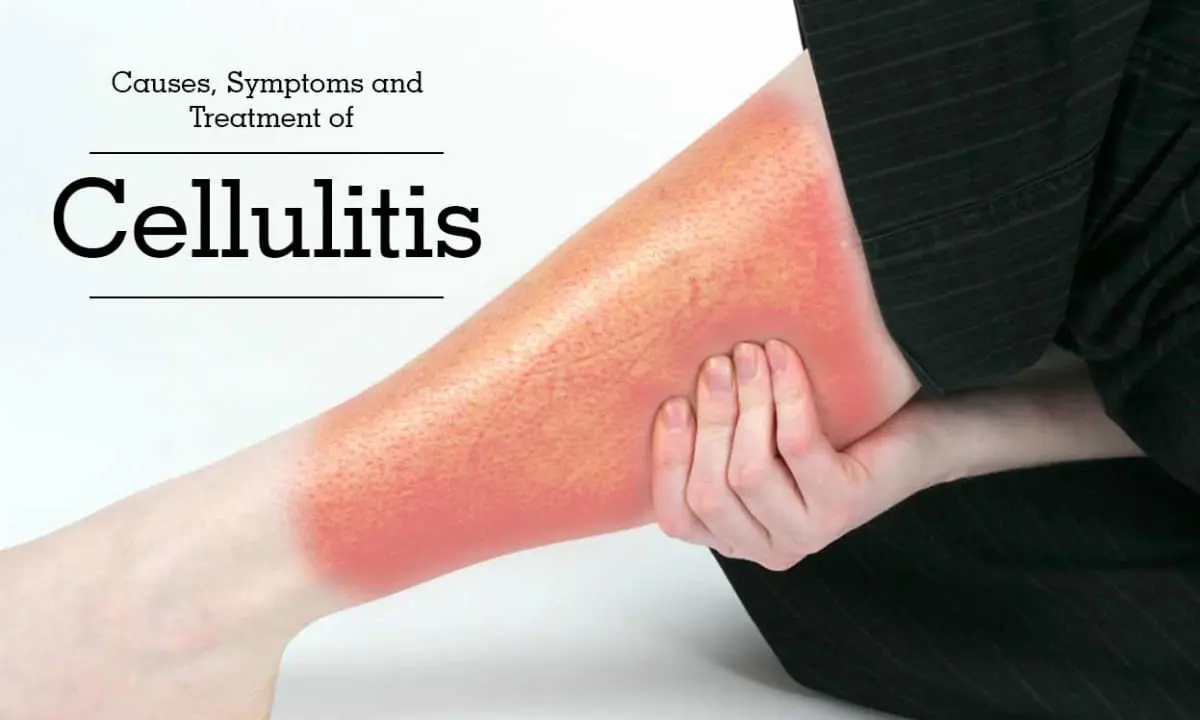
Cellulitis
Table of Contents
Definition:
Cellulitis is a bacterial skin infection that affects the deeper layers of the skin, including the subcutaneous fat and connective tissues. It is a common condition that can cause pain, redness, and swelling, and can affect any part of the body. If left untreated, cellulitis can lead to serious complications, such as sepsis and tissue death.
Symptoms of Cellulitis:
The symptoms of cellulitis usually begin with an area of skin that becomes red, swollen, and warm to the touch. The affected area may also feel tender or painful. As the infection spreads, the redness and swelling may also spread, and the skin may develop a raised, bumpy texture or a rash. In some cases, blisters may form on the skin, and the affected area may feel hot to the touch.
Other common symptoms of cellulitis may include:
• Fever
• Chills
• Fatigue
• Muscle aches
• Nausea and vomiting
• Swollen lymph nodes near the affected area
In severe cases, cellulitis can lead to complications such as blood poisoning or sepsis, which may cause symptoms such as rapid heart rate, low blood pressure, confusion, and difficulty breathing. If you feel any of these symptoms contact your Doctor immediately.
