Pott’s Paraplegia
Table of Contents
What is pott’s paraplegia?
Pott’s paraplegia resulting in severe spinal deformity is a disastrous complication, which is difficult to treat by chemotherapy alone and by surgical decompression. It is commonly accepted that Pott’s paraplegia in early spinal tuberculosis can be cured effectively through chemotherapy alone.
Tuberculous spondylitis known as Pott’s disease refers to vertebral body osteomyelitis & intervertebral discitis from tuberculosis (TB). The spine is the most often area of musculoskeletal tuberculosis, & commonly related symptoms are back pain, kyphotic deformity of the spine, lower limb weakness, & paraplegia.
Pott disease is tuberculosis of the spine that occurs usually because of hematogenous spread from other sites, often the lungs. Percival Pott was the first person to explain the classic description of spinal tuberculosis in 1779; hence, spinal TB was called ‘Pott’s Disease. Tuberculosis of the spine is one of the oldest determined diseases of mankind & is the common extrapulmonary form of TB.
Lower thoracic & lumbar vertebrae are the most common areas of spinal TB followed by middle thoracic & cervical vertebrae. The second cervical to the seventh cervical localization is reportedly involved in 3 to 5% of cases and atlantoaxial articulation is less common. In TB, the involvement of posterior elements because of tuberculosis is not so uncommon. The lamina was the most commonly involved site followed by pedicles, articular processes, spinous processes, & transverse processes.
It leads to a kind of tuberculous arthritis of the intervertebral joints. The infection can spread from 2 adjacent vertebrae through the adjoining intervertebral disc space. If only one vertebra is affected, the disc is normal, but if two vertebras are affected, the disc, which is avascular, cannot have nutrients and collapses. In a process called caseous necrosis, the disc tissue dies, leading to vertebral narrowing & eventually vertebral collapse & spinal damage. A dry soft-tissue mass frequently forms and superinfection is rare. The spread of infection from the lumbar vertebrae to the psoas muscle, causing abscesses, is usual.
Spinal tuberculosis is a worldwide public health issue that is one of the main causes of disability. Osteoarticular tuberculosis, which affects 1–2% of people with tuberculosis, is always a secondary infection that individuals with primary TB elsewhere in the body have. The most serious type of bone TB is Pott’s paraplegia. The spinal cord is compressed, there is a gradual neurologic loss, & there might be deformity as the infection frequently starts from the vertebral body with noticeable damage and the creation of a cold abscess.
What are the causes of paraplegia?
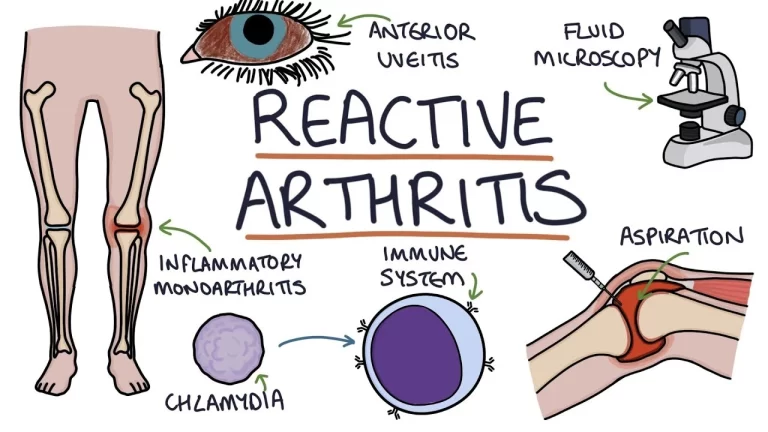
The most frequent cause of TB in humans is Mycobacterium tuberculosis. Mycobacterium microti, Mycobacterium Bovis, and Mycobacterium africanum are other mycobacteria that cause human TB. Mycobacterium is a meticulous, aerobic bacteria that grows gradually. Mycobacterium-containing droplets travel through the air & land on the lungs, where alveolar macrophages consume them. Most of these microorganisms are eliminated. Few are capable of surviving and proliferating in macrophages, which leads to a type IV inflammatory response that causes granulomas to develop. In this granuloma, bacteria can stay latent & persist for decades.
