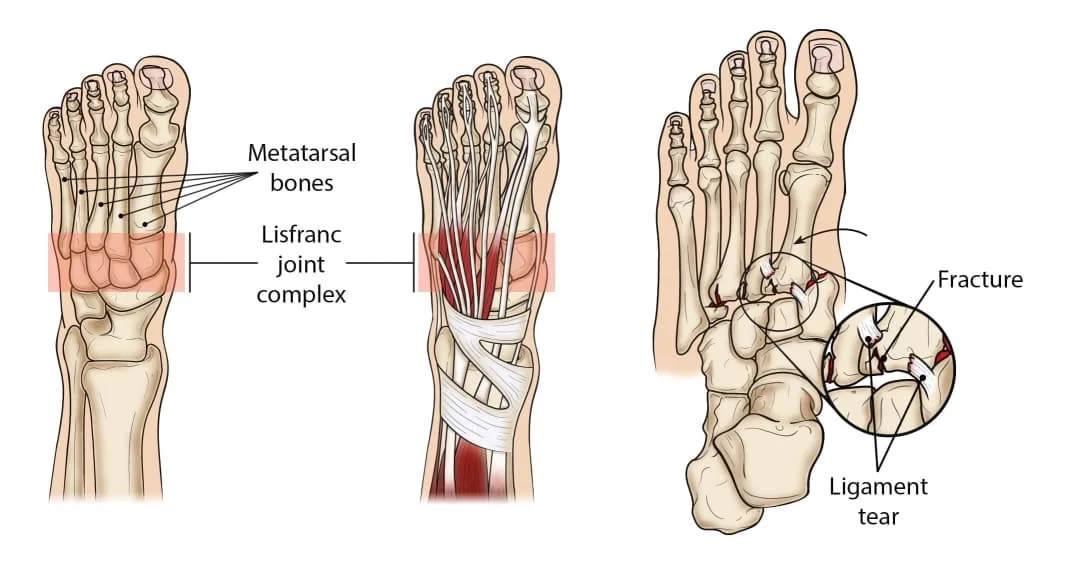
A Lisfranc injury, also known as a Lisfranc fracture or Lisfranc dislocation, is a type of foot injury that involves damage to the bones and/or ligaments in the midfoot region. This injury occurs at the Lisfranc joint complex, which is a cluster of joints and ligaments that connect the metatarsal bones (long bones leading to the toes) to the tarsal bones (bones in the midfoot). The Lisfranc joint complex plays a crucial role in maintaining the stability and flexibility of the foot during weight-bearing activities.
Lisfranc injuries can range from mild ligament sprains to severe fractures and dislocations. They are often the result of trauma, such as a direct impact to the foot (such as in a car accident) or a twisting injury during activities like sports. Additionally, Lisfranc injuries can occur gradually due to repetitive stress or overuse, especially in athletes participating in activities that involve running, jumping, and sudden changes in direction.
Level of Lisfranc Injury
There are different levels of severity for Lisfranc injuries, including:
- Sprains: Mild injuries where the ligaments connecting the metatarsal and tarsal bones are stretched or partially torn.
- Fractures: Involves a break in one or more of the bones in the Lisfranc joint complex.
- Dislocations: Occurs when the bones of the Lisfranc joint complex become displaced or move out of their normal position.
Causes of Lisfranc Injury
- Trauma: Direct trauma or impact to the foot, such as a fall from a height or a car accident, can result in a Lisfranc injury.
- Sports: Athletes involved in sports that require sudden stops, changes in direction, or high-impact movements, such as football, soccer, or skiing, are at a higher risk of Lisfranc injuries.
- Twisting: Twisting or rotating the foot excessively, especially while the foot is planted on the ground, can lead to ligament and bone damage in the midfoot area.
- Falls: Landing on the feet after a fall can cause the midfoot to absorb the impact, potentially resulting in a Lisfranc injury.
