Foot Drop: Cause, Symptoms, Treatment & Exercise
Table of Contents
Introduction of the Foot Drop
- Foot drop is sometimes called drop foot, which is a general term for difficulty in lifting the front part of the foot. If the person has a foot drop, the front of the foot might drag on the floor when they walk. Foot drop is not a disease. Rather, it is a sign of an underlying neurological, muscular, or even anatomical problem. Sometimes foot drop is temporary, still, it can be permanent. If the patient has a foot drop, they might need to wear the brace on the ankle and foot to hold the foot in the normal position.
- Foot drop is the gait abnormality in this the dropping of a forefoot that occurs because of weakness, irritation, or even damage to a deep fibular nerve (deep peroneal), including the sciatic nerve, or even paralysis of the muscles in an anterior portion of the lower leg. Foot drop is usually the symptom of the greater problem, not the disease in itself. Foot drop is mainly characterized by the inability or impaired ability to raise the toes or raise a foot from the ankle meaning dorsiflexion. It may be temporary or permanent, depending on the extent of muscle weakness or even paralysis and it can occur in one or both feet. In walking, the raised leg is slightly bent at a knee to prevent a foot from dragging along the floor.
- It is the abnormal walk that is mainly caused by the tendency of the front half of the foot to drop downwards as the patient walks along. The foot can catch on the ground as they swing the leg forwards to take a step. The walking gait of the foot drop may involve:
As the patient walks along, the injured foot (or feet) catches on the ground.
As a patient walks along he/she can lift a leg high to avoid the foot catching (high stepping gait). Individuals who do this often tend to walk on tiptoe on another side to equalize the sides.
As the patient walks they swing an injured leg out to the side to avoid it catching on the ground.
There are many grades of foot drop. These are measured from 0 to 5 depending on the degree of strength as well as movement there is in the muscles which lift the foot. 5 is normal strength and 0 is total paralysis as well. - Foot drop is a deceptively simple name for the potentially complex problem. This may be defined as the significant weakness of the ankle and the toe dorsiflexion. The foot, as well as ankle dorsiflexion, include the tibialis anterior, the extensor hallucis longus, and the extensor digitorum longus (EDL) muscles. These muscles assist the body clear the foot while the swing phase as well as controlling plantar flexion of the foot on heel strike.
Weakness in a described group of the muscles results in the equinovarus deformity. This is sometimes referred to as the steppage gait, owing to a patient tends to walk with the exaggerated flexion of the hip as well as knee to prevent the toes from catching on the floor while the swing phase.
Pathophysiology
- The causes of the foot drop, as for all causes of neurological lesions, could be approached using the localization-focused approach before etiologies are considered. Most of the time, this condition is the result of a neurological disorder, only rarely is a muscle diseased or even non-functional. The source of a neurological impairment may be central meaning spinal cord or even brain-related or peripheral meaning nerves located connecting from a spinal cord to the end-site muscle or sensory receptor.
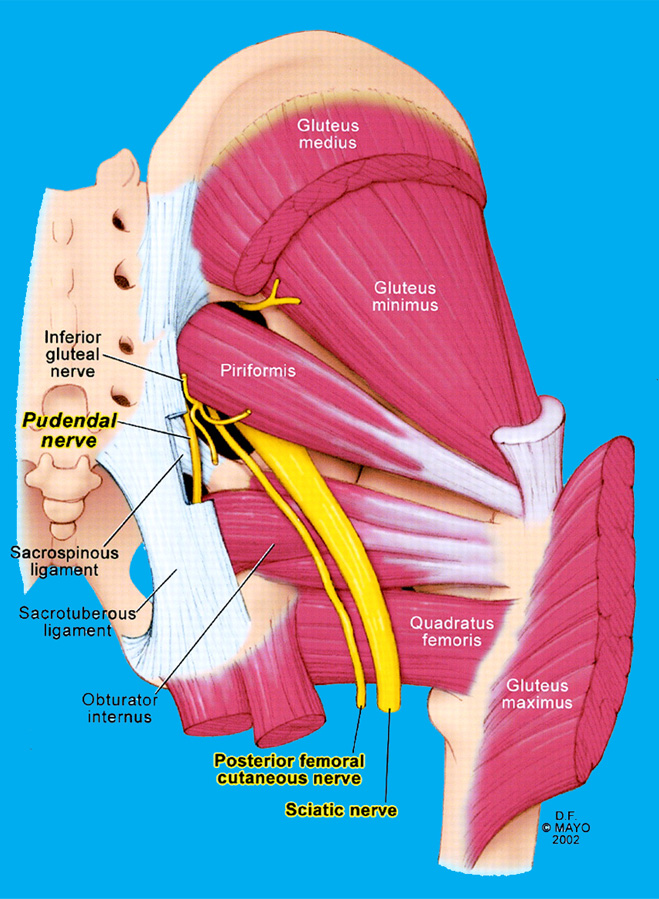
- This condition is rarely the result of the pathology involving the muscles or even bones that make up a lower leg. An anterior tibialis is a muscle that picks up the foot. Even though an anterior tibialis muscle plays a major role in dorsiflexion, this is helped by the fibularis tertius, extensor digitorum longus as well as the extensor hallucis longus muscles. If a drop foot is caused by a neurological disorder all of described these muscles can be affected owing to they are all innervated by a deep fibular (peroneal) nerve, that branches from the sciatic nerve. A sciatic nerve exits a lumbar plexus with its root arising from a fifth lumbar nerve space.
