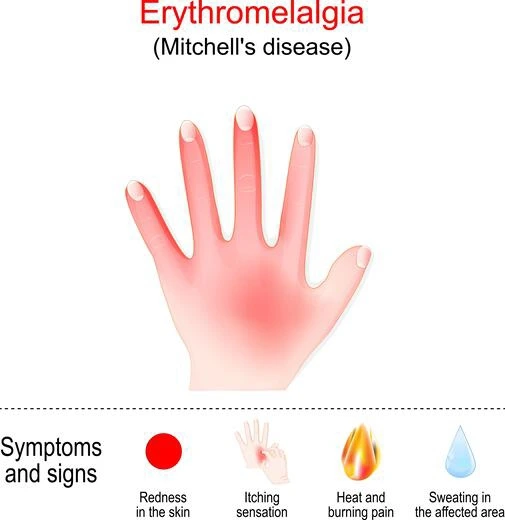
Erythromelalgia
Table of Contents
Definition:
Erythromelalgia is a rare vascular disorder that causes redness, swelling, and burning pain in the extremities, particularly in the hands and feet. It is characterized by episodes of intense heat and burning pain, often triggered by heat, exercise, or stress.
This condition affects both men and women, and it can occur at any age, but it is most commonly diagnosed in individuals between the ages of 20 and 40.
Causes of Erythromelalgia:
The exact cause of erythromelalgia is not fully understood, but it is believed to be related to dysfunction in the small blood vessels and nerves that control blood flow to the skin.
Here are some of the known causes and contributing factors of erythromelalgia:
- Genetic mutations: Erythromelalgia can be caused by inherited genetic mutations that affect the function of sodium channels in nerve cells. These mutations can lead to increased nerve activity and blood flow in the affected areas.
- Secondary to other medical conditions: Erythromelalgia can also occur as a secondary condition to other medical conditions, such as autoimmune diseases, myeloproliferative disorders, and peripheral neuropathies. In these cases, erythromelalgia may be a symptom of an underlying disease.
- Medications: Certain medications, such as calcium channel blockers and vasodilators, can cause erythromelalgia in some people.
- Environmental triggers: Exposure to heat, cold, or changes in temperature can trigger erythromelalgia in some people. Other triggers may include exercise, standing for long periods, or consuming spicy foods.
- Idiopathic: In some cases, the cause of erythromelalgia is unknown (idiopathic).
Overall, the underlying cause of erythromelalgia can vary, and further research is needed to fully understand the condition.
Symptoms of Erythromelalgia:
Erythromelalgia is a rare condition characterized by a set of symptoms that can affect one or more body parts, especially the feet, legs, and hands. The main symptoms of erythromelalgia include:
- Burning pain: The most common symptom of erythromelalgia is intense burning pain, which can range from mild to severe. The pain may be constant or intermittent and can last from minutes to hours.
- Redness: Affected areas of the skin become red and hot to the touch due to the increased blood flow to the skin.
- Swelling: In some cases, the affected area may become swollen, especially if the condition is left untreated.
- Increased skin temperature: The skin in the affected area may feel warm or hot to the touch.
- Increased sweating: Some people with erythromelalgia may experience excessive sweating, particularly in the affected area.
- Changes in skin color: In some cases, the affected area may appear mottled or blue in color, especially after prolonged episodes of erythromelalgia.
- Itching: Itching and a tingling sensation may also occur in the affected area.
The symptoms of erythromelalgia can be triggered by a variety of factors, including exposure to heat, stress, or physical activity.
Diagnosis:
If a person is experiencing symptoms of erythromelalgia, the healthcare provider will begin with a thorough physical examination and medical history to determine the possible cause of the symptoms. Diagnostic tests may also be ordered to confirm the diagnosis and rule out other underlying conditions.
Here are some of the investigations that may be conducted:
- Blood tests: Blood tests may be ordered to check for underlying conditions such as autoimmune diseases, myeloproliferative disorders, or other blood disorders.
- Genetic testing: Genetic testing may be recommended to check for inherited mutations that can cause erythromelalgia.
