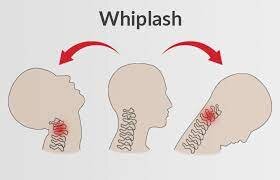
Whiplash Injury (Neck Strain)
Whiplash is an injury that takes place when sudden force or movement of the neck and spine, damaging bone, muscle, ligaments, and nerves. It is most common in motor vehicle crashes, but may also take place for other reasons. It is generally treatable and short-lived. Although, some individuals experience chronic effects like Neck pain for months or even years.
Table of Contents
What is whiplash?
Whiplash is a condition that takes place when sudden movement changes force the neck (cervical spine) and upper spine to move in ways that cause injury. This causes a formation of neck sprain.
Whiplash refers to an only concept that may have a wide range of effects. Doctors refer to conditions that occur because of whiplash as “whiplash-associated disorders.” Whiplash may also occur with sudden movement changes in any direction.
Because it includes a neck injury, first responders and medical personnel will frequently treat whiplash as an emergency condition. Doctors will also approach it with extreme caution until they may confirm, treat and stabilize a dangerous injury, or find out that kind of injury.
Whom does whiplash affect?
- Whiplash may affect anyone at any age but is more likely to cause serious or lasting injuries in two groups: older adults and females and an individual assigned female at birth (AFAB).
- It is more serious in older adults (over age 65) because they are typically more prone to muscle and bone injuries of any kind.
- That is generally because of age-related muscle and bone deterioration and weakening.
- Females and people AFAB are more likely to have whiplash-type injuries in car crashes, which can be because of several factors:
Height-
- Experts suspect that is due to women and people AFAB having a shorter average height compared to males and people assigned male at birth (AMAB).
Spine structure differences–
- Females and individual AFABs also have a different spinal column structure than males and individual AFABs.
- That influences the distance between each vertebra (the interlocking bones that make up your spine).
Muscle differences-
- Females and individual AFABs generally have less muscle tissue, which may perform as a shock absorber to decrease the effects of sudden impact forces.
- That means they have the less available muscle to help absorb movement forces.
Vehicle construction-
- Modern vehicle construction can contribute to the risk of injury for females and individual AFABs.
- Head restraints (better known as headrests) are there to stop the head from moving backward too far in a collision.
- Because females and an individual AFAB have a shorter average height, seat back and headrest height can affect them differently.
How common is whiplash?
- Whiplash is fairly common, affecting millions of individuals worldwide each year.
How does Whiplash affect the person’s body?

- Whiplash takes place because of how one law of physics, the law of inertia, affects the human body.
- Think about what it is like to be in a moving vehicle when the driver immediately steps on the brakes.
- Inertia is why the body keeps moving forward even though the vehicle is stopping.
- Inertia is also why a person presses back into the seat if the driver immediately steps on the gas and goes from a complete stop to quick acceleration.
- Just like a people are a passenger in the car in the above analogy, the brain is a passenger in the skull.
- Sharp, sudden movements may cause the brain to smack against the inside of the skull, causing injury to the brain.
- That is why the neck is like a shock absorber for the head, naturally compressing, extending, or twisting to minimize the effect of immediate movements on the brain.
- Whiplash happens when inertia causes the head, neck, and body to move at different speeds.
- The forces of the neck compress or extend too rapidly or in ways that push the muscles, ligaments, and bones of the spine beyond what they may tolerate.
- The sharper and stronger the motion, the greater the force on the neck.
- That is why whiplash injuries may range from minor to severe.
- Although, even little levels of force may still cause moderate or severe whiplash.
- Experts do not fully understand why this takes place, but research is ongoing.
- At its worst, whiplash may break the vertebrae in the neck, generating a risk of damage to the spinal cord and its network of connected nerves.