Occasionally, spasticity in these muscles opposite to the anterior tibialis, the gastrocnemius, and soleus as well, exists in the presence of the foot drop, making a pathology much more complex rather than foot drop. Isolated foot drop is mainly a flaccid condition. There are gradations of the weakness which can be seen with the foot drop, as follows according to the MRC grading system
0 = complete paralysis,
1 = flicker of the contraction,
2 = contraction with gravity eliminated alone,
3 = contraction against the gravity alone,
4 = contraction against gravity as well as some resistance.
5 = contraction against powerful resistance meaning normal power.
Causes of the foot drop
Foot drop is caused by weakness or even paralysis of the muscles involved in lifting a front part of the foot. It usually happens when there is a problem with the nerves in the lower spine, leg, or foot or the muscles of the leg and foot. Causes of the foot drop may include;
Neurological causes
- Nerve injuries
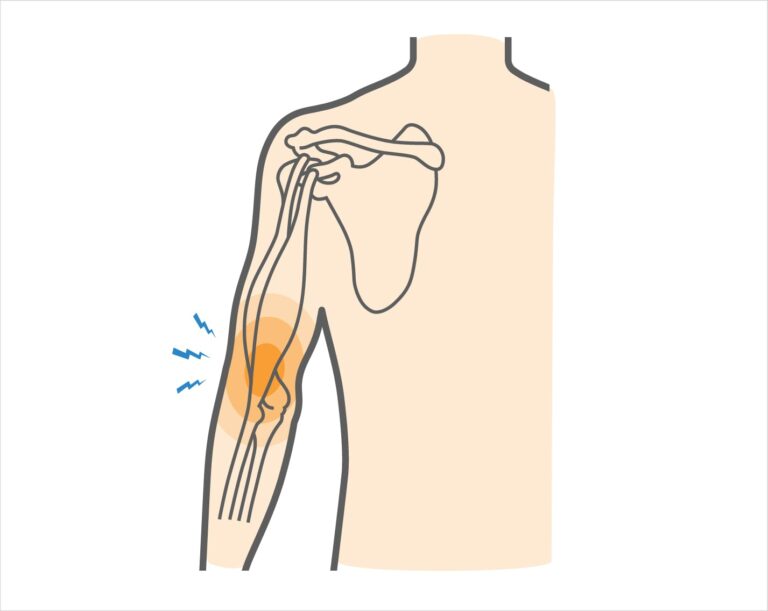
A most common cause of the foot drop is compression of the nerve in the leg which controls the muscles involved in lifting a foot (peroneal nerve). This nerve may also be injured while hip or knee replacement surgery, which can cause the foot drop. The nerve root injury “pinched nerve” in the spine can also cause the foot drop. Individuals who have diabetes are more susceptible to nerve disorders, which are associated with foot drops. Mainly, if the heel strikes the ground first as the foot lands, the dysfunction of a lower spinal nerve root(s) or even peripheral nerve(s) can be suspected. Neurological causes can include one or even more of the following: - Radiculopathy: The symptoms following nerve root irritation or even compression in a lumbar spine, for instance, radiculopathy of an L5 nerve root.
- Neuropathy: Damage to the peripheral nerve in a leg at any point along its path, for instance, neuropathy of a common peroneal nerve, deep peroneal nerve, or even the sciatic nerve.
- Lumbosacral plexopathy: Damage to the group of nerves (plexus) in a lumbar as well as the sacral spine.
Foot drop can also happen when the nerves in a leg and/or feet are damaged owing to systemic conditions or even genetic disorders. A few instances include diabetes, vasculitis (inflammation of the blood vessels), as well as hereditary neuropathy with liability to pressure palsies. Rarely, the tumor block blood vessel, or even bleeding in the brain can cause a foot drop.
Muscle or even nerve disorders cause
- Different forms of muscular dystrophy, the inherited disease that causes progressive muscle weakness, can contribute to the foot drop. Threfore, the patient can have other disorders, such as polio or Charcot-Marie-Tooth disease. The brain as well as spinal cord disorders
- Disorders that affect the spinal cord or even the brain such as amyotrophic lateral sclerosis (ALS), multiple sclerosis, or stroke may cause foot drops. If the toes strike first as the foot lands on the ground, the cause can be weakness or even paralysis of the pretibial, peroneal, or even hip flexor muscles.
Other causes include:
- Total or partial hip replacement
- Knee surgery
- Sciatic nerve damage
- Cauda equina syndrome. In this condition compression of the nerves in a tail of a spinal cord, usually caused by the ‘slipped’ disc or tumor)
- Diabetes with peripheral neuropathy
- Various types of stroke
- Transient ischaemic attack
- Multiple sclerosis
- Cerebral palsy
- Charcot-Marie-Tooth disease.
- Poliomyelitis
- Motor neuron disease
- Friedreich’s ataxia
- Brain tumor
- Adverse drug or even alcohol reaction.
- Patients with pain in the soles of their feet may walk with a high stepping gait that looks similar, still, the patient does not have the foot drop; they are lifting their feet for a different reason.
