Common Peroneal Nerve Injury: Physiotherapy Treatment
Table of Contents
Introduction
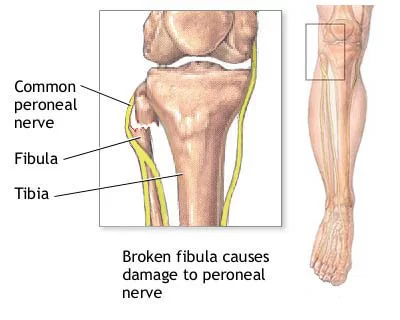
The Common peroneal nerve injury mostly occurs due to trauma and/or nerve compression, such as Knee dislocation, fracture below the Knee, or Compression of the peroneal nerve in the leg
Compression of the peroneal nerve also occurs due to nerve sheath tumors or nerve cysts
Because various medical conditions can cause peroneal nerve injury, it is important to be examined by a Doctor who can diagnose your condition and make a proper treatment plan accordingly.
Anatomy of Common Peroneal Nerve
The common peroneal nerve (common fibular nerve, external popliteal nerve, lateral popliteal nerve) is a nerve in the lower leg that provides sensation and motor function to parts of the lower leg. When damaged or compressed, it can cause foot drop.
The common peroneal nerve, about one-half the size of the tibial nerve, arises from the dorsal branches of the fourth and fifth lumbar and the first and second sacral nerves.
It descends obliquely along the lateral side of the popliteal fossa to the head of the fibula, close to the medial margin of the biceps femoris muscle. Where the common peroneal nerve winds around the head of the fibula, it is palpable.
It lies between the tendon of the biceps femoris and the lateral head of the gastrocnemius muscle, winds around the neck of the fibula, between the peroneus longus and the bone, and divides beneath the muscle into the superficial peroneal nerve and deep peroneal nerve.
A peroneal nerve injury (also called foot drop), is a peripheral nerve injury that affects a patient’s ability to lift the foot at the ankle. While foot drop injury is a neuromuscular disorder, it can also be a symptom of a more serious injury, such as a nerve compression or herniated disc.
Branches of nerve:
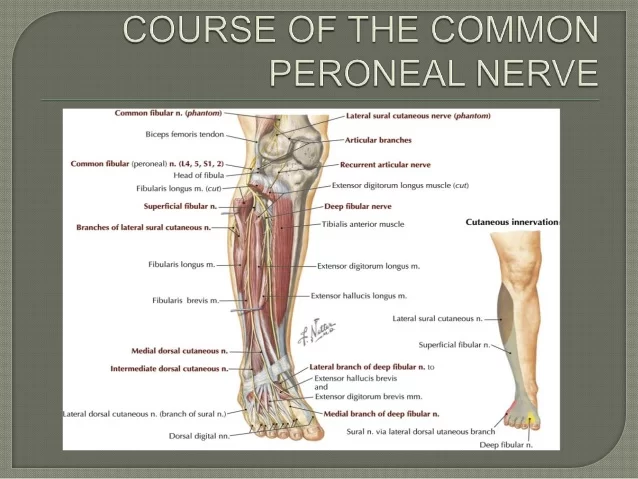
- Cutaneous branches
Lateral sural cutaneous nerve (lateral cutaneous nerve of calf) – supplies the skin of the upper two-thirds of the lateral side of the leg.
peroneal communicating nerve – it runs on the posterolateral aspect of the calf and joins the sural nerve.
2. Articular branches
Superior lateral genicular nerve – accompanies artery of the same name and lies above the lateral femoral condyle.
Inferior lateral genicular nerve – accompanies artery of the same name and lies just above the head of the fibula.
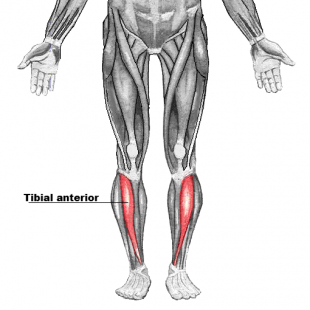
Recurrent genicular nerve – It arises from the point of division of the common peroneal nerve; then ascends anterior to the knee joint together with the anterior recurrent tibial artery to supply the knee joint and the tibialis anterior muscle.
3. Motor branches
There are no motor branches arising directly from common peroneal nerve
You can recognize foot drop by how it affects your gait. Someone with a foot drop may drag their toes along the ground when walking because they cannot lift the front of their foot with each step. In order to avoid dragging their toes or tripping they might lift their knee higher or swing their leg in a wide arc instead. This is called steppage gait and is a coping mechanism for foot drop issues.