Clinically Relevant Anatomy
Whiplash and whiplash-associated disorders (WAD) affect a variety of anatomical structures of the cervical spine, based on the force and direction of impact as well as too many other factors. Causes of pain may be any of these tissues, with the strain injury resulting in secondary edema, hemorrhage, and inflammation:
- Joints: zygapophyseal joints, Atlanto-axial joint, atlanto-occipital joint
- Intervertebral discs and cartilaginous endplates
- Muscles
- Ligaments: Alar ligament, Anterior atlanto-axial ligament, Anterior atlanto-occipital ligament, Apical ligament, Anterior, longitudinal ligament, Transverse ligament of the atlas
- Bones: Atlas, Axis, vertebrae (C3-C7)
- Nervous systems structures: Nerve roots, spinal cord, brain, sympathetic nervous system
- The vascular system structures: Internal carotid and vertebral artery
- Adjacent joints: Tm joint, thoracic spine, ribs, shoulder complex
- The peripheral vestibular system
Pathology
Most WADs are considered to be minor soft tissue-dependent injuries without any evidence of fracture. The injury happens in three stages:
- Stage 1: The upper and lower spines feel flexion in stage one
- Stage 2: The spine presumes an S-shape while it initiates to extend and eventually straighten to make the neck lordotic again.
- Stage 3: Shows the whole spine in extension with an exceptional Sheering force that causes compression of the facet joint capsules.
Studies have proven that whiplash injury is the formation of the S-shaped curvature of the cervical spine which incorporates hyperextension on the lower end of the spine and flexion to the upper levels, which surpasses the physiologic limits of spinal cord mobility.
The Quebec Task Force classifies patients with WAD (whiplash), depending on the severity of signs and symptoms, as follows:
- Grade 1 -The person complains of neck pain, stiffness, or tenderness with no positive findings on the physical exam.
- In grade 2 The patient exhibits musculoskeletal signs including decreased range of motion and point tenderness.
- In grade 3 The patient also shows neurologic signs that may involve sensory deficits, decreased deep tendon reflexes, and muscle weakness.
- In grade 4 the patient shows a fracture.
What causes whiplash?
Whiplash takes place when the movement speed or the direction a person is traveling suddenly changes. Some of the most usual events or activities that may lead to whiplash involve:
- Motor vehicle crashes (these are the most usual cause of whiplash).
- Contact sports (like football, hockey, rugby, etc.).
- Roller coasters.
- While the above are the most usual possible causes, whiplash may take place in many other ways.
- Even simple slips and falls may cause whiplash under the right circumstances.
Symptoms and Causes of Whiplash Injury
The symptoms of whiplash are based on how severe the whiplash was and how severely the neck is hyperextended or compressed. The greater the extension or compression, the deeper the injury. A vital part of whiplash symptoms is the timing. Some symptoms of whiplash can start quickly after a crash, while others take at least 12 hours to appear.
Sometimes, it may take a whole day or even a few days for all the symptoms to show up. Because whiplash may have too many different effects, experts generated a grading system for the severity of whiplash-associated disorders. Identify as the Quebec Classification of Whiplash-Associated Disorders, this grading system (with more details about each grade immediately below) is as follows:
- Grade 0: No injury.
- Grade 1: Pain only.
- Grade 2: Pain plus signs of injury.
- Grade 3: Pain and also a sign of injury and neurological effects.
- Grade 4: Severe pain and signs of serious or dangerous neurological symptoms.
Grade 0
- At this level, a patient with whiplash does not feel any pain or show any signs or symptoms of injury.
Grade 1
- This level of whiplash is the initial one where a person experiences pain. They will also show Stiffness when moving.
- Tenderness to being touched around the injury.
Grade 2
- This is the first level where a patient feels pain and other symptoms from Grade 1, plus physical signs of an injury.
- The pain also may also have various effects from Grade 1.
- The symptoms of Grade 2 whiplash involve.
- Pain radiates to surrounding areas like the head, face, shoulder, and back.
- Muscle spasms make it hard to move or turn the head and neck.