- Repetitive Stress: Repeated stress or overuse of the midfoot can weaken the ligaments over time, making them more susceptible to injury.
- Congenital Factors: Some individuals might have anatomic variations that predispose them to Lisfranc injuries.
Symptoms of Lisfranc Injury
- Swelling: Swelling in the midfoot area is a common early symptom of a Lisfranc injury.
- Pain: Pain in the midfoot that worsens with weight-bearing or movement is a typical sign. The pain can range from mild pain to severe pain.
- Bruising: Bruising along the bottom of the foot or on the top of the arch can develop due to bleeding and tissue damage.
- Difficulty Walking: Walking or putting weight on the affected foot can be painful and challenging.
- Instability: A feeling of instability in the midfoot region, often described as a sensation of the bones shifting, can be present.
- Difficulty Wearing Shoes: Shoes may feel uncomfortable or painful to wear due to the swelling and altered foot structure.
- Decreased Range of Motion: Limited ability to move the foot or toes as usual due to pain and swelling.
- Numbness or Tingling: Some individuals might experience numbness or tingling in the toes or foot due to nerve involvement.
- Visible Deformity: In severe cases, there may be a visible deformity or displacement of bones in the midfoot area.
Risk factors
- Sports Participation: Engaging in sports that involve rapid changes in direction, high-impact movements, or potential for foot trauma (such as football, soccer, basketball, and skiing) increases the risk.
- Trauma: Any situation that exposes the foot to significant force or impact, such as car accidents, falls from a height, or direct blows to the foot, can lead to a Lisfranc injury.
- Foot Shape and Structure: Individuals with certain foot shapes or structures, such as a high arch or a foot that is wider at the front, might have a higher risk due to the altered distribution of forces in the midfoot.
- Footwear: Wearing shoes that do not provide proper support or stability can increase the risk of foot injuries, including Lisfranc injuries.
- Previous Injuries: A history of previous foot injuries or instability can weaken the ligaments and bones, making the midfoot more susceptible to injury.
- Gender: Some studies suggest that men are more likely than women to sustain Lisfranc injuries, possibly due to differences in physical activity and body mechanics.
- Age: While Lisfranc injuries can occur at any age, they are more common among individuals in their 20s to 40s who are involved in physically demanding activities.
- Obesity: Excess body weight increases the forces placed on the feet during weight-bearing activities, which can contribute to midfoot injuries.
- Occupation: Certain occupations that involve standing for long periods, repetitive foot movements, or exposure to potential foot hazards can elevate the risk of Lisfranc injuries.
- Genetics: Some individuals might have a genetic predisposition to weaker ligaments or abnormal foot structures that make them more prone to this type of injury.
Diagnosis
The diagnosis of a Lisfranc injury typically involves a combination of clinical assessment, physical examination, and imaging studies.
- Medical History and Physical Examination: The doctor will ask about your symptoms, the circumstances of the injury, and your medical history. They will then perform a thorough physical examination of the foot, checking for pain, swelling, bruising, and any visible deformities. They may also assess your ability to move the foot and toes.
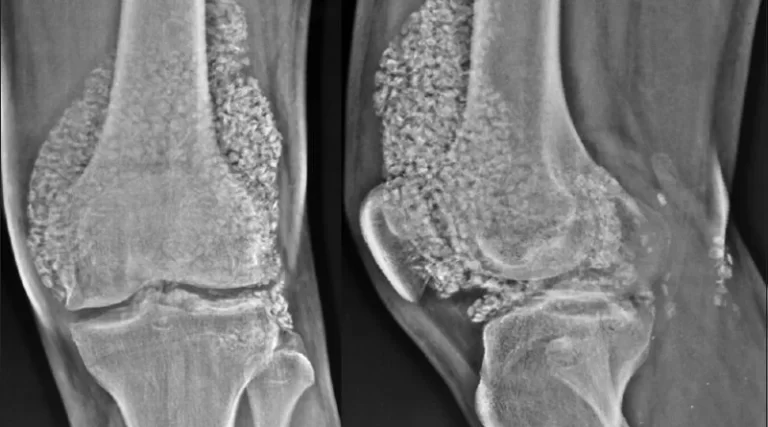
- X-rays: X-rays are often the first imaging study used to evaluate a potential Lisfranc injury. X-rays can help identify fractures, dislocations, and any changes in the alignment of the midfoot bones.