Causes of Cellulitis:
Cellulitis is caused by bacteria entering the skin and spreading throughout the body. The most common bacteria that cause cellulitis are Streptococcus and Staphylococcus. These bacteria are often found on the skin or in the nose and can enter the skin through a cut, scratch, insect bite, or other skin injuries.
The bacteria can also enter the body through medical devices or procedures, such as catheters or surgery. In some cases, cellulitis can be caused by other types of bacteria, such as Pseudomonas or Clostridium.
Once the bacteria enter the skin, they can cause an infection that leads to inflammation and swelling. The body’s immune system responds to the infection, causing the characteristic symptoms of cellulitis, including redness, warmth, and tenderness in the affected area.
In rare cases, cellulitis can be caused by fungal infections or viruses. However, bacterial infections are the most common cause of cellulitis.
Risk factors:
There are several risk factors that may increase the likelihood of developing cellulitis, including:
- Skin injuries: Cuts, abrasions, puncture wounds, insect bites, or other skin injuries can provide an entry point for bacteria to enter the skin.
- Skin conditions: Certain skin conditions, such as eczema, psoriasis, dermatitis, or athlete’s foot, can weaken the skin barrier and make it more susceptible to bacterial infections.
- Compromised immune system: Conditions that weaken the immune system, such as diabetes, HIV/AIDS, cancer, or undergoing chemotherapy, increase the risk of developing infections.
- Obesity: Being overweight or obese can put additional pressure on the skin, leading to cracks, cuts, or sores that can become infected.
- Intravenous drug use: Injecting drugs with contaminated needles or sharing needles can increase the risk of bacterial infections, including cellulitis.
- Age: Elderly people and infants are more susceptible to infections due to their weaker immune systems.
- Recent surgery or hospitalization: Hospital-acquired infections or infections related to medical procedures can lead to cellulitis.
- Lymphatic system disorders: Lymphedema, a condition that causes swelling in the limbs, can increase the risk of developing cellulitis.
It is important to note that not everyone with these risk factors will develop cellulitis, and some people without any known risk factors may still develop the infection. Taking precautions such as maintaining good hygiene and protecting the skin can help reduce the risk of developing cellulitis.
Diagnosis:
The diagnosis of cellulitis is usually made based on a physical examination and medical history. The doctor will examine the affected area and look for signs of redness, swelling, warmth, tenderness, or other symptoms of infection. They will also ask about any recent injuries, medical procedures, or conditions that may increase the risk of cellulitis.
In some cases, the doctor may order tests to confirm the diagnosis and identify the bacteria causing the infection. These tests may include:
• Blood tests: A complete blood count (CBC) can help identify infection by measuring the levels of white blood cells and other markers of inflammation.
• Cultures: A culture of the affected area, such as a skin swab or biopsy, can help identify the bacteria causing the infection and determine the most effective treatment.
• Imaging tests: X-rays, ultrasounds, or other imaging tests may be ordered to rule out other conditions, such as deep tissue infections or abscesses.
It is necessary to seek medical attention if you detect you have cellulitis. Early diagnosis and treatment of infection can help prevent the infection from spreading and decrease the risk of complications.
Treatment of Cellulitis:
The treatment of cellulitis usually involves a course of antibiotics to eliminate the bacterial infection. The type of antibiotics prescribed will depend on the severity of the infection, the age and health of the patient, and any known allergies or sensitivities to antibiotics.
In most cases, cellulitis can be treated with oral antibiotics taken at home. More severe infections or infections in patients with weakened immune systems may require hospitalization and intravenous (IV) antibiotics.
In addition to antibiotics, other treatments for cellulitis may include:
- Pain relief: Over-the-counter painkillers such as acetaminophen or ibuprofen can help alleviate pain and reduce inflammation.
- Elevation: Elevating the affected limb can help reduce swelling and improve circulation.
- Compression: Wearing compression stockings or bandages can help reduce swelling and improve circulation.
- Wound care: The affected area must be clean and dry to prevent further infection and promote healing.
