Flexor Tendon Injury
Table of Contents
What is A Flexor Tendon Injury?
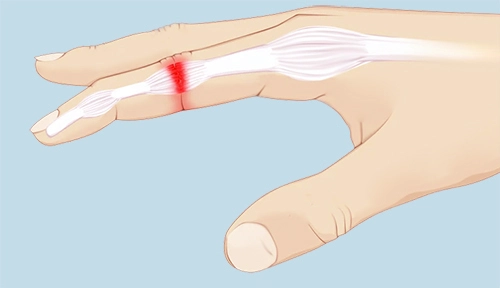
Flexor tendons are cord-like arrangements passing from the forearm across the wrist and palm and into the fingers, allowing you to bend the fingers and thumb to grasp any object or make a fist. Injury to the flexor tendons can cause you to lose the capability to flex one or more of the joints in the hand. Injuries to the flexor tendons can cause a person to lose the incapability to bend one or more of the joints in her hand.
Flexor tendon injury is the most common and complex injury managed by hand surgeons. The flexor tendon mechanism plays an important role in the functionality of the hand. A good deal of the treatment methods, restoring stages, clinically relevant anatomy, and restoration of these damages is needed for a satisfactory result in the patient with a flexor tendon injury.
Clinically Relevant Anatomy
Following are the list of the muscle which is commonly injured-
- Flexor digitorum superficialis
- Flexor digitorum profundus
- Flexor pollicis longus
- Flexor carpi ulnaris
- Flexor carpi radialis
Flexors of the Fingers :
Flexor Digitorum Superficialis:
This muscle has a long linear origin but is thought to arise from two heads
Origin:
1. medial/ humeroulnar head: medial epicondyle of humerus, via common flexor tendon, the anterior part of the ulnar collateral ligament, and the sublime tubercle at the upper medial part of the coronoid process of the ulna.
2. lateral/radial head. : it is the upper two third of the anterior border of the radius.
Insertion:
palmar surface of the base of middle phalanges.
Action:
flex of the metacarpophalangeal joint and proximal interphalangeal joint
also contributes to flexion of the wrist.
Flexor Digitorum Profundus :
It lies deep to flexor digitorum superficialis on medial side of forearm.
Origin:
It originates from the medial side of the coronoid process of the ulna, the upper three-quarters of the anterior and medial surfaces of the ulna, and the medial, middle third of the adjacent interosseus membrane.
It also arises from the aponeurosis that attaches the flexor carpi ulnaris to the posterior border of the ulna.
Insertion:
the base of the palmar/volar surface of distal phalanges.
Action:
flexion of the distal interphalangeal joint
also aids in flexion of the proximal interphalangeal, metacarpophalangeal, and wrist joints, as it crosses many other joints during its course.
Flexor Pollicis Longus:
Lies on lateral side of flexor digitorum profundus.
Origin:
arises from the anterior surface of the radius, between the radial tuberosity above and pronator quadratus down, and the anterior surface of the coronoid process of the ulna.
Insertion:
palmar/volar surface of the bottom of the distal phalanx of the thumb.
Action:
a flex of the interphalangeal joint of the thumb
vital for all gripping exercises of the hand
also flexes the metacarpophalangeal joint of the thumb and wrist joint.
Pulley System in the Hand
The pulley system is an important anatomical structure in comprehending the tendon system in hand.
The annular pulley procedure’s function is to maintain the tendons close to the bone so that tendons don’t bowstring in involved flexion.
The cruciform pulley system is adjustable and collapsible to allow for digital flexion without deformation of the pulley method.
When treating people who had a tendon rehabilitation patients can occasionally present with bowstringing after a tendon repair.
Tendon Injury Zones
For finger flexors zones are as follows:
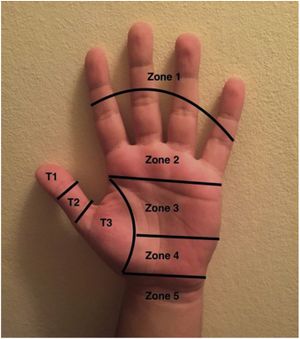
Zone I – it is distal to the muscle flexor digitorum superficialis (FDS)
Zone II – the FDS insertion to the distal portion of the A1 pulley
Zone III – from A1 pulley to the transverse carpal ligament
Zone IV – the carpal tunnel
Zone V – proximal to carpal tunnel
The thumb has its own zone distribution:
Zone I – distal to an interphalangeal joint (IP) in the thumb
Zone II – between metacarpophalangeal (MCP) and interphalangeal (IP) joints
Zone III – proximal to metacarpophalangeal (MCP) volar/palmar flexion crease
Mechanism of Injury
Flexor tendon injuries commonly result from volar/palmar lacerations. This can occur go along with neurovascular injury. Patients often present at a clinic as they have most likely sustained a significant injury.