- Physical signs of injury, involve bruising, swelling, and sensitivity to being touched around the injury.
Grade 3
- Grade 3 whiplash involves neurological symptoms.
- These take place due to swelling or inflammation disrupting nerve signals traveling through the injured area on the way to or from the brain. These symptoms involve:
- The whiplash-associated disorder is a compound condition with varied disturbances in motor, sensorimotor, and sensory functions and psychological distress.
- The most usual symptoms are sub-occipital headache and/or neck pain that is ongoing or motion-induced.
- There can be up to 48 hrs delay of symptom onset from the time of injury.
Motor Dysfunction
- Limited range of motion of the cervical spine.
- Altered patterns of muscle recruitment in both the cervical spine and shoulder girdle areas (clearly a feature of chronic WAD).
- Mechanical cervical spine instability
- Sensorimotor Dysfunction (Greater in persons who also reports dizziness due to neck pain)
- Loss of balance
- Disturbed neck-influenced eye movement control
Sensory Dysfunction:
- Sensory Hypersensitivity to different types of Stimuli.
Other symptoms
- Psychological distress
- Post-traumatic stress
- Concentration and memory problems
- Sleep disturbances
- Anxiety
- Depression
- Initial depression: Connected with greater neck and low back pain severity, numbness/tingling in arms/hands, vision problems, dizziness, and fracture.
- Persistent depression: Connected with older age, greater initial neck, and low back pain, post-crash dizziness, anxiety, numbness/tingling, vision, and hearing problems.
- Degeneration of Cervical Muscles
- Neck stiffness
- Fatty infiltrate can exist in the deep muscles in the suboccipital region and the multifidi may account for some of the functional impairments like Proprioceptive deficits, Balance loss, and Disturbed motor control of the neck.
Other Symptoms
The following symptoms can also take place:
- Tinnitus
- Malaise
- Disequilibrium/Dizziness
- Thoracic, temporomandibular, facial, and limb pain
- It is necessary to carry out thorough spinal and neurological examinations in patients with WAD to screen for delayed onset of cervical spine instability or myelopathy.
- Whiplash may be an acute or chronic disorder.
- In acute whiplash, symptoms last no longer than 2-3 months, while in chronic whiplash symptoms last more than 3 months.
- Persons with acute WAD feel widespread pressure hypersensitivity and decreased cervical mobility.
- Too many different studies indicate that there may be a voluntary recovery within 2-3 months.
- According to the Quebec Task Force of WAD (QTF-WAD), 85% of the patients recover within 6 months.
- Additionally, according to a follow-up study, some symptoms were already transient at baseline and symptoms like neck pain, decreased cervical range of motion, headache, and low back pain, were reduced further over the six months period.
- They also identified the prevalence of depression and found that at baseline this was around 5% in both women and men, whereas post-traumatic stress and anxiety were more common in females (19.7% and 11.7%, respectively) compared to males (13.2% and 8.6%).
- The majority of all reported connected symptoms were mild at both baselines and during follow-up.
Diagnosis and Tests
- Whiplash is a diagnosis of exclusion.
- That means doctors make the diagnosis after finding out more serious conditions that need immediate treatment or other possible causes.
- Finding out those other conditions includes a combination of diagnostic tests, imaging scans, physical and neurological examinations, and more.
- Doctors also ask some questions about the symptoms and any events that could have caused the whiplash, specifically car crashes.
What tests will be done to diagnose whiplash?
There are too many possible tests, most of them imaging scans, that may help a provider find out other conditions or issues and diagnose whiplash, involving:
- X-rays.
- Computerized tomography (CT) scans.
- Magnetic resonance imaging (MRI) scans.