Signs and symptoms of the foot drop
- Foot drop is mainly characterized by steppage gait. During walking, individuals may suffer from the condition drag their toes along the floor or bending their knees to lift the foot higher as compared to usual to avoid the dragging. In this, the abnormal reduction in the extent to which the foot may be lifted off to a floor while the swing phase of normal walking. A swing phase refers to the part of a gait cycle where the front part of the foot lifts off before the heel presses down for the next step. This serves to raise the foot high enough to prevent the toe from dragging and prevent slapping. To accommodate the toe drop, the patient may use the characteristic tiptoe walk on an opposite leg, raising a thigh excessively, as if walking upstairs, while letting a toe drop. Other gaits such as the wide outward leg swing mainly to avoid lifting a thigh excessively or even to turn corners in an opposite direction of the affected limb can also indicate foot drop.
The patient with painful disorders of sensation (dysesthesia) of the soles of the foot can have a similar gait but does not have a foot drop. Due to the extreme pain evoked by even the slightest pressure on a foot, a patient walks as if walking barefoot on hot sand. - Inability to hold footwear: The feeling of loosening of footwear can cause discomfort and drag the injured foot during walking.
Tripping: Weakness in the muscles of the foot, as well as toes, can result in frequent tripping. - Falls: This is common to lose balance, stumble, as well as fall with a foot drop. Falls happen because of the inability to properly lift the front part of the foot and toes while walking.
- Circumduction gait: Sometimes, in order to avoid falls or even tripping, the circumduction walking pattern, where a leg remains straight as well as swings to a side in the semicircle to move forward may be attempted.
- Limp foot: An injured foot can flop away from a body, which may also be difficult to climb stairs.
- Numbness: Loss of sensation can happen on the front and/or outer side of a lower leg, and/or along with an upper part of the foot.
- Often unilateral: A foot drop typically affects one foot, especially when caused by the pinched nerve in the lower back or leg.7
- Decrease in muscle mass: Weakening of the muscles can cause muscle mass to decrease, especially when foot drop is caused by certain autoimmune conditions, namely multiple sclerosis.
- Romberg’s sign: There can be a loss of balance during standing without support as well as with the eyes closed.
- Foot drop symptoms based on specific nerve compression
- Foot drop can cause weakness with numbness and/or pain in specific areas of the foot as well as the leg based on the underlying compressed nerve. A few common examples are:
- L5 radiculopathy or lumbosacral plexopathy: A foot drop from compression of the L5 nerve root or even the group of nerves from a lumbar as well as sacral spine may cause: Weakness in moving the foot upward or even downward at an ankle joint, turning the foot to an outer and/or inner side at an ankle, moving a leg away from a body at a hip, as well as moving the thigh inward from a hip joint, pain in a lower back that radiates to a leg.
- Common peroneal injury or neuropathy: A foot drop from compression of a common peroneal nerve may cause: weakness in lifting an ankle joint upward and during turning the foot to an outer side of an ankle. Numbness in the front as well as the side of the lower leg and top of the foot
- Sciatic neuropathy: A foot drop from a compression of a sciatic nerve can cause: Weakness in moving an ankle joint upward or even downward, turning the foot to an outer and/or inner side at an ankle, and while bending a knee, pain and/or numbness in a back of a thigh, side of the leg, and upper part of the foot.
- Deep peroneal neuropathy: A foot drop from compression of the deep peroneal nerve may cause: Weakness in lifting an ankle joint upward. Numbness in the skin over a web between the first as well as second toes.
Gait cycle
- Drop foot or even foot drop are interchangeable terms that describe the abnormal neuromuscular disorder that affects a patient’s ability to raise the foot at an ankle. Drop foot is further characterized by the inability to point the toes toward a body (dorsiflexion) or even move the foot at an ankle inward or even outward. So, a normal gait cycle is affected by drop foot syndrome.
- The normal gait cycle is as follows:
- Swing phase(SP): A period of time when the foot is not in contact with a floor. In those cases where the foot never leaves a floor(foot drag), which can be defined as a phase when all portions of the foot are in forwarding movement.
- Initial contact (IC): A point in A gait cycle when the foot initially makes contact with a floor; this represents a starting of a stance phase.
This suggests the heel strike not be the term used in clinical gait analysis as in many circumstances initial contact is not made with a heel. - Terminal contact (TC): The point in the gait cycle when the foot leaves the ground, which represents the end of the stance phase or start of a swing phase. Also referred to as the foot off. Toe-off can not be used in situations where a toe is not the last part of the foot to leave the ground. The foot drop gait cycle requires more exaggerated phases.
- Foot drop SW: If the foot in the movement occurs to be an injured foot, there will be greater flexion at the knee to accommodate an inability to dorsiflex. This enhancement in the knee flexion will cause the stair-climbing motion.
- Foot drop IC: Initial contact of the foot that is in the movement will not have a normal heel-toe foot strike. Instead, the foot can either slap a floor or the entire foot can be planted on the ground all at once.
- Foot drop TC: Terminal contact that is observed in the patients that have drop foot is quite different. Since the patients tend to have weakness in an injured foot, they may not have the ability to support their body weight. Often, the walker or cane will be used to help in this aspect.