- Stress Tests: Sometimes, the doctor might perform stress tests, which involve applying pressure and evaluating how the midfoot bones move in response. This can help assess the stability of the midfoot.
- Additional Imaging: In some cases, more advanced imaging studies such as CT scans or MRI scans might be ordered. These imaging methods can provide more detailed views of the bones, ligaments, and soft tissues, helping to determine the extent of the injury.
- Clinical Evaluation: Based on the information gathered from the physical examination and imaging studies, the medical professional will make a diagnosis, categorizing the Lisfranc injury by its severity (ranging from sprains to fractures and dislocations).
- Consultation with Specialists: In complex cases, the patient might be referred to an orthopedic surgeon or a foot specialist for further evaluation and treatment recommendations.
Medical Treatment of Lisfranc Injury
The medical treatment for a Lisfranc injury depends on the severity of the injury and can vary from conservative measures to surgical intervention.
- Rest and Immobilization: Mild Lisfranc injuries, such as ligament sprains or minor fractures, may be treated with rest, ice, compression, and elevation (RICE). Immobilization using a cast, walking boot, or brace may be recommended to allow the injured area to heal.
- Pain Management: Over-the-counter pain relievers or prescribed medications may be recommended to manage aches and decrease inflammation.
Recovery from a Lisfranc injury can be a lengthy process, involving physical therapy and rehabilitation to regain strength, flexibility, and normal function in the foot. The outcome depends on the severity of the injury, the type of treatment received, and the adherence to rehabilitation protocols.
Physiotherapy Treatment
Physiotherapy plays a significant role in the recovery process for individuals with a Lisfranc injury. A physiotherapist (also known as a physical therapist) can design a tailored treatment plan to help improve the mobility, strength, and overall function of the injured foot. Here are some components of physiotherapy treatment for Lisfranc injuries:
- Pain Management: Physiotherapists can use techniques such as ice, heat, ultrasound, or electrical stimulation to manage pain and reduce inflammation in the injured area.
- Range of Motion Exercises: Gentle exercises are introduced to help restore the normal range of motion in the foot and ankle joints. These exercises prevent stiffness and promote flexibility.
- Strengthening Exercises: Specific exercises are prescribed to strengthen the muscles surrounding the foot and ankle. Strengthening these muscles can help support the injured area and improve overall stability.
- Balance and Proprioception Training: Balance and proprioception exercises help improve the body’s awareness of its position in space. This is crucial for preventing future injuries and enhancing stability.
- Gait Training: Physiotherapists work with patients to regain a normal walking pattern. They may use gait training exercises and techniques to ensure that weight-bearing is distributed appropriately.
- Functional Exercises: Physiotherapists design exercises that mimic everyday activities to help patients regain the ability to perform tasks like walking, climbing stairs, and getting in and out of chairs.
- Manual Therapy: Hands-on techniques like joint mobilization and soft tissue manipulation can aid in reducing stiffness, improving circulation, and promoting healing.
- Custom Orthotics: Physiotherapists may collaborate with orthotics to create custom orthotic devices that provide support and alignment for the foot during the recovery process.
- Patient Education: Physiotherapists educate patients about proper posture, body mechanics, and techniques to minimize strain on the foot and prevent future injuries.
- Progressive Plan: As the patient’s condition improves, the physiotherapist will gradually increase the intensity and complexity of exercises to support ongoing recovery.