Another mechanism of injury is a rupture rather than an injury, for example, the FDP tendon has been injured from its insertion at the distal phalanx – usually, this is caused by a closed mechanism of injury. This occurs as a result of forced extension throughout active flexion. This occurs in ball sports where a finger is forced into extension while it is being flexed or where a player grabs an opponent’s shirt (jersey finger) or in activities such as rock climbing.
Symptoms of Flexor tendon injury
The common sign of a flexor tendon injury include:
An open wound, like a cut, on the palm side of your hand, wrist, or forearm
An inability to bend one or more joints of your finger and hand.
Pain when you try to flex your finger
Tenderness through your finger on the palm side of your hand
insensibility in your fingertip
Diagnostic Procedures
Clinical tests:
- Flexor Digitorum Profundus (FDP) tendon – the patient is inadequate to flex the distal interphalangeal joint (DIP) in isolation
- Flexor Digitorum Superficialis (FDS) tendon – isolate the involved/affected finger and ask the patient to bend the proximal interphalangeal joint (PIP)
- Flexor Pollicis Longus tendon – bending the interphalangeal joint (IP) joint of the thumb in isolation
- Radiographs – may have associated fracture
- Ultrasound – used to assess suspected lacerations
- MRI
Outcome Measures
- Grip strength
- DASH
- Goniometer measurement
Treatment of Flexor tendon injury
Surgical Treatment
- Surgical Repair
It is needed for a cut or ruptured tendons. When a tendon ruptures, the ends differ as a result of the tension in the tendons. Sometimes this differential between the cut or ruptured ends of the tendon can be many centimeters. Surgical repair is required in order to regain the function that has been lost. it may be performed under painkiller or regional anesthetic (injection of local anesthetic at the shoulder).
During surgery, the gash is dilated so that the cut ends of the tendon can be discovered and held jointly with stitches. After the surgical repair, the hand and forearm are immobilized in a splint that is put over the dressing with the wrist and fingers in a slightly flexed position,
Post-Surgical Tendon Healing : 3 phases
- Inflammatory phase
it is the first phase
it lasts from day one to day seven post-operatively
in this stage, fibroblasts produce type III collagen, and macrophages help initiate healing and remodeling - Proliferative phase
It is the second phase
It runs from day 8 to about three weeks post-operatively
tissue modeling via large amounts of disorganized collagen happens during this stage
angiogenesis also happens during this stage. - Remodeling phase
this is the third stage
occurs up until about 18 months post-operatively
in this, tensile forces lead to tissue remodeling, and type III collagen is replaced with type I collagen
Post-Surgical Physiotherapy Treatment
Doctors need to have knowledge about the anatomy, the pulleys, the tendon injury zone, and the tendon healing stage as this will advise the treatment approach. For example, the tendon injury zone will speak about the splint design and the treatment protocol. The tendon healing duration and stage will influence the type of recovery exercises to commence with. For example, if a person is referred for treatment for 8 or 9 days after surgery and the patient has not had any treatment yet, the therapist would likely not start with active range of motion movement as the tendon is at its weakest from day 8 to day 21 post-operatively. Therapists need to be aware of the importance of the flexor mechanism in the functional utilization of the hand and how a flexor tendon injury can functionally impact a patient.
- Wound and Scar Management
After surgery wound management is the foremost step to address. The post-surgical laceration may be clothed with a basic silicone dressing (products such as Mepitel may be used). The finger is covered with breathable convenient gauze material. Another product that therapists may utilize contain Coban, but best, comfortable, clean, and a dry dressing is adequate as well.
Compression bandaging is used to control edema.
Once the injury is healed, scar management can commence. Silicone gel sheeting can be utilized on the scar or paper tapes or products for scar control like Fixomull. Scar massage can be done during treatment sessions and at home to stop adhesions.
- Patient Education
- Patient education is essential in the management of flexor tendon injuries.
- Patients need to be aware of the required precautions.
- The gash needs to be kept clean and dry.
- The splint needs to remain on 24 hours a day, 7 days a week.
- If the splint does need to come off, the patient must be educated about secure hand positioning.
- For a flexor injury, the patient needs to keep the fingers cupped with the wrist in neutral when the splint is off.
- This position does not put any stretch or pressure on the tendons.
- Later, weekly sessions until around 10 weeks post-surgery are done.
Orthoses
- FDP and FDS Tendon Repair
Forearm-based metacarpophalangeal joint (MCP) extension blocking splint with wrist in impartial and MCP’s in around 30° of flexion.