- Surgery: In rare cases, surgery may be necessary to drain an abscess or remove infected tissue.
It is necessary to complete the full course of antibiotics as prescribed, even if symptoms recover before the medication is finished. Failure to complete the full course of antibiotics can increase the risk of the infection returning and may lead to antibiotic resistance.
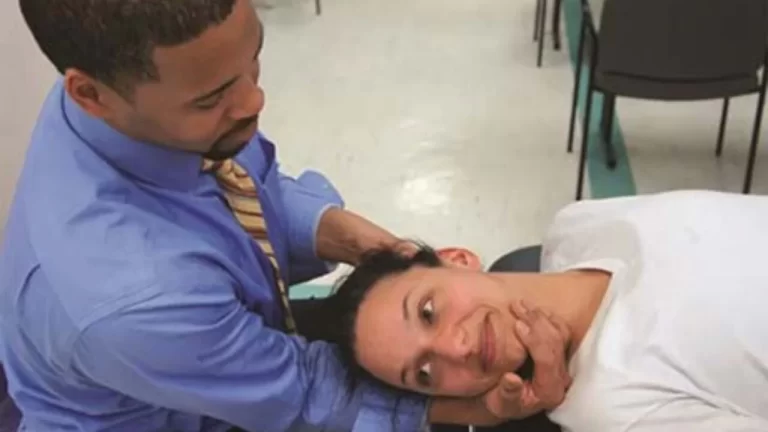
Physiotherapy Treatment in Cellulitis:
Physiotherapy can play an important role in the management of cellulitis, particularly in cases where the infection affects the limbs. The goals of physiotherapy for cellulitis may include:
Reducing swelling: Physiotherapists can use manual lymphatic drainage (MLD), compression bandaging, or other techniques to reduce swelling and improve lymphatic drainage in the affected limb.
Improving mobility: Cellulitis can cause pain, stiffness, and limited mobility in the affected limb. Physiotherapists can prescribe exercises to help improve the range of motion and strengthen the affected muscles.
Preventing recurrence: Physiotherapists can teach patients self-care techniques, such as skin care, exercise, and compression bandaging, to help prevent future episodes of cellulitis.
Education and advice: Physiotherapists can provide education and advice on how to manage symptoms and prevent complications, such as deep vein thrombosis or lymphedema.
The specific approach to physiotherapy for cellulitis may vary depending on the individual case and the severity of the infection. It is important to consult with a physiotherapist who is experienced in managing cellulitis to develop an appropriate treatment plan. Physiotherapy should be used in conjunction with appropriate medical management, such as antibiotics, wound care, and pain management, to ensure the best possible outcome for the patient.
How to Prevent Cellulitis?
There are several steps that can be taken to help prevent cellulitis:
- Keep skin clean and dry: Regular washing with soap and water can help prevent the buildup of bacteria on the skin. It is important to dry the skin thoroughly, especially in areas where moisture can accumulate.
- Protect skin from injury: Wearing protective clothing, such as gloves and long sleeves, can help prevent cuts, scrapes, and other injuries that can provide an entry point for bacteria.
- Treat cuts and scrapes promptly: Clean cuts and scrapes with soap and water and apply an antiseptic ointment and a bandage to prevent infection.
- Manage skin conditions: People with skin conditions such as eczema or psoriasis are at higher risk of developing cellulitis. It is important to manage these conditions with appropriate skin care and medication.
- Avoid sharing personal items: Sharing items such as razors, towels, or nail clippers can increase the risk of spreading bacteria.
- Seek medical attention for signs of infection: It is important to seek medical attention promptly if you have symptoms of an infection, such as redness, swelling, warmth, and tenderness.
- Manage underlying medical conditions: People with diabetes, obesity or other medical conditions that affect the immune system or circulation are at higher risk of developing cellulitis. It is important to manage these conditions with appropriate medical care and lifestyle changes.
By taking these steps, it is possible to reduce the risk of developing cellulitis and other skin infections.
