Cervicalgia
Table of Contents
What is Cervicalgia?
- Two-thirds of people suffer from cervicalgia, often known as neck pain, a prevalent condition.
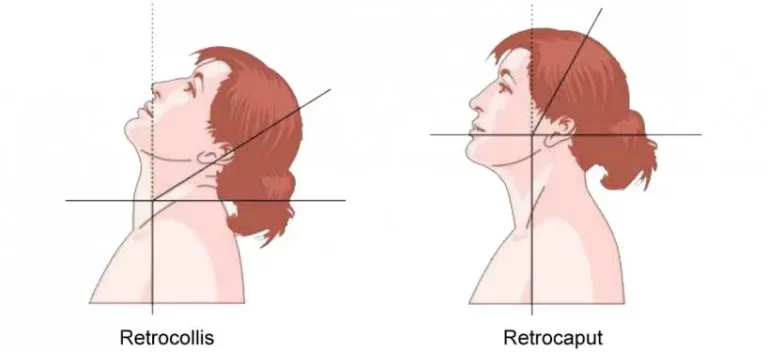
- Cervicalgia is neck pain. The bones of the neck form the cervical spine—this is the area that continues from the first spinal vertebra through the seventh. The first and seventh vertebrae of the spine are situated near the base of the neck and roughly at the level of your ears, respectively.
- Neck pain, also called cervicalgia, is a pain in or around the cervical spine beneath the head. Neck pain is a common symptom of cervical spine injuries and medical conditions.
- The neck, known as the cervical spine, is assigned to protect the spinal cord and support the head while permitting good movement.
- The cervical spine is made of a structure of bones, nerves, discs, muscles, ligaments, and muscle tendons, which allow the neck to be protected while keeping flexible.
- This capacity to be flexible also makes the neck structure unprotected from damage, especially given that it is continuously under pressure from keeping the head upright.
- Some movements put either gradual or sudden pressure on the neck, and the resulting strain can cause discomfort. When the injury only occurs in the neck area and not in other areas, such as in the shoulder or lower back, it’s called cervicalgia.
- Cervicalgia, or neck pain, can occur in any part of the neck, from the bottom of your head to the top of your shoulders. It can expand to the upper back or arms and may restrict how much you can move your head and neck.
Anatomy:
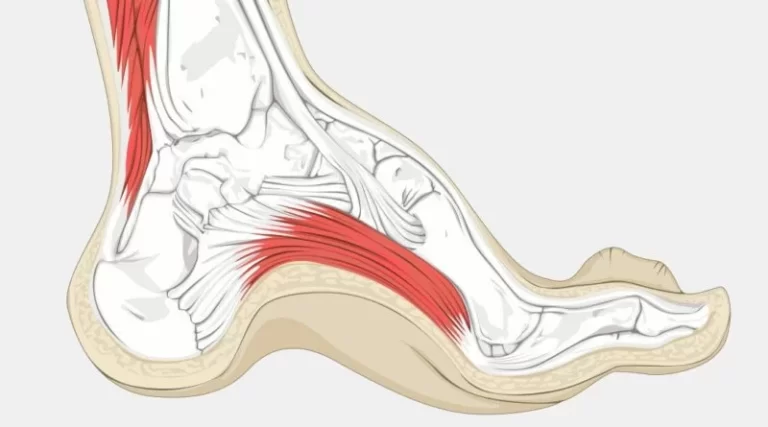
- Bones and Joints-
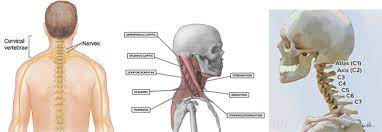
- The neck involves 7 bones C1-C7. Osteoarthritis, which occurs when the bones rub against one another in the joints and results in pain and stiffness, is the most frequent type of neck discomfort brought on by bone-related issues. Facet joints, which are small connections between vertebrae, connect these bones.
- Muscles, Tendons, and Ligaments-
- The movements in the neck are made possible by muscles like the sternocleidomastoid and trapezius. The most common pain produced by these parts is a neck muscle strain which affects the cervical muscles and tendons or a sprain which affects the ligaments, both involving overstressed or tearing of these structures.