FUNCTIONS:
The common peroneal nerve innervates the short head of the biceps femoris muscle via a motor branch that exits close to the gluteal cleft. The remainder of the peroneal-innervated muscles are innervated by its branches, the deep peroneal nerve, and the superficial peroneal nerve.
It provides sensory innervation to the skin over the upper third of the lateral aspect of the leg via the lateral cutaneous nerve of the calf. It gives the peroneal communicating nerve which joins the sural nerve in the midcalf.
CLINICAL SIGNIFICANCE:
Chronic peroneal neuropathy can result from, among other conditions, bed rest of long duration, hyperflexion of the knee, peripheral neuropathy, pressure in obstetric stirrups, and conditioning in ballet dancers.
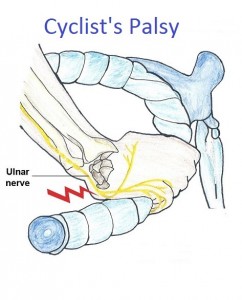
The most common cause is habitual leg crossing which compresses the common peroneal nerve as it crosses around the head of the fibula. Transient trauma to the nerve can result from a peroneal strike.
Damage to this nerve typically results in foot drop, where dorsiflexion of the foot is compromised and the foot drags (the toe points) during walking, and in sensory loss to the dorsal surface of the foot and portions of the anterior, lower-lateral leg. A common yoga kneeling exercise, the Vajrasana, has been linked to a variant called yoga foot drop.
Surgical procedures involving the nerve involve:
Peroneal nerve decompression: To surgically decompress the peroneal nerve, an incision is made over the neck of the fibula. Fascia surrounding the nerves to the lateral side of the leg is released.
Deep peroneal nerve decompression: In the surgical treatment of deep peroneal nerve entrapment in the foot, a ligament from the extensor digitorum brevis muscle that crosses over the deep peroneal nerve, putting pressure on it and causes pain, is released
Cause of Common Peroneal Nerve Injury:
Injury to the spinal cord.
Other underlying diseases such as Amyotrophic lateral sclerosis(ALS).
Multiple sclerosis (MS).
Parkinson’s disease.
Sometimes it is a complication of hip replacement surgery.
Knee or joint dislocation or fracture.
Herniated disc.
Trauma or injury to the knee.
Fracture of the fibula.
Use of tight plaster cast (or the long-term constriction) of the lower leg.
Crossing the leg regularly.
Regularly wearing high shoes.
Pressure to the knee from positions during deep sleep or coma.
Symptoms
Inability to point toes toward the body (dorsi flexion).
Pain.
Weakness.
Numbness (on the shin or top of the foot).
Loss of function of foot.
High-stepping walk (called steppage gait or footdrop gait).
Decreased sensation or tingling in the top of the foot or the outer part of the upper or lower leg.
Walking problems.
Loss of muscle mass because the nerves aren’t stimulating the muscles.
POSSIBLE COMPLICATIONS:
Decreased ability to walk.
Permanent decrease in sensation in the legs or feet.
Permanent weakness or paralysis in the legs or feet.
Side effects of medicines.
DIAGNOSIS:
A comprehensive clinical exam, including neurological exams.
Complete medical history.
Electrical testing.
Nerve conduction velocity(NCV) test.
X-rays.
High-resolution 3-T MRI.
Nerve ultrasound.
Electromyography.
How to prevent Common peroneal nerve injury?
Warm up and stretch properly before activity.
Maintain physical fitness.
Wear properly fitted and padded protective equipment.
Avoid crossing legs or putting long-term pressure on the back or side of the knee. Treat injuries to the leg or knee right away.
If a cast, splint, dressing, or other pressure on the lower leg causes a tight feeling or numbness, call your provider.
Prognosis:
Common peroneal nerve injury is often curable with non-surgical treatment. Often symptoms will go away on their own (spontaneously). Sometimes, surgery is needed to relieve pressure from the nerve.
Treatment of Common Peroneal Nerve Injury
Treatment first involves resting from any activities that cause the symptoms to get worse.
The use of ice and medicine may reduce pain and inflammation.
If ice is used, do not place it directly on the skin. Instead, place a towel in-between.
If there is weakness of the muscles, causing foot drop, bracing the ankle and foot may be needed.