Drop Foot is an inability to dorsiflex, evert, or invert the foot. Therefore, when looking at a gait cycle, a part of the gait cycle that involves most dorsiflexion action would be Heel Contact of the foot at 10% of the Gait Cycle, as well as the entire swing phase, or 60- 100% of the Gait Cycle. This is known as the Gait Abnormalities.
Risk factors
- A peroneal nerve controls the muscles that lift the foot. This nerve runs near the surface of the skin on the side of the knee closest to the hand. Such activities that compress the nerve can increase the risk of foot drop. Examples include:
- Crossing the legs: Individuals who habitually cross their legs may compress a peroneal nerve on their uppermost leg.
- Prolonged kneeling: Occupations that mainly involve prolonged squatting or even kneeling, namely picking strawberries or laying floor tile may result in foot drops.
- Wearing a leg cast: Plaster casts that enclose the ankle as well as end just below the knee may exert pressure on the peroneal nerve.
Diagnosis
- The starting diagnosis often is made during routine physical examination. Such diagnosis may be confirmed by a medical professional, namely a physiatrist, neurologist, orthopedic surgeon, or even neurosurgeon. The person with the drop foot will have difficulty walking on the heels due to the patient will be unable to lift the front of the foot (balls as well as toes) off the floor. Thus, the simple test of asking a patient to dorsiflex can determine the diagnosis of a problem. This is measured on the 0-5 scale that observes mobility. The lowest point from 0 to 5 is 0, which will determine complete paralysis and the highest point is 5, which will determine complete mobility.
- There are other tests also present that may assist in determining the underlying etiology of the foot drop diagnosis. Such tests can include MRI, MRN, or EMG to assess the surrounding areas of damaged nerves as well as the damaged nerves themselves, respectively. The nerve which communicates to the muscles that lift the affected foot is a peroneal nerve. This nerve innervates the anterior muscles of a leg that are used while dorsiflexion of an ankle. The muscles that are used in plantar flexion are innervated by a tibial nerve as well as often develop tightness in the presence of a drop foot. The muscles that keep an ankle from supination (as from the ankle sprain) are also innervated by a peroneal nerve, and it is common to find a weakness in this area. Paraesthesia in a lower leg, particularly on the top of the foot as well as the ankle, also can accompany drop foot, even though it is not in all instances.
- Imaging tests
- This is sometimes caused by the overgrowth of a bone in a spinal canal or by the tumor or cyst pressing on a nerve in a knee or even spine.
- X-rays: Plain X-rays use a low level of radiation to visualize the soft tissue mass or the bone lesion that might be causing the symptoms.
- Ultrasound: This technology, uses sound waves to create images of the internal structures and may check for cysts or tumors on a nerve or show swelling on a nerve from compression.
- CT scan: This combines X-ray images taken from severe different angles to form cross-sectional views of the structures within a body.
Magnetic resonance imaging (MRI): This test uses radio waves as well as a strong magnetic field to create detailed images. MRI is mainly useful in visualizing soft tissue lesions which may be compressing the nerve. - Nerve tests: Electromyography (EMG), as well as nerve conduction studies, measure electrical activity in the muscles and nerves as well. These tests may be uncomfortable, but it is useful in determining the location of damage along the injured nerve.
Treatment
Treatment for a drop foot depends on the cause. If a cause is successfully treated, a foot drop might disappear. If a cause can not be treated, drop foot can be permanent.
Treatment for foot drop might include:
Medical treatment
- If painful paresthesias develop, the condition can sometimes be effectively managed with sympathetic blocks or even laparoscopic synovectomy. Alternative managements are amitriptyline, nortriptyline, duloxextine, pregabalin, as well as gabapentin. Local treatment with transdermal capsaicin or even diclofenac may also decrease symptoms. Even if there is significant pain, narcotic medications may be kept to a minimum.
- Erythropoietin is the naturally happening hormone that is approved by the US Food as well as Drug Administration for the anemia but has neuroprotective and, possibly, neurotrophic properties as well. The proposed mechanism of the action is antiapoptotic as well as anti-inflammatory, promoting cell survival.
Braces or splints or AFO(Ankle foot Orthosis)
The brace on the ankle as well as the foot or splint that fits into the shoe may help hold the foot in the normal position.
Splinting
- One way to enhance function while a foot drop resolves is the use of splints. The solid ankle-foot orthoses (AFO) or foot-up splint may be used to keep the foot in plantar-grade. This work to improve the amount of dorsiflexion the foot is held in while gait and can prevent falls as the toes do not get caught on the ground.
Specialized shoes
- Shoes fitted with spring-loaded braces may assist prevent the foot from dropping while walking. One type uses the cuff around an ankle, a spring above, and a hook in the shoelace area which connects to the spring and pulls the foot up during walking.
Ankle-foot orthoses (AFOs)

- These types of orthosis specialized L-shaped ankle splints. It simply holds the foot at 90° to a lower leg so that it can not dropdown. The simple as well as relatively inexpensive way to correct these issues is to wear the foot support brace that assists the patient to lift the foot. These dorsiflexions help AFOs (ankle-foot orthotics) come in many styles, starting from posterior leaf spring (PLS) AFOs made of plastic or even lightweight carbon fiber to bulkier foot drop boots which may be worn at night to soft foot drop braces that may be worn even when the patient is barefoot.