Whether an infection is healed or not depends on how well the host cell-mediated immune response functions. Mycobacterium might escape from granuloma if the immune response against the pathogen is insufficient. A mycobacterium that has escaped can either cause an active lung infection or it can enter other organs via hematogenous and lymphatic routes. With the hematogenous spread of infection from a primary area, spinal involvement is typically subsequent. Spinal involvement starts from the lungs or the genitourinary system.
Someone with active TB infections can spread through the air with aerosol droplets by spitting, sneezing, coughing, speaking, etc. Each sneeze can release up to 40,000 aerosol droplets, & it only takes one infected droplet to spread TB.
Since the intervertebral disc lacks its own blood supply, the infection travels there from the vertebra next to it. Mycobacterium enters the highly vascular cancellous bone of the vertebral body via the venous or arterial pathway. Paradisal involvement results from the transmission of infection through the vascular plexus formed by the arterial arcade generated from the posterior and anterior arteries. The valveless Batson’s paravertebral venous plexus system allows for an unrestricted flow of blood which is dependent on pressure.
What are the symptoms of pott’s paraplegia?
There are several early signs of tuberculosis including night sweats, fever, weight loss, etc. whereas, spread to the spine would be determined by severe back pain, this patient may face difficulty in standing and walking. Severe back pain is the most often symptom of Pott’s disease, nevertheless, systematic symptoms such as anorexia, fever, fatigue, night sweats, weight loss, etc. are also common.
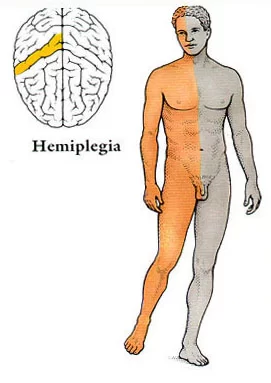
The swelling of the infection site might cause weakness or numbness in the legs. In a complicated tubercular spine, disease patient may present with rest pain, deformity, bone destruction, instability, and sometimes radicular pain would be the main symptom. In Pott’s paraplegia, the presence of a neurologic deficit is not quite common and the percentage of incidence greatly varies due to the stages of the disease. Pott’s illness can therefore result in a significant curvature of the spine & limb paralysis. Spinal cord involvement in Pott’s illness can be caused by direct pressure from abscess development and bone sequestra
Tenderness, spasms, Neurological deficits, and spinal deformities are the primary clinical features. Nerve root pain, paraplegia, and sensory deficits were also seen in the patient. He even complained of difficulty in breathing and performing activities of daily living and bowel and bladder incontinence.
Progressive neurological deficit in Pott’s paraplegia:
During the active Pott’s paraplegia stage of or after healing, there might be some neurological deficit. The vertebral collapse because of TB would result in the involvement of the anterior spinal tract. Later, the posterior column lack is followed by a gradual involvement of the lateral spinal pathways. Scores such as Frankel & ASIA ratings would also be used to categorize the neurological loss in spinal tuberculosis. The most useful classification for Pott paraplegia with spinal cord involvement is the modified version of the Tuli classification. Motor fibers are crushed initially because they are not situated similarly, as seen in the typical Pott’s paraplegia or anterior spinal TB. As an outcome, the sensory fibers are only implicated later on.
When compression occurs because of anterior or posterior spinal tuberculosis, pressure is initially given to the column of cerebrospinal fluid around the cord before being conveyed to the ligamentum denticulatum. The claims made by Bosworth et al. that the tubercular pus consists of a chemical that prevents the spinal cord from conducting properly seem speculative. The categorization of Pott’s disease, whether brought on by anterior or posterior spinal TB, should primarily be based on the level of motor involvement to constitute the severity of cord compression. As the degree of compression elevates, sensory & autonomic functional loss is increased. Sensory recovery comes before motor recovery.
When an intraspinal tuberculous granuloma is initially observed, it often exhibits compressive myelopathy or a cauda equina lesion with sphincter involvement. They are diagnosed with “spinal tumor syndrome,” which covers both tumorous and non-tumorous disorders of the spinal cord & meninges because they exhibit no clinical spinal deformity upon inspection.
Classification of pott’s paraplegia:
Tuli and Kumar’s grading of paraplegia:
- negligible- unaware of neural deficit, the physician detects plantar extensor or ankle clonus
- mild- aware of the deficit but manages to walk with support /UMN features
- moderate-nonambulatory paralysis in extension, sensory deficit<50%
- severe- 3+flexor spasm/paralysis in flexion/flaccid, sensory deficit>50% /sphincter involved
What are the complications of pott’s paraplegia?