- Nerves-
- Depending on the spinal level at which they are located, the cervical spine nerves give the head, neck, and upper sections of the body functional control and sensations. There are 8 cervical nerves: C1, C2, and C3 help to control the head and neck, including neck flexion, extension, and lateral flexion movements. C4 aids in controlling shoulder shrugs and supplies the diaphragm, whereas C5 controls the deltoids and biceps. C6 helps to control the wrist extensors and elbow flexion, C7 helps control the elbow extensor and wrist extensors, and C8 controls the movement of the hands, such as finger flexion. Pain can be caused by nerve root compression or irritation and sensation such as tingling is frequently felt in the upper extremities aiding identification of the damaged nerve.
Causes of Cervicalgia:
There are many different causes of cervicalgia. The most common causes include as following:
- Poor or bad posture or long periods with the neck at an awkward angle, such as when working at a computer desk, work with head down position.
- Whiplash injury or an impact sports injury involves a sudden neck movement.
- Long-term stress causes the holding of neck and shoulder muscles, leading to a strain on the neck muscles.
- Arthritis or osteoporosis, which is a bone condition that is more common in older people, Old age people is more prone to cervicalgia.
- Meningitis is a condition that affects the spine, and many other diseases or conditions such as spinal infections cause cervicalgia.
- Certain postural abnormalities like kyphosis affect posture as follows that strain the neck. Kyphosis can also lead to cervicalgia.
- Sports that promote pressure, can occur from posture, such as cycling, or certain bodybuilding programs that build up chest muscles more than the back muscles so that the shoulders are forwarded and rounded, putting pressure on the neck. It causes cervicalgia.
- Worry or stress can cause headaches.
Symptoms of Cervicalgia:
Mostly it presents with pain in the neck area, which can either be a sharp, stabbing pain or a dull, insistent pain.
The intensity of the pain will vary depending on the level of the injury, and mostly mild discomfort in most cases.
Other symptoms of cervicalgia can include:
- Pain in the neck and cervical area
- Stiffness in the neck:
- The neck muscles become tight. Neck stiffness can make it difficult to move the neck or painful neck movement.
- Tightness in the upper back
- Numbness or tingling sensation in the upper back or arm
- Weakness in arm
- Muscle spasm:
- Cervical paraspinal muscle and Trapezius muscle spasms are common in neck pain, A spasm is a sudden, strong, involuntary contraction of muscles. The muscles feel painful and knotted.
- Reduce neck movement
- Neck soreness
- Tenderness in the cervical area
- Swelling,
- Headaches, dizziness, nausea
Risk factors for Cervicalgia:
- Poor posture, neuromuscular disorders, autoimmune diseases, age, sports activities, poor sleeping position, psychological conditions such as anxiety, depression, workload, sedentary lifestyle
- Although certain occupations like computer workers, laborers, and health care workers, have a higher incidence of neck pain.
Differential Diagnosis:
Neck pain may originate from any of the neck’s structures, including its vascular, nerve, muscular, and skeletal systems, or it may refer to another area of the body.
Major and serious causes of neck pain include:
- Carotid artery dissection
- Referred pain from the acute coronary syndrome
- Head and neck cancer
- Infections, including:
- Meningitis
- Retropharyngeal abscess
- Epiglottitis
- Spinal disc herniation – protrusion or disc bulging
- Spondylosis – degenerative arthritis or osteophytes
- Cervical Spinal stenosis – space narrowing in the spinal canal
More standard and minor neck pain causes include:
- Stress – physical and emotional stress:
- Prolonged poor postures – many people fall asleep on sofas and chairs and wake up with sore necks.
- Minor injuries and falls – whiplash injuries from car accidents, sporting events, and day-to-day injuries that are minor.
- Referred pain – mostly from cervical and upper back problems
- Overuse of muscle strain – is one of the most common causes
- Pinched nerve
Although the causes are various, most are easily cured by either professional help or using self-help advice and techniques.
More common causes can include Poor sleeping posture, torticollis, head injury, rheumatoid arthritis, Carotidynia, congenital cervical rib, mononucleosis, certain cancers, ankylosing spondylitis, cervical spine fracture, esophageal trauma, subarachnoid hemorrhage, lymphadenitis, thyroid, and tracheal trauma.
How to Diagnose Cervicalgia?
- Medical history: If the patient has any medical history relevant to symptoms such as accident, or any injury.
- Physical examination: By palpating and measuring the range of motion of the neck. Ask to do neck movements and see if the pain increased. Check whether any neurological symptoms are present or not. such as tingling or numbness and weakness in the shoulder, arm, and hands. Perform special tests for proper diagnosis.
- X-rays: These show which areas in your neck (cervical vertebrae) where your nerve root or spinal cord may be compressed by degenerative changes or any other conditions.
- CT scan: It shows cross-sectional views of the cervical spinal structures of your neck.