It is important to perform strengthening and stretching exercises to maintain muscle strength.
These exercises may be completed at home or with a therapist.
If pain continues to get worse, despite treatment, or a cyst is present, surgery may be needed to relieve the pressure on the nerve.
If the pressure on the nerve is due to compartment syndrome, a fascial (sheet of connective tissue) release may need to be performed.
The earlier surgery is performed, the better your chances of full recovery.
MEDICATION:
If pain medicine is needed, nonsteroidal anti-inflammatory medicines (aspirin and ibuprofen), or other minor pain relievers (acetaminophen), are often advised.
Do not take pain medicine for 7 days before surgery.
PHYSIOTHERAPY TREATMENTS:
Goals of physical therapy intervention include minimizing edema, increasing neural mobility, and maintaining or increasing the strength and endurance of unaffected sites.
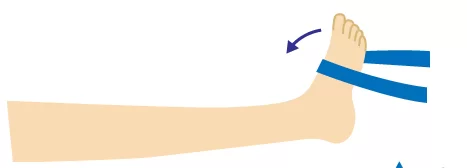
Range of motion exercise for ankle eversion.
Range of motion exercises for ankle inversion.
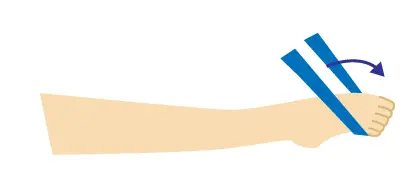
Range of motion exercise for ankle dorsiflexion, active assisted.
Stretching of calf and hamstring muscle.
Stretching of gastrocnemius – soleus muscle.
Strengthening exercises for dorsiflexors, ankle eversion and ankle inversion.
Modalities:
Cold therapy.
Electric stimulation.
Ultrasound.
Iontophoresis.
Ankle-foot orthosis.
Injury to the spinal cord.
Causes of Foot Drop
There are three main causes of the weakened nerves or muscles that lead to foot drop:
1: Nerve Injury. The peroneal nerve is the nerve that communicates to the muscles that lift the foot. Damage to the peroneal nerve is the most common cause of foot drop. The nerve wraps from the back of the knee to the front of the shin and sits closely to the surface, making it easy to damage. Damage to the peroneal nerve can be caused by sports injuries, hip or knee replacement surgery, a leg cast, childbirth or even crossing your legs.
2: Muscle Disorders. A condition that causes the muscles to slowly weaken or deteriorate can also cause foot drop. These disorders may include muscular dystrophy, amyotrophic lateral sclerosis (Lou Gehrig’s disease), and polio.
3: Brain or Spinal Disorders. Neurological conditions can also cause foot drop. Conditions may include stroke, multiple sclerosis (MS), cerebral palsy, and Charcot-Marie-Tooth disease.
How foot Drop is Treated?
Treatment for foot drop requires treating the underlying medical condition that caused it. In some cases, foot drop can be permanent, but many people are able to recover. There are a number of treatments that can help with foot drop:
1: Surgery
If your foot drop is caused by a pinched nerve or herniated disc then you will likely have surgery to treat it. Surgery may also be necessary to repair muscles or tendons if they are directly damaged and are causing foot drop. In severe or long-term cases, you might have surgery to fuse your ankle and foot bones and improve your gait.
2: Functional Electrical Stimulation
If your foot drop is being caused by damage to the peroneal nerve then Functional Electrical Stimulation may be an alternative to surgery. A small device can be worn or surgically implanted just below the knee that will stimulate the normal function of the nerve, causing the muscle to contract and the foot to lift while walking.
3: Braces or Ankle Foot Orthosis (AFO)
Wearing a brace or AFO that supports the foot in a normal position is a common treatment for foot drop. The device will stabilize your foot and ankle and hold the front part of the foot up when walking. While traditionally doctors have prescribed bulky stiff splints that go inside the shoe, the SaeboStep is a lightweight and cost-effective option that provides support outside the shoe.
4: Physical Therapy
Therapy to strengthen the foot, ankle, and lower leg muscles is the primary treatment for foot drop and will generally be prescribed in addition to the treatment options mentioned above. Stretching and range of motion exercises will also help prevent stiffness from developing in the heel.
Rehabilitation Exercises for Foot Drop
Specific exercises that strengthen the muscles in the foot, ankle, and lower leg can help improve the symptoms of foot drop in some cases. Exercises are important for improving range of motion, preventing injury, improving balance and gait, and preventing muscle stiffness.