- One of the most popular products is the soft foot drop brace which can be worn with shoes or when the patient is shoeless. The common complaint with carbon fiber as well as a plastic ankle-foot orthosis(AFOs) is that it can dig into a leg and/or foot and can not be used with some shoes as well as pants owing to their bulkiness.
- The soft fabric of this brace will not dig in, plus its slim, innovative design means the patient will not have to size up in terms of shoes or even worry about the pants getting caught on a product. A foot drop strap, as well as an optional shoe tongue, insert turns many “normal” shoes into the “best” shoes for a drop foot. The patient can even wear this dynamic ankle-foot orthosis(AFO) barefoot or with sandals.
- A low-profile design gives the patient more flexibility as compared to some of the more rigid supports, which can assist a patient to maintain more muscle strength as well as flexibility that is so essential to the function of the foot. With that said, this sock-like thing that lifts the foot is not intended for rigorous athletic activity. If the patient looking for the foot drop brace for running, the patient will likely need the carbon fiber ankle-foot orthosis, possibly the hinged one. Another common request is a foot drop night brace which supports the foot as the patient is sleeping. Without the dorsiflexion night splint, the foot can flop to a side, straining other areas of the body as well as renewing an ankle and foot pain, burning, and tingling associated with neuropathy as well.
- This dorsiflexion night splint is specially designed to support an ankle as well as a foot at a 90-degree angle as the patient sleep. This foot, as well as an ankle brace, is far less bulky as compared to traditional night braces for a foot drop and it features a breathable, open heel design that enhances sleep quality.
- The patient can wear it whether he is a side, back, or stomach sleeper. And a medical-grade faster used to secure its highly adjustable straps is ten times stronger than compared to the standard fastener, so the patient does not have to worry about it coming loose while the night.
- If the patient would prefer a more traditional boot to prevent a foot drop at night (or during the day), he should consider buying this drop foot brace for sleeping. A rigid shell of a brace forms an “L” which supports the foot, with cushioning making it more comfortable against the skin. A front side of a dorsiflexion boot is pretty open, with the series of straps giving the patient a custom fit. Tread along with the bottom of an anti-foot-drop boot makes the patient less likely to trip on late-night trips to the bathroom.
Physiotherapy treatment
Electrical modalities
- Electrical stimulation: Electrical stimulation while walking can also help reduce the symptoms of foot drops. This management method is known as functional electrical stimulation (FES). The Small devices worn near a knee respond to the motion of a leg as well as send mild electrical stimuli to the muscle to help it move properly.
- TENS(Transcutaneous electrical nerve stimulation): It is a method of pain relief involving the use of a mild electrical current. A TENS machine is a small, battery-operated device that has leads connected with the sticky pads called electrodes.
- Wax therapy: This method mainly assists a patient with the reduction of pain.
Exercise
Passive range of motion exercise
- Passive dorsiflexion
To begin with, the therapist should tell a patient to take a comfortable position, such as lying on a bed with a knee straight as well as the foot should out of a bed. After that, a physical therapist cups the heel with one hand and places another hand on the bottom of the foot. Then, a clinician gently pushes the foot up so that the toes point toward the head of a patient. Perform it ten times in a session. Do three sessions in one day.

- Passive inversion
To embark, ask a patient to take a comfortable position, namely lying on a bed with the knee straight the foot should out of a bed. Then, a therapist cups the heel with one strong hand and places another hand on the bottom of the foot. After that, a therapist gently turns the foot inward, not allowing a leg to rotate. Perform it ten times per session. Do three sessions per day. - Passive eversion
To start with, a physical therapist should give a command to a patient to take a comfortable position, such as lying on a bed with the knee straight as well as the foot should out of the bed. After that, the clinician cups the heel with one strong hand as well as places another hand on the bottom of the foot. Then, a clinician gently turns the foot outward but does not allow a leg to rotate. Perform it ten times in one session. Do three sessions in one day. - Passive toe extension
To begin with, sit on a chair, as well as place the foot to be exercised across an opposite knee. After that, a patient place one hand on the heel and the other hand on the toes, then, move the toes up towards the shin of the tibia as long as comfortable. Do it ten times in one session. perform three sessions in one day. - Passive toe flexion
First of all, a physical therapist tells a patient to take a sitting position on a chair and put the foot to be exercised across an opposite knee. Next, a patient put one hand on the bottom of a heel and another hand on the toes, after that move the toes down towards the shin of the tibia as long as comfortable. Do it ten times in one session. Perform three sessions in one day.
Stretching exercises
- Achilles stretch
The Achilles stretch is a lot like the calf stretch the patient may already know how to do:
First of all, start by standing near the wall or another support, like a chair, with the hands-on a wall at the eye level. After that, place the affected leg a step behind the unaffected leg. Then, keep the affected leg’s heel on the ground as well as bend the injured knee until the patient feels the stretch in the affected leg.
Here’s the trick: Bend the back knee bent slightly to stretch the Achilles tendon.
Hold this stretch for 30 seconds, repeating three times per session per day. - Towel stretch
To do this:
To begin with, sit on the ground with the legs extended straight out in front of the face. Next, wrap the towel around the toes on both feet. After that, pull back slightly till the patient starts to feel the stretch at the very bottom of the feet as well as the back of the lower legs. Aim to hold this stretch for around thirty seconds. Repeat it three times per session. Do three sessions per day.