- MRI: It creates detailed images of bones and soft tissues, including the spinal cord and the nerves from the spinal cord.
- EMG/ NCV: If the pain radiates to the arm then the doctor suggests EMG/NCV study to diagnose any nerve compression at the cervical level.
- Blood tests: For diagnosing Rheumatoid or infectious conditions that might be causing your neck pain.
Medical Treatment in Cervicalgia:-
- Commonly doctors prescribe Pain reliever Analgesics medicine (NSAIDs) eg. aceclofenac/diclofenac and Muscle relaxants eg. cyclobenzaprine to relieve muscle aches, Pain reliever Gels are also useful.
- Analgesics: Mild pain is often relieved with aceclofenac
- Nonsteroidal anti-inflammatory drugs (NSAIDs): eg. Aceclofenac, Diclofenac. They help in reducing neck pain, muscle spasms, and swelling.
- Oral corticosteroids: In severe cases of neck pain – oral corticosteroids can help relieve pain by reducing symptoms.
- Muscle relaxants: In case of muscles severe spasms eg. cyclobenzaprine or carisoprodol can be used.
Treatment for cervicalgia:
- The management of cervicalgia will vary depending on the condition of the patient. In the majority of cases, it can be managed at home.
- Cervicalgia will commonly relieve within 2 to 3 weeks. People should see a doctor if the pain lasts longer than 3 weeks, or immediately if the pain occurred by a direct injury.
- It is essential to avoid any heavy activities which cause neck pain, such as cycling, and long time computer work. Take a rest as much as possible. If the injury occurred from a lousy posture, it is essential to notice this immediately and improve it.
Different methods can be taken to treat cervicalgia at home:
- Ice therapy:
- Pain can be relieved by applying an ice pack to the affected part for up to 20 minutes 2 to 3 times a day.
- This can help to reduce swelling brought on by a neck injury.
- Heat therapy:
- It can also be applied to improve healing, such as through a hot shower or warm towel and hot packs.
- Medications:
- Such as anti-inflammatories or painkillers, can be helpful to treat cervicalgia.
- Massage:
- Deep massage techniques such as effleurage, and kneading to the localized areas will help to increase blood flow, encourage healing, and induce relaxation
- Cervical Collar:
- It supports the neck and the head, restricts movement, and reduces pressure from the area.
- Stretching exercises:
- Neck muscle stretching helps to maintain or increase the range of motion and improves the cervical joints’ flexibility.
If it can not be relieved in a couple of weeks, more serious treatment will be necessary, including a physiotherapy program or surgery to reduce discomfort.
It is also possible for cervicalgia to be a sign of a more concerning condition, such as a spinal infection.
Medical treatment must be looked to immediately if other symptoms develop, such as feelings of numbness or shooting pains in the arms. These symptoms may signal a bigger problem that needs urgent intervention.
Acute cervicalgia:
Acute cervicalgia with mobility deficits can be managed in different interventions including Neck range of motion exercises, scapulothoracic, and upper limb strengthening, isometrics, and cervical manipulation and/or mobilization (AP glide of the cervical spine).
Goals:
Reduce pain
Control inflammation
Reduce muscle spasm
Improve ROM of cervical
Reduce stiffness
Cervical collar:
Sometimes cervical collars apply to relieve strain on the neck muscle. A cervical collar may provide momentary pain relief from cervical spondylosis, an age-related disorder brought on by the deterioration of the cartilage and bones in the neck. general stiffness or soreness in the neck.
Pain management:
Cold compress:
Try to reduce both pain and inflammation by applying a cold or ice pack or ice wrapped in a towel to the neck. You can apply it to the area for up to 10 minutes a few times a day.
Follow up with a warm compress:
You can also alternate cold therapy with heat. With heat, its working eases muscle tension and pain. You can take a warm shower or heating pad on your neck. Again, apply it for up to 10 to 15 minutes.
The modality for pain management:
Transcutaneous electrical nerve stimulation (TENS) is useful to reduce pain in cervicalgia patients.
To reduce muscle spasms:
Deep massage techniques such as effleurage, kneading, and friction to the localized areas effectively reduce the spasm and pain and induce relaxation.
Stretching and gentle massage may help to stop muscle spasms. Icing or applying a heat pack may also help to reduce muscle spasms.
Postural correction and ergonomic advice:
Certain daily activities might be more painful for the neck, such as working on the computer for a long time, writing for long hours, work with a forward head. Alter this certain activity will usually reduce the pain. Use a proper size pillow during sleep. Take 5-minute rest between working hours. For the great majority of individuals with cervical pain, ergonomics is essential. Bad posture also accelerates degenerative changes.