Zone I, II and III injury of flexor digitorum profundus and the flexor digitorum superficialis
This encourages the arc of flexion to be started by the long flexors, rather than the intrinsic
If therapists splint patients in a more remarkable degree of MCP joint flexion, flexion will be formed by the intrinsics rather than the long flexors.
Manchester short splint
hand-based splint
allows maximal wrist flexion, stops wrist extension at 45°
MCP joints – 30° flexion
IP joints – neutral
The use of the Manchester marks splint seems to enhance the digital arc of flexion in the early phase. This results in an improvement in DIP joint flexion and differential glide
Use of this type of splint displayed improved results, while still preserving repair integrity.
2. FPL Repair
Dorsal forearm-based orthosis
goes to the tip of the thumb up to three-quarters of the metacarpal size on the dorsum of the hand
wrist in neutral
thumb barely palmar-flexed into eased opposition with the MCP in about 20° of flexion and IP joint in neutral
The type of orthosis/splint that will be employed in a patient is often defined by the surgeon and therapists will need to discuss the appropriate choice of the splint with the surgeons that they work with.
Rehabilitation Exercises
The goal of the restoration exercises after a flexor tendon repair is to:
keep the tendons gliding and facilitate differential tendon glide
control early collagen deposition
facilitate the strengthening of the repair site
prevent adhesions, tendon gapping or re-rupture
supply patients with the best possible result after surgery
- Post-Operative Exercise FDS and FDP Repairs (first 6 weeks)
Place-and-hold Flexion Exercises
Place-and-hold flexion movements consist of the patient positioning the finger or fingers down in passive flexion and then holding it in active flexion. Multiple flexor tendon restoration protocols include place-and-hold flexion exercises. However, recent research shows that this provokes gapping and forces through the tendon when the tendon is abruptly required to activate after passive flexion. Hand therapists are moving away from this exercise and rather prescribe active flexion to a half fist with active extension into the back of the splint.
Active Flexion
Instead of place-and-hold drills, therapists are now using more developed protocols and are asking patients to perform active flexion to half a fist with active extension into the rear of the splint. Active flexion can begin from day one post-surgery. However, if the patient just sees the therapist after day 8 post-surgery and has had no restoration up until then, it is best not to start with active flexion exercises as the tendon is at its most powerless during this stage of healing.
Passive Flexion and Active Extension
The patient can perform passive flexion of the fingers and then vigorously extend the fingers into the rear of the splint.
A way to stop any PIP joint flexion sticking is to put a ruler down the back of the splint for the patient to actively extend against.
Exercise Frequency and Precautions
Patients should complete these exercises for 10 repetitions, five times a day.
Patients always do their activities with the splint, so that there is no chance of extending the fingers and rupturing or putting the tendon at risk.
- Post-Operative Exercises after 6 weeks
For all post-surgical tendon rehabilitation – the splints are modeled for 6 weeks
- After the initial 6 weeks, the patient is weaned out of the sling to start light usable use
- Gradually increase and grade the patient’s fully active and full passive range of motion
- Strengthening can usually begin at about 8 weeks post-surgery
- Strengthening activities can include activities such as: Squeezing Theraputty, Play-doh or a sponge in hot water
- Can move to wrist weights and Theraband if appropriate, for complete upper limb strengthening
- Once the patient is capable to return to his/her leisure activities and is capable to use the hand functionally with few limitations and pain is under management, the person can be released with a home program of continued stretching, scar management, and strengthening exercises.
Early Passive Flexion and Place-and-Hold
A total of four analyses examined and reached early passive flexion and place-and-hold protocols. Reasonable evidence was supplied that place-and-hold movements lead to very better total active motion at 8 weeks compared to passive flexion exercises. This was only the matter in patients with two-strand zone II repairs.
Dangers
- Rupture
- Infection
- Contraction
- Scar Adhesions
- Loss of sensation.
FAQs
What is a flexor tendon injury and repair?
Flexor tendons flex the finger or thumb into the palm. There are two flexor tendons for the individual finger and the thumb. The surgeon compared the ends of the cut tendon together and
placed specially designated stitches in the tendon. Following the repair, the voluntary movement of
the hand is limited. Active hand motion is limited to prevent the repaired tendon from
‘stretching’ and to permit scar tissue to develop to provide additional stability.Why do I have to wear the splint?
The splint is designed to minimize pull on the recently repaired flexor tendons. In the early phase of
the rehabilitation, even pulling or stretching the repaired tendon could result in poor motion. Usually,
your therapist will ask you to wear the splint at all duration, except for designated dressing
changes or hand exercises.What are the complications of the flexor tendon?
A considerably common complication is adhesion formation, which limits the active range of movement. Other complications contain joint contracture, tendon break, triggering, and pulley loss with tendon bowstringing. Less specific issues have quadriga, swan-neck malformation, and lumbrical plus deformation.