Outcome Measures
- Neck Disability Index
- Visual Analogue Scale (VAS)
- Pain Catastrophizing Scale
- The Whiplash Activity a participation List (WAL)
- Disabilities of the Arm, Shoulder, and Hand (DASH) in preserving Whiplash
- SF-36
- Functional Rating Index
- The Self-Efficacy Scale
- The Coping Strategies Questionnaire
- Patient-Specific Functional Scale
- General Health Questionnaire (CHQ)
Differential Diagnosis
It includes:
- Cervical spine fracture
- Carotid artery dissection
- Herniated disc
- Spinal cord injury
- Subluxation of the cervical spine
- Muscle strain
- Facet injury
- Ligamentous injury
Treatment of Whiplash Injury
Whiplash is treatable, but there is no way to cure it directly. Alternatively, the goal of treatment is to permit whiplash to heal as much as possible while supporting that healing process and decreasing symptoms. Some individuals can also require care for chronic issues that occur because of whiplash.
What medications or treatments are used?
Some treatments for whiplash are most helpful immediately after an injury, while others are best if utilized to treat the long-term effects and chronic problems from a whiplash injury. Some individuals may do both. The most usual treatments for whiplash (with more about them below) involve:
Painkillers
These range from over-the-counter drugs like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, etc. Stronger painkillers, like opioids, are also possible for moderate to severe pain. Although, doctors prescribe these very cautiously because of the risk of long-term dependence or addiction to these drugs.
Anti-inflammatory drugs-
- These medications decrease swelling from inflamed tissue.
- Swelling from whiplash may lead to other symptoms if it presses on nerves and keeps signals from going to or coming from the brain.
Muscle relaxers-
- Sprained muscles may frequently spasm uncontrollably, causing severe pain and preventing healing from an injury.
- Muscle relaxers cause muscles to relax, reduce spasms and give those muscles a chance to heal.
Nerve blocks-
- Blocking nerve signals may provide relief to the person dealing with severe or chronic pain from whiplash.
- Many other kinds of medications are also possible.
- The physician is the best person to tell you about the available medication options they suggested.
Radiofrequency (RF) nerve ablation
- One way to treat chronic pain is to stop the nerves in the injured area from sending pain signals.
- This is specifically helpful when an injury leads to nerve damage, making the affected nerves send pain signals more than they should.
- This treatment uses RF energy to heat the involved nerves and intentionally damage them, so they stop sending pain signals.
- This may reduce pain for weeks or months.
Conservative methods
- Immobilization.
- Medications.
- Cold application for the first seven to a few days. Heat application is recommended after that.
- Exercise/physical therapy.
- Transcutaneous electrical nerve stimulation (TENS) therapy.
- Radiofrequency nerve ablation.
Surgical methods
Spine surgery
- Immobilization
- Because whiplash may affect the spine and spinal cord, it is usual for people with possible neck and spine injuries to receive some form of protective care instant.
- An example is a cervical collar (C-collar), which emergency medical personnel may put on a patient’s neck at the scene of a car crash.
- A C-collar has a rigid frame that holds the head and neck in alignment, so the vertebrae do not press on or damage the spinal cord.
- That also helps keep the neck muscles from bearing the weight of the head, which might be very painful if the neck muscles are injured.
- There are also other forms of immobilization.
- A doctor is the best person to tell you about the available forms and which form they suggested.
Physiotherapy treatment
Applying cold and heat
- Experts suggested using cold packs at the time the first seven to 10 days to reduce swelling and inflammation.
- After that, gentle warmth and heating may help increase blood flow to an affected area, which helps to give the healing of damaged tissues.
Ultrasound
Ultrasound sends sound waves into the injured area, which creates light heat. This gives healing and enhances circulation. This improves blood circulation and helps reduce:
- Muscle spasms
- Cramping
- Stiffness; and
- Pain
Transcutaneous electrical nerve stimulation (TENS) therapy
- Transcutaneous electrical nerve stimulation, or TENS for short, is a therapy that delivers a mild electrical current through the skin to surface nerve endings.
- The nerves use electrical signals to communicate, so using an outside electrical current at low levels may help with pain in those areas.