The correct posture of the neck during working is important, to avoid overstress. straight neck with the chin tucked in is the ideal posture. Ergonomic advice can prevent recurrent neck pain.
Educate the patient on correct ergonomics to prevent common neck pain.
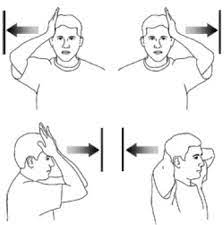
Cervical ROM exercise:
- Neck flexion
- extension
- rotation
- side flexion
Stretching exercise:
Straighten your back and keep your head level with your shoulders. Until you experience a stretch in the side of your neck and shoulder, slowly move your head to the right. Once you’ve stretched for 15–30 seconds, carefully move your head forward once more. Repeat on your left side.
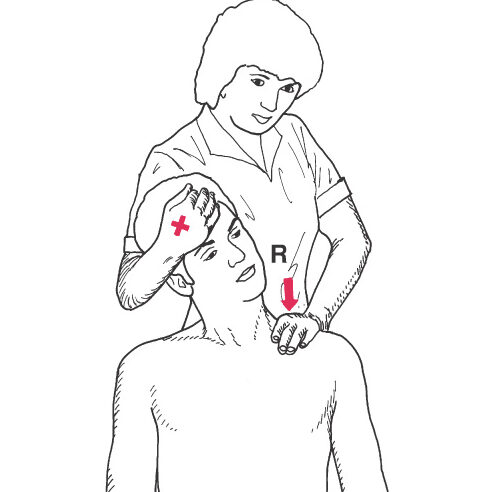
Isometric exercises: Self-Resistance
The intensity of the isometric exercises depends upon the patient’s forbearance and symptoms.
Patient Position and Procedure Sitting position
- Flexion: The person places both hands on the forehead and squeezes the tops of the hands together. that time movement is not allowed.
- Lateral flexion: Places one hand opposite the side to perform the movement and tries to reach the head toward the shoulder but the movement isn’t allowed.
- Extension: With both hands, the patient applies pressure on the back of the head, just below the crown.
- Rotation: Without allowing movement, the patient presses one hand against the area slightly above and to the side of the eye and executes a head turn to see over the shoulder.
Home exercise program (HEP): a single session consisting of early advice, exercise prescription, and education; along with strength and endurance with/without coordination exercises.
It has been found that an effective home exercise program has a strong correlation with reduced cervicalgia, increased motion, decreased disability, and improved QoL. Specifically, home exercise programs are more effective when they utilized self-mobilization techniques, strengthening exercises, and endurance exercises, and when the HEPs were designed to address a specific spinal level.
Patients who are showing symptoms of progressing towards chronicity or delayed rehabilitation outcomes should be identified and observed as early as possible, to provide them with a more intensive rehabilitation and an early pain education program.
Acute Headache management:
An emphasis should be placed on mobilization for managing acute cervicalgia with headaches.
Active exercises should be provided along with supervised instruction to be given by the therapist
Further, C1-C2 self-sustained natural apophyseal glide exercises should also be provided to be done independently.
Subacute Cervicalgia:
- For subacute management of cervicalgia with mobility impairment the following has been advised:
- Neck and shoulder girdle strengthening exercises.
- Chin tuck exercises,
- Acute mobility exercises
- Isometric exercise of the neck
- Thoracic manipulation, cervical manipulation, or cervical mobilization.
Subacute cervicalgia with headaches can also be managed with importance on mobilization, both independently and passively employed by a therapist.
This is to include:
cervical manipulation and mobilization:
C1–2 self-SNAG exercise and C1-2 SNAG rotation exercises
Chronic Cervicalgia:
Chronic cervicalgia with mobility loss benefits more from multiple management techniques, including thoracic manipulation and cervical manipulation or mobilization; all the mixed exercises for cervical and scapulothoracic regions: neuromuscular exercise (e.g. coordination, proprioception, and postural training), endurance training, aerobic conditioning exercises, stretching, strengthening, and cognitive-affective elements; or manual traction.
Dry needling is also used as an intervention in cervicalgia. It has been shown to be effective on pain, mechanical hyperalgesia, neck movements, neck muscle strength, and perceived neck disability.
LASER therapy provides relief from chronic cervicalgia for 3-6 months, without any serious side effects or complications.