Exercises
Here are some exercises that might be included in a physiotherapy program for a Lisfranc injury. Remember, it’s essential to consult a physiotherapist or healthcare professional before attempting any exercises to ensure they are appropriate for your specific condition.
Ankle Pumps:

Gently move your ankle up and down (dorsiflexion and plantarflexion) while keeping your foot elevated. This helps improve blood circulation and prevent stiffness.
Toe Flexion and Extension:
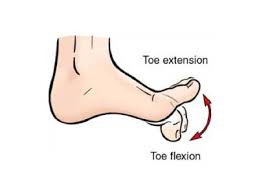
Slowly curl and uncurl your toes to work on the range of motion in your toes and the arch of your foot.
Ankle Alphabet:
Imagine you are writing the alphabet with your big toe in the air. This exercise helps improve ankle mobility in different directions.
Resistance Band Exercises:
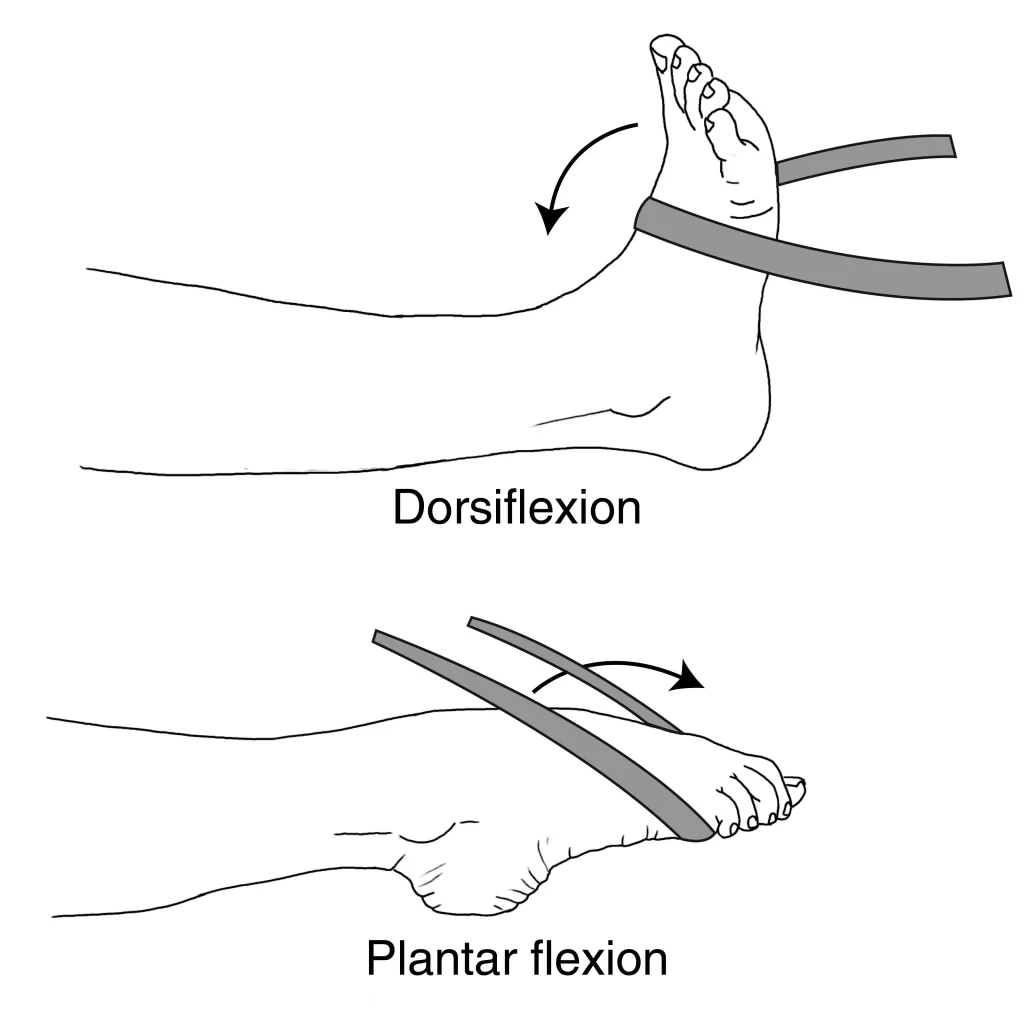
Using a resistance band, perform exercises like ankle dorsiflexion and plantarflexion against the band’s resistance. This helps strengthen the muscles around the foot area.