Conclusion:
Cellulitis is a common bacterial skin infection that can be easily treated with antibiotics and self-care measures. Early diagnosis and prompt treatment are crucial to prevent complications and ensure a full recovery. Taking steps to prevent skin injuries and infections can also help reduce the risk of developing cellulitis.
FAQs
What is the main cause of cellulitis?
The main cause of cellulitis is a bacterial infection, usually caused by Streptococcus or Staphylococcus bacteria. These bacteria can enter the body through a break in the skin, such as a cut, scrape, insect bite, or surgical incision. Once the bacteria enter the body, they can cause an infection in the underlying tissues, leading to inflammation, redness, swelling, and pain.
Factors that can increase the risk of developing cellulitis include having a weakened immune system, such as from diabetes or HIV/AIDS; having a chronic skin condition such as eczema; having lymphedema, which can cause fluid buildup and swelling in the limbs; or having a history of cellulitis. It is important to take appropriate measures to prevent skin breaks, such as keeping the skin clean and moisturized and seeking prompt medical attention if you have any signs or symptoms of cellulitis.What is the fastest way to get rid of cellulitis infection?
There is no one “fastest” way to get rid of cellulitis, as the treatment will depend on the severity of the infection and other individual factors such as age, overall health, and medical history. However, here are some steps that may help speed up the healing process:
Take antibiotics: Antibiotics are the primary treatment for cellulitis. It is important to take the full course of antibiotics as prescribed by your healthcare provider, even if symptoms improve before the medication is finished.
Elevate the affected limb: elevating the affected limb above the level of your heart can help reduce swelling and improve circulation, which may speed up the healing process.
Use warm compresses: Applying warm compresses to the affected area can help reduce pain and promote healing.
Get plenty of rest. Resting can help your body fight the infection and allow time for the antibiotics to work.
Manage underlying medical conditions: If you have an underlying medical condition, such as diabetes or lymphedema, it is important to manage it appropriately to reduce the risk of recurrent infections.What are the three symptoms of cellulitis?
There are several symptoms of cellulitis, but here are three common ones:
Redness: The affected area of the skin may appear red, and the redness may spread over time.
Swelling: Cellulitis can cause swelling in the affected area, which may feel warm or tender to the touch.
Pain: The affected area may be painful, especially when touched or when pressure is applied.
Other symptoms of cellulitis can include fever, chills, fatigue, and the development of blisters or abscesses.What are the dos and don’ts for cellulitis?
Here are some general dos and don’ts for cellulitis:
Do:
• Take antibiotics as prescribed by your doctor. Finish the entire course of antibiotics, even if you start to feel better before you have completed the course.
• Elevate the affected limb above the level of your heart to help reduce swelling and improve circulation.
• Use warm compresses on the affected area to help reduce pain and promote healing.
• Get plenty of rest to allow your body to fight the infection of cellulitis.
• Take care of your affected skin by keeping it clean and moisturized.
• Seek medical attention if you notice any signs of a worsening infection or if you develop a fever or other symptoms.
Don’t:
• Ignore the symptoms of cellulitis, as it can lead to serious complications if left untreated.
• Do not scratch or pick at the affected area, as this can introduce more bacteria and worsen the infection.
• Do not use over-the-counter creams or ointments without consulting your healthcare provider, as they may not be effective and could worsen the infection.
• Delay seeking medical attention if you have symptoms of an infection or if you have a history of cellulitis.
• Neglect underlying medical conditions such as diabetes or lymphedema, as these can increase the risk of developing cellulitis.How long does cellulitis last?
The duration of cellulitis can vary depending on several factors, such as the severity of the infection, the age and health of the patient, and the effectiveness of treatment. In general, mild cases of cellulitis may improve within a few days with appropriate antibiotic treatment and self-care measures such as rest and elevation of the affected limb.
More severe cases of cellulitis or infections in patients with weakened immune systems may require hospitalization and intravenous antibiotics, which can take several days or even weeks to complete. The presence of abscesses or other complications may also prolong the duration of the infection.





4 Comments