Further, patient education should be provided in order to recommend an active lifestyle and direction to the cognitive and affective factors – e.g. help to arrange a suitable weekly activity program.
In the end, neck, shoulder girdle, and trunk endurance exercises should be used – e.g. plank, side plank, shoulder shrugs, etc.
Exercises:
The type of exercise is to be planned according to the patient’s needs, abilities, and comfort.
Relaxed passive movements:
Neck Flexion:
The patient stands straight or sits on the chair, bend the head forward, and holds for 10 to 15 seconds before releasing to neutral. Repeat this 3 – 5 times.
Lateral Flexion:
The patient stands straight or sits on the chair, bend the head to the side, and holds for 10 to 15 seconds before releasing to neutral. Repeat this 3 – 5 times.
Chin Tuck:
The patient Lies on the floor with a towel rolled up beneath his neck in a neutral position. The back of your head should rest on the floor.
Create a double chin by raising your chin slowly towards your chest. Hold for 1 to 5 seconds, then let your neck naturally relax for 5 to 10 seconds. 8–12 times should be done in this manner.
Neck rotations:
Turn your head from left to right while standing upright or when seated on a sturdy chair. Hold the left and right sides of your head for 15 to 30 seconds each, then alternate between the two sides two to four times.
Stretching exercises:
Stretching increases flexibility in the cervical joints and aids in maintaining or extending the range of motion.
Side bending stretch-
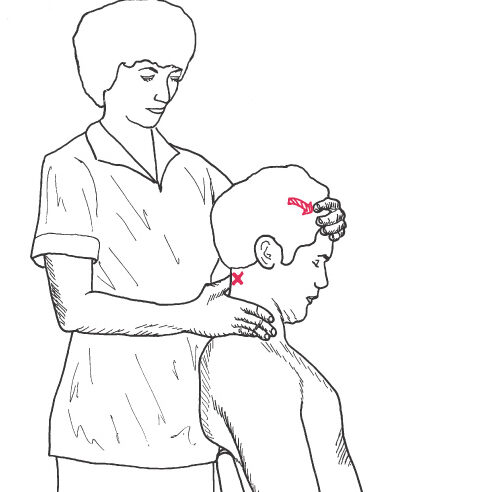
Manual stretching exercise:
In a sitting position, the patient does a chin tuck followed by side bends as a manual stretching exercise.
The therapist stands behind the patient and holds the head against the trunk and shoulder while stabilizing it with one hand around the side of the patient’s head and face. On the side of the tightness, place the other hand across the top of the rib cage.
Instruct the patient to breathe in and out, then press downward while they do so. Pick up the slack as soon as the patient exhales.
Repeat it. This moderate stretching technique uses a hold-and-relax movement.
Self-stretching exercises:
The person is straight-backed sitting at a table or chair. While bending the head to one side, maintain a straight chin.
Stretch or gently pull on the neck muscle.
Keep the chin straight while tilting the head to one side and across the shoulder.
He or she will gently stretch, lean away from the table, breathe in and out, hold the stretch position for 20 to 30 seconds, then resume their normal position.
Three to five times on each side, repeat the exercise.
Forward tilt stretch-
Manual stretching exercise:
While seated, locate the second cervical spine’s spinous process and stabilize it with your thumb or the second MCP joint.
Have the patient nod slowly, focusing only on the top of the spine.
On the other hand, direct the movement by placing it across the patient’s forehead.
Exercises to stretch the suboccipital muscles for cervical degenerative disc degeneration or cervicalgia.
Self-stretching exercise:
The patient must tuck his or her chin, flex his or her neck, and bring the chin towards the throat or neck until he or she feels a stretch.
In order to strengthen the forward head movement, the patient must apply pressure with their palm to the back of the head.
The patient should perform a chin tuck before rotating gently 45 degrees towards both sides and nodding.
Three to five times should be done.
Isometric exercises: Self-Resistance
The patient’s tolerance and symptoms will determine the level of intensity for the isometric exercises.
Position of the patient and procedure: Sitting
- Flexion:
- The patient presses his or her forehead firmly into the palms of both hands. Motion is forbidden at the period.
- Side bending/flexion:
- The patient tries to raise the head towards the shoulder while placing one hand against the side, however, the motion is not permitted.
- Extension:
- The patient presses with both hands, just below the top of the head, on the back of the head.
- Rotation:
- The patient presses one hand against the area directly above and to the side of the eye and executes a head-turning maneuver without allowing any movement.