- Big toe stretch
Keeping a wide range of movement in a big toe is essential.
To do this exercise:
To begin with, tell the patient to sit up straight in the chair, with a foot flat on the ground. After that, bring the affected foot to rest on the unaffected thigh. Then, using the fingers, gently stretch a big toe up, down, as well as to the side. Next, keep a big toe in each position for thirty seconds. Repeat it three times per session. Do three sessions per day. - Band stretch
The patient can also use the band or strap to assist with stretches. As with a towel stretch, using a prop like this may assist deepen a stretch.
To do an inward towel stretch:
To embark, sit with the towel or band around the affected foot. Next, firmly hold each end of a towel with the patient’s hands. Then, slowly turn the ankle inward, like the patient is facing the sole of the foot to the uninjured foot. After that, pull up with the unaffected hand side of the towel to deepen a stretch. Stretch for 30 seconds per repetition. Do it three times per session. Do three sessions per day. - Standing calf stretch
To dial up the tension in the stretch, a patient may move to the standing position:
To begin with, stand facing a wall or other support, like a chair, with one foot in front of the patient by around 12 inches. Next, point the toes up. After that, the therapist tells the patient to slowly lean forward till the patient feels the stretch in the back of the lower leg. Hold this position for 30 seconds. Repeat this exercise three times per session. Do three sessions per day. - Standing soleus stretch
To start with, the therapist tells the patient to stand a few feet away from the wall or other support, with facing it. After that, place one leg in the back with the heel flat on the ground. Next, the other leg can come forward toward the support. Then, gently turn the foot on the affected leg inward toward the other foot, and then slightly bend the front knee into the support till the patient feels the stretch in the affected leg. Hold this stretch for thirty seconds. Do three repetitions per session. Do three sessions per day.

- Cross leg ankle stretch
To do this:
First of all, sit comfortably with the affected leg crossed over the unaffected knee. After that, hold the unaffected foot with the patient’s hands. Then, use the unaffected hand to bend the affected toes as well as the ankle downward, like the patient is pointing the toes. Next, the patient should feel this stretch on the front of the ankle and the foot. Hold this position for 30 seconds. Repeat this exercise three times per session. Do three sessions per day. - Chair pose
To embark with, the therapist should tell the patient to tell stand tall in tadasana. Inhale as a patient raise both arms overhead, with palms inward. Next, as the patient exhale, bend both of the knees slightly, working toward getting the thighs parallel with the floor. After that, the torso should make the right angle with the tops of the thighs. In the end, try to hold it for 30 seconds. Do three repetitions per session. Do three sessions per day.
Active-assisted ankle range of motion exercise
- Active-assisted dorsiflexion
First of all, tell a patient to take a comfortable position, such as lying on a bed with a knee straight as well as the foot should out of a bed. Then, a clinician cups a heel with one strong hand and places another hand on the bottom of the foot as well. After that, a physiotherapist gives an instruction to a patient that moves the foot upward as long as the patient can, and when a patient is not able to move the foot between the motion, a clinician helps a patient to reach the full range of the dorsiflexion. Hence, the toes move towards the face. Perform it ten times per session. Do three sessions per day. - Active-assisted inversion
To embark with, tell the patient to take a comfortable position, such as lying on a bed with the knee straight and the foot should be out of a bed. After that, a physical therapist cups an inner border with one strong hand and places another hand on the bottom of the foot. Then, a physical therapist gives a command to the patient that moves the foot inward as long as the patient can, and when the patient is not able to move the foot inward in between the movements, a clinician helps the patient to reach the full range of the movement. Perform it ten times in one session. Do three sessions in a day.

- Active-assisted eversion
First of all, tell a patient to take a comfortable position, namely lying on a bed with the knee straight as well as the foot should out of the bed. After that, a clinician cups an inner border with one strong hand as well as places another hand on the bottom of the foot. Next, a clinician gives a command to a patient that moves the foot outward as long as a patient can, and when a patient is not able to move the foot outward in between the action, a physical therapist helps a patient to reach the full range of the movement. Do it ten times in one session. Do three sessions per day. - Active assisted toe flexion
First of all, tell the patient to take a comfortable position, such as lying on a bed with a knee straight as well as the foot should out of a bed. After that, a clinician cups the toes with one strong hand and places another hand on the bottom of the foot. Next, a physical therapist gives a command to a patient to move the toes toward the ground as far as the patient can, and when a patient is not able to bend the toes in between the action, a physical therapist helps a patient to reach the full range of the toe movement. Do it ten times per session. Do three sessions in a day. - Active-assisted toe extension
To embark with, ask a patient to take a comfortable position, namely lying on a bed with a knee straight and the foot should out of a bed. Next, a physical therapist places one hand on the backside of the toes as well as places another hand on the bottom of the foot. After that, a clinician gives a command to the patient to move the toes upward meaning toward the face side as long as a patient can, and when a patient is not able to extend the toes in between the action, a clinician assists a patient to reach the full range of the toe extension movement. Do it ten times per session. Perform three sessions in one day.