- Nerve conduction studies: Nerve conduction studies may be performed to evaluate the function of the nerves in the affected area.
- Imaging tests: Imaging tests, such as X-rays or MRIs, may be ordered to check for structural abnormalities or damage to the nerves or blood vessels in the affected area.
- Skin biopsy: A skin biopsy may be performed to examine the skin tissue and check for any abnormalities or inflammation.
- Thermography: This non-invasive imaging test uses infrared technology to measure skin temperature and blood flow, which can help to diagnose and monitor erythromelalgia.
- Provocative testing: Provocative testing involves exposing the affected area to triggers such as heat or exercise to induce symptoms and evaluate their severity.
Treatment of Erythromelalgia:
Treatment for erythromelalgia depends on the underlying cause, severity of symptoms, and response to previous therapies. Here are some of the treatment options that may be recommended for erythromelalgia:
- Lifestyle modifications: Avoiding triggers such as heat, cold, and stress may help reduce symptoms. Wearing loose-fitting clothing, avoiding standing or sitting for long periods, and elevating the affected area can also help to improve blood flow.
- Medications: Several medications may be used to help manage the symptoms of erythromelalgia, including:
- Aspirin: Low-dose aspirin may help reduce pain and inflammation.
Calcium channel blockers: These medications can help reduce blood flow to the affected area and alleviate symptoms. - Topical agents: Topical creams containing lidocaine or capsaicin may be used to reduce pain and improve circulation.
Antidepressants: Certain antidepressants, such as serotonin-norepinephrine reuptake inhibitors (SNRIs), may be used to reduce pain and improve mood. - Nerve blocks: Local anesthetics may be injected into the affected area to provide temporary relief from pain and inflammation.
- Surgery: In severe cases, surgery may be recommended to remove or disconnect the affected nerves or blood vessels.
- Supportive therapies: Physical therapy, counseling, and relaxation techniques may be helpful in managing the symptoms of erythromelalgia.
The treatment of erythromelalgia is focused on reducing symptoms and improving quality of life.
Physiotherapy Treatment in Erythromelalgia:
Physiotherapy can play an important role in the management of erythromelalgia, particularly in helping to alleviate pain, improve circulation, and prevent disability. Here are some of the physiotherapy interventions that may be used:
- Exercise: Exercise can help to improve circulation, reduce pain, and prevent muscle weakness and atrophy. A physiotherapist can design an individualized exercise program that includes stretching, aerobic exercise, and strength training.
- Manual therapy: Soft tissue mobilization, myofascial release, and trigger point therapy may be used to alleviate pain and improve the range of motion in the affected area.
- Thermotherapy: The local application of heat or cold may help reduce pain and inflammation. A physiotherapist can use hot or cold packs, ultrasound, or other modalities to deliver thermotherapy.
- Compression therapy: Compression stockings or sleeves may be used to improve circulation and reduce swelling in the affected area.
- Education and self-management: A physiotherapist can provide education on lifestyle modifications, pain management strategies, and self-care techniques to help you manage your symptoms and prevent disability.
- Relaxation techniques: Deep breathing, guided imagery, and meditation can help reduce stress and improve circulation.
The physiotherapy management of erythromelalgia is focused on improving circulation, reducing pain, and preventing disability.
Conclusion:
Erythromelalgia is a rare and painful condition that can have a significant impact on daily activities and quality of life. The symptoms can be triggered by exposure to heat, exercise, stress, or alcohol and can range from mild to severe. Treatment options include lifestyle modifications, medications, nerve blocks, surgery, and physiotherapy. It is necessary to consult with a healthcare provider to develop an individual treatment plan that meets your specific needs.
FAQs:
What are the complications of erythromelalgia?
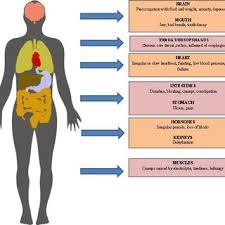
Erythromelalgia is a rare and painful condition that can have a significant impact on daily activities and quality of life. If left untreated or poorly managed, it can lead to several complications, including:
Disability: The pain and other symptoms of erythromelalgia can limit mobility and make it difficult to perform daily activities, leading to disability and reduced quality of life.