- Using a TENS unit to reduce the pain is much like using white noise to help block out other sounds while a person is sleeping.
Deep tissue massage
- This may help release tension in the soft tissues of the neck and shoulders and can help the body heal faster. And it can feel good to release that tension, which is a bonus.
Exercise therapy
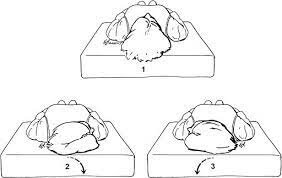
Chin Tucks
Purpose: To stretch the muscles in the cervical spine and promote good posture.

- Start with lying on your back.
- As a person looks toward the ceiling, move the chin toward the chest.
- Hold for 10 seconds. A person should experience a comfortable stretch from the neck to the base of the head.
- Repeat this stretch up to five times.
Chin tuck in a seated position:

- Use correct sitting posture.
- Looking forward, move the head back so the chin is tucked down. Nothing beneath the head should move.
- Hold the position for 1o seconds.
- Repeat this stretch up to 5 times.
Side-to-Side Head Rotation
Purpose: To reduce tightness in the sides and back of the neck, and improve mobility in the neck.
A side-to-side head rotation in a lying down position:
- Start with lying on the back.
- Rotate the chin toward the right shoulder.
- A person can use the hand to slowly pull the head further into the stretch.
- Hold for 10 seconds.
- Rotate the chin toward the left shoulder.
- A person can use the hand to move the head further into the stretch.
- Hold for 10 seconds.
- Repeat the stretch 5 times on both sides.
A side-to-side head rotation in a seated position:
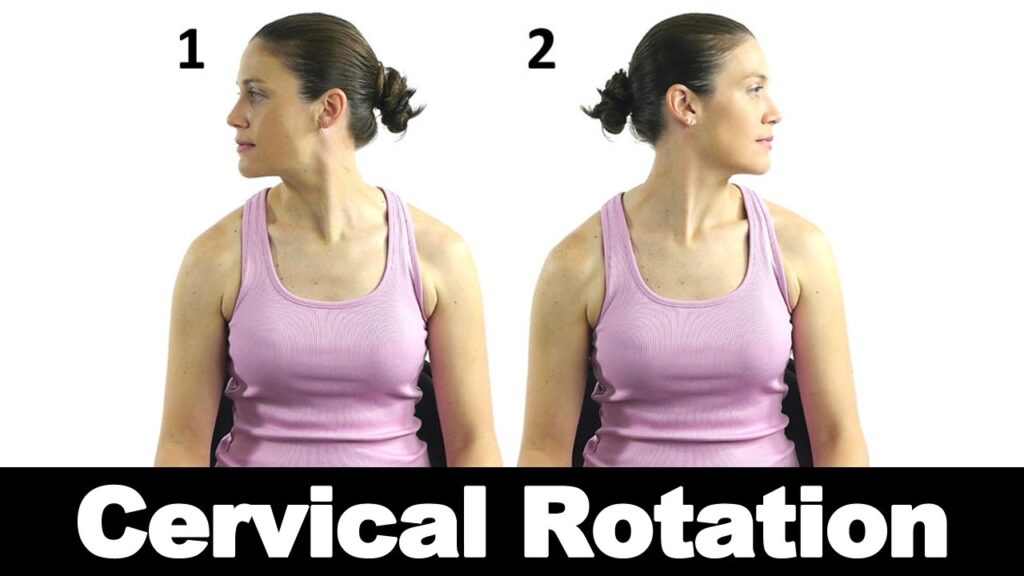
- Make sure a patient is seated in good posture.
- Rotate the chin toward the right shoulder.
- A person can use the hand to slowly pull the head deeper into the stretch.
- Hold for 10 seconds.
- Rotate the chin toward the left shoulder.
- A person can use the hand to pull the head deeper into the stretch.
- Hold for 10 seconds.
- Repeat the stretch 5 times on both sides.