Active range of motion exercises
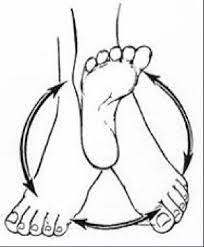
- Active ankle circles
This exercise can assist with the range of motion. The patient can do ankle circles from either sitting or even lying position:
To embark by turning an ankle around slowly in circles to the left, after that the right side. The patient can find this exercise easier to try drawing an alphabet in the air with the affected foot. Lead it with the big toe. Keep the movement small initially and focus on only using the foot and the ankle, not the whole leg. For circles, try doing ten in every direction with an injured foot. If the patient is doing the alphabet, complete three sessions of it on an injured foot per day.
- Toe extension
To do this exercise: Tell a patient to take the sit-up straight in a chair, with the feet flat on the ground. After that, place an affected foot on the normal thigh. Next, pull the toes upward toward an ankle. There should be a stretching feeling along with the bottom of the foot and the heel cord as well. Massaging the arch of the foot while stretching will assist ease tension and pain as well. Repeat this exercise ten times per session. Do three sessions in one day. - Toe flexion
First of all, tell the patient to take a sit-up straight on a chair, with the feet flat on the ground. Then, place the affected foot on the unaffected thigh. Next, move the toes down toward the ground. Do ten repetitions per session. Do three sessions per day. - Active dorsiflexion
First of all, ask a patient to take a comfortable position, namely lying on a bed. Next, a physical therapist should give a command to a patient to bend the foot toward the face side meaning upward as far as a patient can. Perform ten repetitions per session in one day. Do three sessions per day. - Active ankle inversion
To begin with, tell a patient to take a comfortable position, like lying on a bed. After that, a physical therapist should give a command to the patient to move the foot inside as far as the patient can. Repeat ten times per session in a set. Do three sessions per day. - Active ankle eversion
To begin with, tell the patient to take a comfortable position, like lying on the bed. Next, a clinician should give a command to a patient to move the foot outside as far as the patient can. Do ten repetitions per session. Do three sessions per day. - Hip adduction and abduction
Even though this exercise targets a leg, it is also useful for foot drop due to improved tone (stiffness) in a leg that may also affect the foot. Embark on this lower limb exercise in the seated position. After that, kick the injured leg inward toward the midline (hip adduction). Next, kick the injured leg outward (hip abduction), like the patient is kicking the ball to the side. Repeat this exercise ten times per session. Do three sessions in one day. - Toe raise
- It mainly works muscles in the lower leg, especially the tibialis anterior, which is located on the outer surface of a tibia, or even shin. This muscle is responsible for flexing the foot upward and extending the toes. The therapist should give the command to the patient that moves the toes upward actively as far as possible. Perform ten times per session. Do three sessions per day.
Strengthening
- Single leg stands
Standing on one foot is another best way to exercise ankle eversion as well as a challenge to ankle stability in general.
To embark with, the patient with foot drop who has enough strength as well as the balance can try to stand on their injured leg for ten seconds at a time. Be sure to hold onto the back of the chair for stability so that the patient does not fall. The risk of falling is greater in the patient with foot drop, so does skip this step. Do it ten times per session. Perform three sessions per day. - Toe to heel rocks
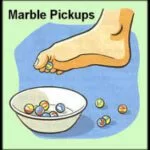
Stand in front of the table, chair, wall, or another stable object the patient can hold onto for support. Rock the weight forward as well as rise up onto the toes. Hold this position for ten seconds. After that, rock the weight backward onto the heels and lift the toes off the floor. Hold for ten seconds. Repeat the sequence ten times per session. Do three sessions per day. - Marble Pickup
First of all, the therapist should tell the patient to sit on the chair with both feet flat on the ground. Place 20 marbles as well as a bowl on the ground in front of the patient. Using the toes of the injured foot, pick up each marble as well as place it in a bowl. Repeat till the patient has picked up all the marbles.
- Ball lift
To begin with, sit on the chair with both feet flat on the ground. Place the small round object on the ground in front of the patient (about the size of a tennis ball). Hold an object between the feet and then slowly lift it by extending the legs. Hold for ten seconds then slowly lower. Repeat 10 times per session. Do three sessions per day. - Toe raise, point, and curl
This exercise mainly has three stages as well as it will assist in strengthening all parts of the feet and toes.
To do this exercise:
Take a sit-up straight position in the chair, with the feet flat on the ground. After that, keeping the toes on the ground, raise the heels. Then, stop when only the balls of the feet remain on the floor. Hold it ten seconds before lowering the heels.
For the second stage, raise the heels as well as point the toes so that only the tips of a big, as well as second toes, are touching the ground. Hold this position ten seconds before lowering.
For the third stage, raise the heels as well as curl the toes inward so that only the tips of the toes are touching the ground. Hold it ten seconds. Build flexibility and mobility by repeating each step ten times in one session. Do three sessions in one day. - Toe splay
Doing the toe splay exercise may improve control over the toe muscles. Individuals may do it on both feet at once or on alternate feet, mainly depending on which the patient finds more comfortable.
To do this exercise:
To begin with, sit in the straight-backed chair, with the feet gently resting on the ground. After that, spread the toes apart as long as possible without straining. Hold this position for ten seconds. Repeat this movement ten times per session. Do three sessions per day. Once the person has built up their strength, he can try looping the rubber band around the toes. This will provide resistance as well as make the exercise more challenging. - Toe curls
Doing toe curls builds up the flexor muscles of the toes as well as the feet, and improves overall strength.