Skin changes: Prolonged inflammation and damage to the skin and blood vessels can lead to thickening, scarring, and discoloration of the affected area.
Infections: The breakdown of the skin barrier and decreased immune function in the affected area can increase the risk of skin infections.
Depression and anxiety: Chronic pain and disability can lead to emotional distress, depression, and anxiety.
Reduced blood flow: In severe cases, erythromelalgia can lead to reduced blood flow to the affected area, increasing the risk of tissue damage and gangrene.
Social isolation: The pain and other symptoms of erythromelalgia can limit social interactions and lead to feelings of isolation and loneliness.What diseases are associated with erythromelalgia?
Erythromelalgia can be associated with several underlying medical conditions, including:
Myeloproliferative disorders: These are a group of blood disorders in which the bone marrow produces too many red blood cells, white blood cells, or platelets. Erythromelalgia is commonly seen in patients with polycythemia vera, a type of myeloproliferative disorder.
Autoimmune diseases: Erythromelalgia can occur as a result of autoimmune diseases such as lupus, rheumatoid arthritis, and Sjogren’s syndrome.
Peripheral neuropathies: Damage to the peripheral nerves that carry signals to and from the limbs can lead to abnormal sensations and pain, including erythromelalgia.
Small fiber neuropathies: These are a type of peripheral neuropathy that affects the small nerve fibers that carry pain and temperature signals. Erythromelalgia can be a symptom of small fiber neuropathies.
Fabry disease: This is a rare genetic disorder that leads to the buildup of a fatty substance called globotriaosylceramide in the body’s cells. Erythromelalgia is a common symptom of Fabry disease.
Sodium channelopathies: These are a group of genetic disorders that affect the function of sodium channels in the nerves, leading to abnormal nerve activity and increased sensitivity to pain and other sensations. Erythromelalgia can be a symptom of sodium channelopathies such as primary erythromelalgia and paroxysmal extreme pain disorder.What is the first-line treatment for erythromelalgia?
The first-line treatment for erythromelalgia typically involves lifestyle modifications and medication therapy. The goal of treatment is to reduce the frequency, severity, and duration of symptoms as well as to prevent complications.
Lifestyle modifications may include:
Avoiding triggers: Patients with erythromelalgia should avoid triggers such as heat, exercise, alcohol, and spicy foods, which can exacerbate symptoms.
Cooling measures: applying cool packs, soaking the affected limbs in cool water, or wearing cooling garments can help reduce inflammation and relieve symptoms.
Elevation: Keeping the affected limb elevated can help reduce swelling and improve blood flow.
Compression: Wearing compression stockings or bandages can help improve blood flow and reduce symptoms.
Medication therapy may include:
Aspirin: Low-dose aspirin is a first-line medication for erythromelalgia. It works by inhibiting platelet aggregation and reducing inflammation.
Antihistamines: Certain antihistamines, such as cetirizine and ranitidine, can be effective in reducing symptoms by blocking histamine receptors.
Calcium channel blockers: Medications such as nifedipine and amlodipine can be effective in reducing symptoms by dilating blood vessels and improving blood flow.
Topical treatments: Topical treatments such as lidocaine cream or capsaicin cream can be effective in reducing pain and inflammation.What is erythromelalgia caused by?
The exact cause of erythromelalgia is not well understood, but it is thought to be related to dysfunction of the small blood vessels and nerves in the affected area. It may also be related to underlying medical conditions such as autoimmune diseases, myeloproliferative disorders, or other blood disorders.
Erythromelalgia can also be caused by genetic mutations that affect the function of sodium channels in the nerves. This can lead to abnormal nerve activity and increased sensitivity to pain and other sensations.
Is erythromelalgia an autoimmune disease?Erythromelalgia (EM) is not considered an autoimmune disease in itself, but it can be associated with autoimmune conditions. An autoimmune disease occurs when the body’s immune system attacks its own healthy tissues and organs, causing inflammation and damage.


One Comment