Muscle energy techniques (MET):
This method is also utilized to enhance joint mobility and promote craniocervical mobility. For three to five seconds, the patient holds the muscle contraction against the therapist’s resistance before relaxing. Perform 3 to 5 times.
Cervical traction:
Cervical traction can help with issues resulting from strains, fractures, dislocations, and cervical vertebral degeneration.
In these circumstances, cervical traction might be static, ongoing, or intermittent.
Both supine and seated positions involved applying cervical traction.
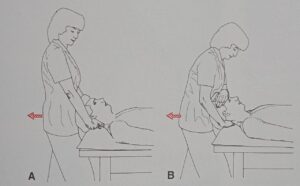
Manual Traction: for the cervical spine:
- The intervertebral foramina are widened as well as the muscles and facet joint capsules are stretched using the traction technique. The force can be delivered specifically and with the least amount of stress to areas that shouldn’t be strained.
- Supine and the therapist are positioned at the head of the treatment table.
- Placement is based on how the patient and therapist feel.
- Under the occiput, place the fingers of both hands. also possible to place one hand on the forehead and the other on the occiput.
Cervical Traction Machine:
- The treatment of choice for cervical dysfunctions is cervical traction.
- This issue can be treated using a variety of cervical traction methods, including continuous, static, intermittent, and polyaxial.
- Wherever you are most at ease is where you should apply traction.
- Traction is not recommended in cases of ligamentous instability, malignancy, fractures, and rheumatoid arthritis with necrosis of the ligaments close to the traction level.
Cervical manipulation:
If cervical spondylosis is not too advanced, cervical manipulation procedures are beneficial.
The cervical manipulation methods are recommended for reducing pain and enhancing joint motion.
When using this approach, precautions should be considered.
Unhealed fractures, rheumatoid arthritis, vertebral artery disease, and acute joint inflammation are all contraindications to manipulation.
Surgical management:
In the following situations, surgery for the cervical condition is typically taken into consideration:
If you experience neurological symptoms like tingling or weakness in your hands and arms. Surgery may be advised in these circumstances to prevent additional issues such as nerve injury brought on by strain on the nerve roots.
Inability to do everyday tasks if the persistent pain is not resolved after at least six months of non-surgical therapy. Patients with these concerns are anticipated to have better surgical outcomes.
Anterior cervical discectomy:
A discectomy, which entails the removal of a damaged portion of the disc and decompression of the nerve root in the cervical spine, is the most popular procedure for treating cervical disc disorders. An “anterior cervical discectomy” is a common name for the procedure, which is carried out through the front of the neck.
Cervical fusion:
Also known as vertebral fusion, this procedure involves removing all of the vertebrae from the cervical spine and acting as a bridge between the vertebrae after the worn-out affected disc of the cervical spine has been removed using a bone graft or metal plates.
Cervical artificial disc replacement:
In this process, the damaged disc is removed and a synthetic disc is put in its place. Patients with early arthritic alterations to the posterior facets may find these cervical artificial disc replacement results to be a very good option. It will provide pain relief and aid in preserving the cervical vertebrae’s regular, normal movement.
Physiotherapy Management of Post-operative Cervicalgia:
In the first several days following surgery, the patient is kept in bed for at least 10 to 12 days.
Use a cervical collar to restrain the neck.
During this stage, the patient received the following advice:
Avoid physically demanding activities
Chest physiotherapy
Lower limb exercise
During mobilization:
Low-intensity exercise was first performed
Exercising the neck muscles isometrically
Neck stretching exercises to improve mobility
After the doctor advised, you can undertake both active and passive ROM exercises
Exercises should be done easily and slowly
Do not move erratically or quickly
Stop any workout that makes you feel uncomfortable or queasy
FAQs
cervicalgia is known as neck pain, In this pain occurs in or around the cervical spine beneath the head
Pain, stiffness, tightness in the upper back, numbness or tingling sensation in the upper back or arm, muscle spasm, Reduce neck movement, tenderness in the cervical area.
Physical strain, bad posture, emotional stress, osteoarthritis, spinal stenosis, ruptured discs, pinched nerves, tumors, and other medical disorders are some of the common reasons.
Cervicalgia, which is neck discomfort that does not radiate to other parts of the body such as down the arms, can afflict anyone. Even though cervicalgia is often not a dangerous illness, it can still be uncomfortable and has to be treated right away.
It may be pointy, dull, or stiffen the neck. The discomfort could only be an annoyance or it might get in the way of regular activities. Fortunately, neck pain seldom indicates a severe condition. And the majority of patients with ordinary neck discomfort will fully heal in four to six weeks.