To do this exercise:
To embark, sit up straight in the chair, with the feet flat on the ground. After that, lay a small towel on the ground in front of a body, with the short side facing the feet. Next, place the toes of one foot on the short side of the towel, and try to grasp the towel between the toes and pull it toward oneself as well. Repeat it ten times per session. Do three sessions per day. To make the exercise more challenging, try weighing down an opposite end of the towel with the object. - Sand walking
Walking barefoot on sand is the best way to stretch as well as strengthen the feet and calves. This is the best exercise in general due to sand’s soft texture makes walking more physically demanding.
To do this exercise:
To begin with, head to the beach, a desert, a volleyball court, or even any other location with sand. Remove the shoes as well as socks. Walk as far as possible. Try improving the distance slowly over time to avoid overexerting the muscles in the feet and calves as well. - Golf ball roll
Rolling the golf ball under the foot may assist in relieving discomfort in an arch as well as ease pain associated with plantar fasciitis.
To do this exercise:
First of all, sit up straight in the chair, with the feet flat on the ground. After that, place the golf ball or another small, hardball on the ground next to the feet. Then, lay one foot on a ball as well as move it around, pressing down as hard as is comfortable. Continue for ten seconds. A frozen bottle of water may be a soothing alternative if not suitable the ball is available. - Seated ball lift
To start with, tell the patient to sit on the chair with the feet flat on the ground. After that, place the small ball (e.g., a tennis ball) on the ground in front of the patient. Grab the ball using both the feet as well as slowly extend the legs to lift it. Hold for ten seconds, lower back to the floor. Repeat 10 times per session. Do three sessions per day. - Toe-to-heel rocks
Rock the weight forward to rise onto the toes as well as hold the position for ten seconds. After that, rock the weight backward and lift the toes off the floor and hold for ten seconds. Repeat ten times per session. Do three sessions per day. For more of the challenge, the patient can do this standing on one leg. The patient may want to do it near the wall or with the chair or counter in front of the therapist so the physical therapist can hold on for added support. - Dorsiflexors strengthen with the band
To begin with, the therapist tells a patient to sit on a chair and tie the theraband around a stable surface that would not move, such as a heavy table. Then, the therapist gives the command to the patient that extends the lower leg and wraps the other end of a band around the top of the foot. After that, do flexion of the foot, with the use of the theraband resisting the movement. Repeat ten times in one session. Do three sessions in one day for strengthening. - Invertors strengthen with the use of the band
To begin with, tie a band around the leg of the chair or with the table on the same side of the affected foot. After that, wrap another end of the band around the inside of the injured foot. Next, the therapist gives the command to the patient and then tries to turn the foot inside. Do it ten times per session. Do three sessions in one day. - Everson strengthening exercise with the use of the band
To embark, the therapist tells the patient to take a comfortable position, such as sitting on the chair, then tie a theraband on the leg of the chair opposite to the injured foot. Next, wrap another end around the outside of the injured foot. After that, a physical therapist should give a command to a patient that tries to turn the foot outside. Repeat it ten times per session. Do three sessions in one day.
Gait Training
- Gait signifies the way the person walks. The gait abnormality is the deviation from normal walking.
- Gait training is mainly recommended for those patients with significant gait problems. This treatment assists the patient in walking. more efficiently as well as improve stability by incorporating different strength and balance exercises as well. At times, gait training requires the use of walkers, canes, and parallel bars to safeguard a patient. The gait belt is the assistive device used to assist the patient to maintain balance while training.
Home exercise
- Passive dorsiflexion with the use of a towel or belt at home
First of all, a physical therapist tells a patient to sit with the leg extended and knee straight. After that, place the towel or belt around the ball of the foot. Next, hold each end of a towel in a clinician’s hands, and pull back with the towel so that the foot moves toward the face. A patient should feel a stretch in the calf and the hamstring muscles. Do ten repetitions per session. Do two sessions per day at home. - Passive ankle inversion with the use of a towel or belt at home
To begin with, a clinician tells a patient to sit with the leg extended and the knee straight. Next, place the towel or belt around a ball of the foot, after hold each end of a towel in the patient’s hands, and move the foot inward passively. Do it ten times in one session. Perform three sessions in one day. - Passive ankle eversion with the use of a towel or belt at home
To start with, a physical therapist tells a patient to sit with the leg extended and the knee straight as well. After that, place the towel or the belt around a ball of the foot, then hold each end of the towel in a physical therapist’s hands, as well as move the foot outward passively. Do it ten times in one session. Perform three sessions per day. - Passive plantar flexion with the use of a towel or belt at home
To embark, the therapist tells the patient to sit with the leg extended and the knee straight. Next, place a towel or belt around a ball of the foot. After that, hold each end of the towel in a physical therapist’s hands and pull back with a towel so that the foot moves toward the face. The patient should feel the stretch in the calf as well as the hamstring muscles. Do ten repetitions in one session. Do two sessions in one day at home. - Passive toe extension against the step at home
First of all, place the toes against the bottom of the wall/step resting a heel on the ground. Then, gently lean into a wall putting pressure through the toes, as well as pushing them back towards a shin of the tibia, but do not hold this position. Do it ten times in one session. Do three sessions in one day.



4 Comments