Toe Tapping:
Sit with your legs extended. Gently tap your toes on the floor, alternating between tapping the toes up and down. This exercise improves foot mobility.
Heel Raises:

Standing position with the patient’s feet flat on the floor. gradually raise the patient’s heels as high as possible, then lower them back down. heel raise exercise helps strengthen the calf muscles.
Toe Curls:

Place a towel on the ground and use your toes to scrunch it towards the patient’s. This exercise strengthens the small foot muscles in the foot.
Single Leg Stance:
Stand on the uninjured leg and balance for a short period of time. Progress by adding slight movements of the injured foot or closing your eyes.
Balancing on an Unstable Surface:
Stand on a foam pad or balance board to challenge your balance and stability. This can help improve proprioception.
Towel Pickup:
Place a small towel on the floor and use your toes to pick it up and release it. The foot arch muscles are strengthened by this workout.
Resisted Plantarflexion and Dorsiflexion:
Loop a resistance band around your foot and anchor the other end to a sturdy object. Sit down and gently press your foot against the band, pointing your toes away (plantarflexion), and then pull your toes towards you (dorsiflexion).
Calf Raises on an Elevated Surface:
Stand on a step or sturdy platform with the balls of your feet on the edge. Slowly raise your heels as high as you can, then lower them below the level of the step to stretch the calves.
Ankle Circles:
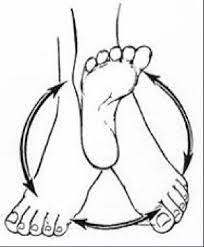
Sit on a chair with your feet off the ground. Slowly circle your injured foot in both clockwise and counterclockwise directions to improve ankle mobility.
Toe Squeezes:

Place small objects like marbles or a softball on the floor. Use your toes to pick up the objects and place them in a container. This exercise helps strengthen the muscles that control toe movement.
Towel Stretch:
Sit on the floor with your legs extended. Place a towel around the ball of your foot and gently pull the towel towards you to stretch the calf muscles and Achilles tendon.
Seated Ankle Inversion and Eversion:

Sit down with your legs extended. Attach a resistance band to a stationary object and wrap the other end around the injured foot. Move the patient’s foot inward (inversion) and outward (eversion) against the resistance.
Marble Pickup:
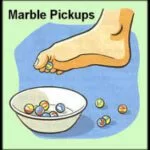
Place marbles on the floor and use the patient’s toes to pick them upside and place them in a container. This exercise helps improve toe strength and dexterity.
Standing Heel-to-Toe Balance:
Stand near a wall or counter for support. Place the heel of your injured foot against the toe of your uninjured foot. Attempt to balance in this position, gradually increasing the duration as your balance improves.
Resistance Band Toe Flexion:
Sit on the floor with your legs extended. Wrap a resistance band around your toes and gently flex them against the resistance of the band.
Toe Spread:
Sit on a chair with the patient’s feet flat on the ground. Spread your toes apart as much as you can, then bring them back together. This exercise improves toe mobility and strength.
Elastic Band Ankle Resistance:
Sit on the floor with your legs extended. Loop an elastic band around the top of your foot and hold the ends in your hands. Flex and extend your ankle against the resistance of the band.
Place the patient’s hands on a wall and step one foot back. Keep the patient’s back leg straight and the heel on the ground. Gently lean forward side to feel a stretch in the calf muscle of the back leg.