- Slowly moving the head from side to side may help relieve tight neck muscles and improve flexibility and movement.
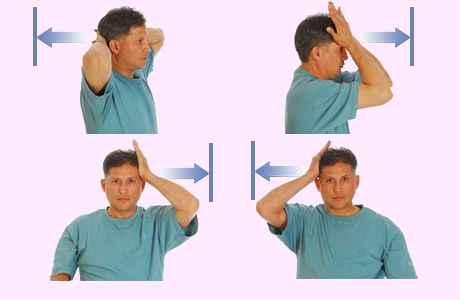
Side Bending
Purpose: To relieve a stiff neck or tightness in the sides of the neck and improve neck flexibility and mobility.
Side bending exercise in a lying down position:
- Start with lying on the back.
- Move the head to the right, bringing the right ear close to the right shoulder.
- A person can use the hand to slowly pull the head deeper into the stretch.
- Hold for 10 seconds.
- Repeat on the left side, lowering the head so the left ear moves closer to the left shoulder.
- A person can use the hand to pull the head deeper into the stretch.
- Hold for 10 seconds.
- Repeat 5 times on both sides.
Side bending stretch in a seated position:
- Make sure a person is seated in good posture.
- Lower the right ear toward the right shoulder.
- A person can use the hand to slowly pull the head deeper into the stretch.
- Hold for 10 seconds.
- Lower the left ear toward the left shoulder.
- A person can use the hand to pull the head deeper into the stretch.
- Hold for 10 seconds.
- Repeat 5 times on each side.
Scapular stabilization exercise
Purpose: to relieve the neck pain

- Start with lying in a prone position with the arms hanging at the side, the head facing straight ahead, and the shoulders relaxed.
- Move the shoulders slowly backward and pull the shoulder blades into a down and back position.
- The chest should protrude forward minimally while making this motion
- Hold for 5 seconds
- Complete 3 repetitions two times per day then a person may improve the duration gradually
- After that as a progression a person may use a thera band to a door and then pull toward you with both ends of it while doing a scapular squeeze.
Isometrics
Aim: for strengthening the muscles of the neck, upper back
- Place the palm on your forehead
- Push the head against the palm without bending the neck at all
- Hold for 5 seconds
- Repeat 5 times per day
Prone cobra
Aim: for strengthening the muscles of the neck, upper back, and shoulder griddle.

- Start with lying on the floor with the face down, a person may put a rolled hand towel under the forehead for comfort.
- Place the arms at the sides with palms down on the floor
- Put the tongue at the roof of the mouth to stabilize the muscles in the front of the neck to assist in strengthening
- Squeeze the shoulder blades and lift the hands off the floor
- Roll the elbows in, palms out, and thumbs up
- Gently lift the forehead slowly about one inch off the towel with keeping the eyes looking at the floor
- Hold for 5 seconds, then perform 10 repetitions.
The corner stretch:
Aim: for stretching the muscles of the chest and front of the neck, and positioning the scapulae

- Face the corner of a room or put the forearms on the door jams
- Try to make the feet position about 2 feet away from the corner
- Put the forearms on each side of the wall with the elbows slightly below shoulder height.
- Lean forward till a person feel a good stretch across the chest and shoulders
- Hold for 10 seconds, It may be done 5 times per day.
Levator scapular stretch:
Aim: Stretching the levator scapulae, which is often the big knot in your upper back

- Start with sitting in the correct sitting posture with keeping your shoulders down
- Grasp the bottom of the seat with one hand
- Gently turn the chin toward the armpit till feeling a comfortable stretch on the opposite side of the neck
- Hold for 10 seconds then do it one more time for the opposite side.
- Perform 5 repetitions two times daily.