When treating foot drop, you may work with a physical therapist who will help you get started strengthening your foot, leg, and ankle muscles. Rehabilitation for foot drop can be a slow process, so your physical therapist will likely recommend that you continue to do strengthening exercises at home on your own.
By being consistent about your exercises at home, you can maximize your chances of making a successful recovery from foot drop. Strengthening the weakened muscles will allow you to restore normal function and hopefully start walking normally again.
Like any exercise program, please consult your healthcare professional before you begin. Please stop immediately if any of the following exercises cause pain or harm to your body. It’s best to work with a trained professional for guidance and safety.
- Towel Stretch

Sit on the floor with both legs straight out in front of you. Loop a towel or exercise band around the affected foot and hold onto the ends with your hands. Pull the towel or band toward your body. Hold for 30 seconds. Then relax for 30 seconds. Repeat 3 times.
2. Toe to Heel Rocks
Stand in front of a table, chair, wall, or another sturdy object you can hold onto for support. Rock your weight forward and rise up onto your toes. Hold this position for 5 seconds. Next, rock your weight backward onto your heels and lift your toes off the ground. Hold for 5 seconds. Repeat the sequence 6 times.
3. Marble pickup

Sit in a chair with both feet flat on the floor. Place 20 marbles and a bowl on the floor in front of you. Using the toes of your affected foot, pick up each marble and place it in the bowl. Repeat until you have picked up all the marbles.
4 . Ankle Dorsiflexion
Sit on the floor with both legs straight out in front of you. Take a resistance band and anchor it to a stable chair or table leg. Wrap the loop of the band around the top of your affected foot. Slowly pull your toes towards you then return to your starting position. Repeat 10 times.
5-plantar-flexion:
Sit on the floor with both legs straight out in front of you. Take a resistance band and wrap it around the bottom of your foot. Hold both ends in your hands. Slowly point your toes then return to your starting position. Repeat 10 times.
slowly lower. Repeat 10 times
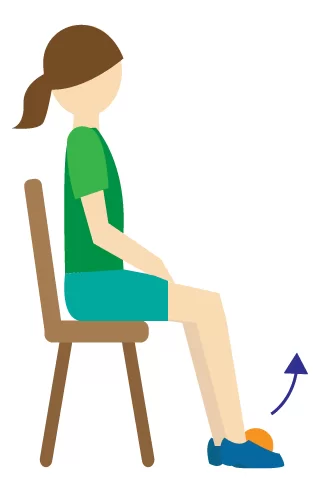
6. Ball Lift
Sit in a chair with both feet flat on the floor. Place a small round object on the floor in front of you (about the size of a tennis ball). Hold the object between your feet and slowly lift it by extending your legs. Hold for 5 seconds.
FAQ
Symptoms of peroneal nerve damage are:
Diminished feeling, tingling, or numbness in the outside portion of the upper or lower leg or the top of the foot.
Foot dropping (inability to keep the foot up)
“Slapping” gait (a manner of walking where the sound of each step is similar to a slapping one)
Walking causes toes to drag.
issues with walking.
weakness in the feet or ankles.
The lumbar nerve roots in the spine or the common peroneal nerve in the knee are the typical sites of involvement. More specifically, the deep branch is the cause of the loss of function when the peroneal nerve is affected.
A program of stretching, strengthening, mobilization, manipulation, and proprioceptive and balance exercises is part of physical therapy for common peroneal nerve injuries. Additionally, tape, ankle bracing, and/or ice may be used.
The most frequent nerve lesions in the lower leg are common peroneal nerve (CPN) injuries, which can have a variety of causes. Even while they usually heal on their own, there is a chance that the nerve will be permanently damaged.
Your healthcare professional will check your leg and inquire about your symptoms in order to identify a peroneal nerve damage. A variety of tests, including as imaging tests like an MRI, CT scan, or ultrasound, may also be used. A specialist MRI called magnetic resonance imaging (MR) neurography can help in diagnosis.
Your recovery period may vary depending on your age, underlying medical conditions, and the degree of your common peroneal nerve palsy. Nerve damage heal gradually, but symptoms go away right away. Up to six months may pass before full healing occurs.
Walking with a common peroneal nerve injury may be challenging, as it can cause weakness and instability in the lower leg and foot. The extent of impairment varies, but some individuals may experience difficulty walking or an altered gait.




2 Comments