Toe Walking:

Walk on your tiptoes, engaging your calf muscles. This exercise helps strengthen the calves and improve balance.
Heel Slides:
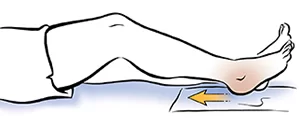
Lie on the patient’s back with the patient’s legs extended. Gently slide your injured heel towards your buttocks, bending your knee. Then, slowly slide it back to the starting position.
Single-Leg Balance with Eyes Closed:

Once you’re comfortable with single-leg balance, try closing your eyes while balancing. This adds an extra challenge to your proprioception and balance.
Ankle Eversion and Inversion with Resistance:

Attach the band to a sturdy object. Loop the other end around your foot and perform controlled eversion (moving the sole of your foot outward) and inversion (moving the sole of your foot inward) against the resistance.
Eccentric Calf Raises:
Stand on the edge of a step with the patient’s heels hanging off the edge. Raise both heels up onto your toes, then slowly lower your injured foot’s heel below the level of the step. Use your uninjured foot to assist in raising back up.
Intrinsic Foot Muscle Strengthening:

Place a small soft ball (such as a lacrosse ball) under your foot. Press down on the ball using your toes to work the muscles in the arch of your foot.
Foot Massage and Rolling:
Use a tennis ball or a foam roller to massage the bottom of the patient’s foot. Roll the ball or roller back and forth to release tension and improve blood flow.
Resistance Band Ankle Circles:
Sit down and loop a resistance band around your forefoot. Hold the band with both hands and create small circles with your ankle in both clockwise and counterclockwise directions.
Seated Toe Taps:
Sit on a chair with the patient’s feet flat on the floor. Lift your injured foot off the ground and tap your toes up and down in a controlled manner.
Calf Raises with Ball Squeeze:
Stand with your feet hip-width apart. Place a small soft ball between your ankles and perform calf raises while squeezing the ball with your ankles.
Seated Toe Stretch:
Sit down with your legs extended. Gently pull your toes back towards you using your hand to stretch the top of your foot.
Marble Roll:
Place marbles on the floor and use the injured foot to roll the marbles back and forth using only your toes.
Ankle Proprioception Exercises:
Stand on one foot and perform controlled movements such as shifting your weight from side to side, forward and backward, and making circles with your ankle.
Surgery
Surgery for a Lisfranc injury is typically considered when the injury is severe, involving significant fractures, dislocations, or ligament damage that cannot be effectively treated with conservative measures. The goal of surgery is to realign the bones, stabilize the midfoot, and restore proper function. Here’s an overview of the surgical options and the general process:
Surgical Options:
- Open Reduction and Internal Fixation (ORIF): This is a common surgical procedure where the surgeon uses screws, plates, or other devices to realign and stabilize the bones in the midfoot. The hardware holds the bones in place as they heal.
- Ligament Repair or Reconstruction: In cases of severe ligament damage, the surgeon might repair or reconstruct the damaged ligaments using sutures or grafts.
- Fusion: In some complex cases, fusion of the midfoot joints might be necessary. This involves permanently joining bones together to create stability.
- Surgery Process: Preoperative Evaluation: Before surgery, you’ll undergo a thorough evaluation, which may include imaging studies (X-rays, CT scans, MRI) to assess the extent of the injury and help the surgeon plan the procedure.
- Anesthesia: Surgery is typically performed under general anesthesia, meaning you’ll be asleep during the procedure. In some cases, regional anesthesia or nerve blocks might be used.
- Surgical Procedure: The surgeon makes incisions to access the injured area. They then realign the bones, repair ligaments, and stabilize the midfoot using screws, plates, or other devices. Once everything is in place properly, the incisions are closed.