Serratus wall slide – light strengthening
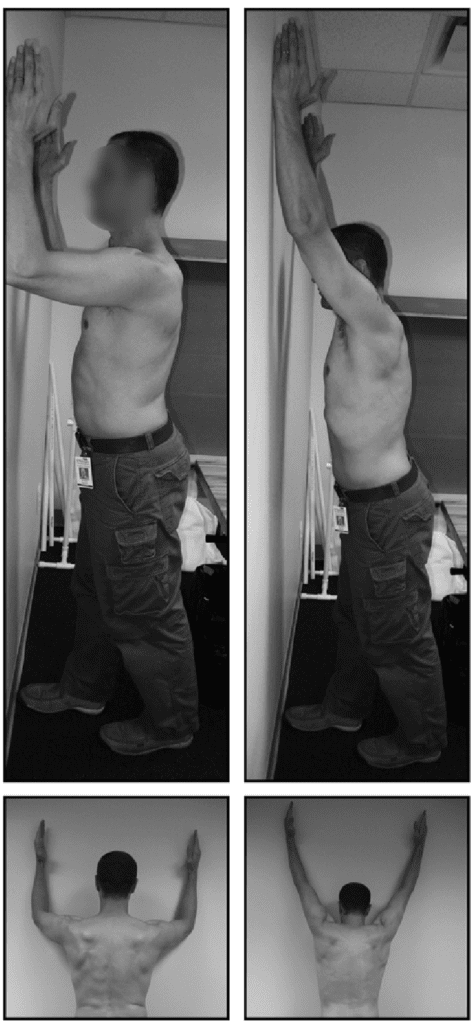
- The serratus anterior muscle is a muscle that arises from the shoulder blade and is muffled upward and forward to the rib cage.
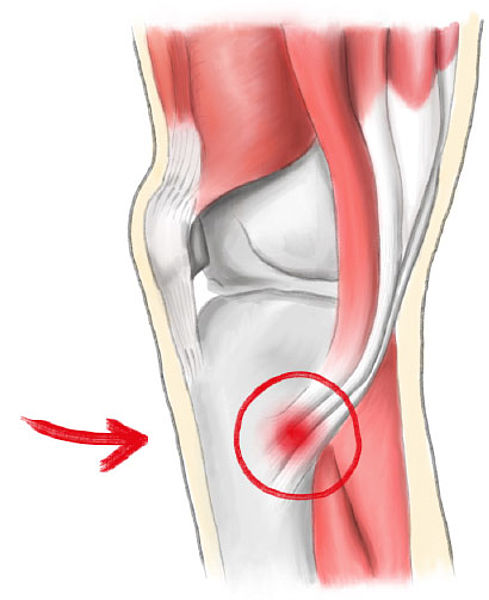
- The serratus is a stabilizing muscle of the shoulder studies. show that the timing of this muscle is compromised in individuals who have had a whiplash injury.
- This may lead to poor mechanics with reaching and moving the arm which may make individuals who have had a whiplash injury more likely to suffer a shoulder injury.
- The serratus wall slide may be helpful for retraining this muscle.
- Two sets of 5 reps.
FAQ
While whiplash does not have a perfect appearance in MRIs, they are useful for diagnosis. First, MRIs may find out things like fractures, slipped discs, or other severe injuries that can cause pain, allowing doctors to identify whiplash as the primary injury to treat.
A person has tingling or pins and needles on one or both sides of the body. A person has problems with walking or sitting upright. you have a sudden “electric shock” feeling in the neck and back which can also go into the arms and legs.
Worsening of pain with neck movement. Decreased range of motion in the neck. Headaches, most frequently starting at the base of the skull. Tenderness or pain in the shoulder, upper back, or arms.
Avoid lifting, sports, or other activities that might strain the neck. Try sleeping on a special neck pillow. Put it under the neck, not under the head. Putting a tightly rolled-up towel under the neck while you sleep will also work.
However, a person can want to avoid exercise or sports that could put her in danger of reinjuring the neck. Contact sports or high-impact exercise routines are not suggested. Instead, stick with low-impact exercises like walking, yoga, or dancing until the neck has healed completely.





One Comment