- Recovery and Rehabilitation: After surgery, you’ll likely need to wear a cast, splint, or boot to protect the foot as it heals. Physical therapy will play a crucial role in the patient’s recovery, helping patients regain strength, mobility, and function.
- Follow-Up Appointments: You’ll have regular follow-up appointments with your surgeon to monitor healing and progress. X-rays may be taken to ensure the bones are healing properly.
- Weight-Bearing Progression: Your surgeon and physiotherapist will guide you on when you can start bearing weight on the injured foot and how to gradually increase activity levels.
- Return to Normal Activities: The timeline for returning to normal activities varies based on the severity of the injury, the type of surgery, and individual factors. It may take several months to regain full function and strength.
Prevention
Preventing Lisfranc injuries involves a combination of proper footwear, training techniques, and awareness of foot mechanics. Here are some steps you can take to reduce the risk of experiencing a Lisfranc injury:
- Choose Appropriate Footwear: Wear well-fitting shoes that provide good arch support, cushioning, and stability. Make sure your footwear is suitable for the activity you’re engaging in, whether it’s sports, exercise, or daily activities.
- Gradual Training: When starting a new exercise routine or sport, gradually increase intensity, duration, and intensity to give your feet and body time to adjust.
- Proper Technique: Practice proper techniques and body mechanics during sports and physical activities to minimize the risk of sudden twisting or impact on the midfoot.
- Warm-Up and Stretch: Always warm up before physical activity and perform appropriate stretching exercises to prepare your muscles and ligaments for movement.
- Foot Strengthening: Perform exercises that target the muscles in your feet and ankles to improve stability and support the arches.
- Cross-Training: Engage in a variety of physical activities to avoid overuse of specific muscles and reduce the risk of repetitive stress injuries.
- Terrain Awareness: Be cautious when navigating uneven or slippery surfaces to prevent trips and falls that can lead to foot injuries.
- Proper Shoe Lacing: Ensure your shoes are properly laced to provide a snug fit and prevent excessive movement within the shoe.
- Non-Weight-Bearing: In more severe cases, where there is significant instability or displacement of bones, non-weight-bearing status might be advised. This means avoiding putting any weight on the injured foot.
- Regular Foot Care: Keep your feet clean and dry to prevent infections. Regularly inspect your feet for any signs of discomfort, swelling, or changes in shape.
- Listen to Your Body: Pay attention to any discomfort, pain, or unusual sensations in your feet. If you experience persistent ache or discomfort, seek medical attention promptly.
- Orthotics: If you have certain foot biomechanical issues, consider using custom orthotic inserts to provide proper support and alignment.
- Stay Informed: Learn about common injuries associated with your sport or activity and take steps to minimize the risks.
- Follow-Up Care: Regular follow-up appointments with a medical professional are crucial to monitor the healing process, make necessary adjustments to treatment, and ensure proper recovery.
Complication
- Post-Traumatic Arthritis: Damage to the joints and cartilage in the midfoot can lead to post-traumatic arthritis, causing pain, stiffness, and reduced mobility over time.
- Chronic Pain: Incomplete or inadequate healing of fractures or ligament injuries can result in chronic pain that affects daily activities and quality of life.
- Instability: If the ligaments and bones of the midfoot do not heal properly, the foot’s stability can be compromised, leading to chronic instability and difficulty with weight-bearing activities.
- Altered Foot Mechanics: Lisfranc injuries can change the way your foot functions, affecting gait and movement patterns, which might contribute to pain and dysfunction.
- Decreased Range of Motion: Scarring and inadequate healing can lead to decreased range of motion in the foot and ankle joints.
- Nerve Damage: Injuries to nerves in the foot can result in numbness, tingling, or other sensory disturbances.
- Secondary Deformities: Improper healing can lead to deformities in the midfoot, affecting the alignment of the bones and joints.
- Recurrent Injuries: An improperly healed Lisfranc injury can increase the risk of future foot injuries and complications.
- Delayed Healing: Some Lisfranc injuries might take longer to heal, and complications can arise if the injury is not managed appropriately.
- Complex Surgical Outcomes: Surgical intervention, while often necessary, can carry risks such as infection, hardware-related complications, or unsatisfactory surgical outcomes.
- Psychosocial Impact: Living with chronic pain or functional limitations due to a Lisfranc injury can have emotional and psychological effects.
Home Advice
- Rest and Elevate: Spend time resting and elevating the patient’s injured foot. Elevating the foot above heart level can help decrease swelling and promote circulation.
- Ice Application: Applying ice to the injured area for about 15-20 minutes every few hours can help alleviate swelling and reduce pain. Be sure to use a cloth or towel as a barrier between the ice pack and the patient’s skin.
- Pain Management: Take prescribed or over-the-counter pain medication as directed by your healthcare provider to manage pain and discomfort.
- Follow Rehabilitation Exercises: Perform the prescribed exercises provided by your physiotherapist to improve strength, flexibility, and mobility in the injured foot.
- Weight-Bearing Progression: If advised by your healthcare provider, gradually transition from non-weight-bearing to partial weight-bearing and eventually full weight-bearing as you heal.
- Nutrition and Hydration: Maintain a balanced diet rich in nutrients to support the healing process. Staying hydrated is also important.
- Foot Elevation While Sleeping: Use pillows to prop up your injured foot while sleeping to help minimize swelling.
- Foot Hygiene: Keep the patient’s foot clean and dry to prevent infection. Follow any wound care instructions provided by the patient’s healthcare provider.
- Proper Footwear: Wear comfortable and supportive shoes or sandals that provide adequate support and protection for your injured foot.
- Assistive Devices: If recommended by the patient’s healthcare provider, use crutches, a walker, or a cane to help you move around safely while the patient’s foot heals.
- Avoid High-Impact Activities: Refrain from engaging in high-impact activities or putting excessive stress on the patient’s injured foot during the initial stages of recovery.
- Stay Positive: Maintain a positive attitude and remain patient throughout the recovery process. Healing takes time, and it’s important to give your body the opportunity to recover fully.
- Follow Medical Advice: Adhere to your healthcare provider’s recommendations regarding follow-up appointments, medication, and activity restrictions.
- Communicate: If you experience any unexpected symptoms or changes in your condition, contact your healthcare provider promptly.
It’s important to promptly seek medical attention if you suspect a Lisfranc injury, as untreated or improperly managed cases can lead to chronic pain, instability, and long-term complications.
FAQ
A Lisfranc injury is a type of foot injury that involves damage to the ligaments and bones in the midfoot area. It can range from ligament strains to fractures and dislocations.
Lisfranc injuries can be caused by direct trauma, such as a fall or a car accident, as well as by sports-related activities involving sudden stops, changes in direction, or high-impact movements.
Common symptoms include swelling, pain in the midfoot, bruising, difficulty walking, instability, and difficulty wearing shoes.
Diagnosis involves medical history, physical examination, and imaging studies such as X-rays, CT scans, and MRI scans.
Mild Lisfranc injuries, such as ligament sprains, can often heal with conservative treatment methods like rest, immobilization, and physical therapy. Severe injuries may require surgery.
Prevention involves wearing appropriate footwear, practicing proper techniques during physical activities, and maintaining foot strength and flexibility.
Rest, elevate the foot, apply ice, take prescribed pain medication, follow rehabilitation exercises, and maintain good foot hygiene.
complications can include chronic pain, post-traumatic arthritis, instability, altered foot mechanics, and decreased range of motion, among others.
Surgery may involve realigning bones, repairing ligaments, and stabilizing the midfoot using screws, plates, or other devices. The specifics depend on the severity of the injury.
Recovery times vary, but it can take several months to regain full function. Physiotherapy treatment plays a crucial role in the rehabilitation process.