Patients with spinal infections are bedridden for a certain period of time, which is longer in those with neurologic deficits or those who were recommended surgical operation. These patients should be observed closely in terms of complications & treated accordingly. Failing to detect and treat complications, such as hypertension, hypotension, deep venous thrombosis, pulmonary infections, urinary retention, urinary infections, spasticity, contractures, decubitus ulcers, depression, & osteoporosis increase morbidity and mortality.
Spinal deformity and paraplegia are the specific complications of spinal tuberculosis both of which occur more frequently in cases of delayed diagnosis and management. Patients with an initial kyphotic angle of 30 degrees or less should be treated with antituberculous medicines, with close monitoring for the progression of the deformity. Rehabilitation programs for patients with neurologic deficits or those who had a surgical operation due to spinal infections should be conducted with more care. Complications are observed more often and the response to treatment is delayed because of the longer immobilization period.
How to prevent pott’s paraplegia?
Controlling the growth of tuberculosis infection can prevent tuberculous spondylitis and arthritis. Patients who have a positive PPD test but not active tuberculosis might decrease their risk by properly taking medicines to prevent tuberculosis. To successfully treat tuberculosis, patients must take their medications exactly as prescribed.
What is the diagnostic procedure for pott’s paraplegia?
Mycobacterium culture is the gold standard for diagnosing tuberculosis, nevertheless, as it’s a fastidious microorganism relying solely on positive cultures for diagnosis might have low sensitivity. To confirm the diagnosis, further laboratory reference standards such as microbiological, immunological, hematological, serological, & other diagnostic studies should be employed. MRI is most often used for the diagnosis and cold abscesses by using ultrasound. Myelography has an important role diagnosis of patients who do not heal neurologically and in situations where there are multiple skipped multifocal spinal lesions to identify which lesion is causing compression.
Imaging modalities:
Radiography
Plain radiographs were suggested previously as an imaging modality for Pott’s disease. As a first-stage diagnosis process, conventional lateral radiographs are utilized to look for TB infection. These radiographs typically present osteolysis affecting the entire vertebral body with diffuse osteopenia.
Computed tomography (CT) scan
With great sensitivity, computed tomography (CT) can help in the diagnosis at a far earlier stage than ordinary x-rays (100%). CT is a valuable & common diagnostic tool, in cases with Pott’s disease which would able to demonstrate the extension of soft tissue involvement clearly. For the intention of making a diagnosis, CT scans can also help in the image-guided biopsy.
Magnetic resonance imaging (MRI)
With 100% sensitivity and 80% specificity, magnetic resonance imaging (MRI) is the most useful modality in the diagnosis of spinal TB. The site of the abscess, the degree of soft tissue enhancement, & spinal canal impairment are all best detected with MRI. MRI with gadolinium enhancement might give more details on the diagnosis. We can also identify non-contiguous vertebral involvement by doing screening sequences that involve the whole spine. MRI can be utilized to evaluate therapy response. MRI can also demonstrate the number of lesion and their sites in cold abscesses. The early detection of inflammatory edema could be ensured by T2 STIR images.
Nuclear imaging
Nuclear imaging can provide descriptive evidence of the activities in the affected tissues. These techniques are unable to assist differentiate between cancer or other pyogenic diseases & tubercular infections.
Laboratory tests
Laboratory tests such as the Erythrocyte sedimentation rate (ESR) & C-reactive protein (CRP) are less common tests. ESR has a sensitivity of 90% and CRP has a sensitivity of 71%, nevertheless, has more specificity than ESR. The serological tests have a round of restrictions. IgG & IgM (antibody test) levels are not effective to determine the distinction between natural TB infection, vaccinated person, active disease, or healed person. Traditional TB culture, Acid-fast bacilli staining, & BACTEC assay are some general laboratory techniques. Isolation of Mycobacterium tuberculosis with computed tomography (CT) guided needle biopsy or open surgical management can yield an accurate diagnosis. In cases receiving anti-TB chemotherapy in the lead-up to surgery, it is difficult to show typical acid-fast bacilli on staining with hematoxylin-eosin, & the consequences of TB cultures are typically negative in such cases. Histological examination of formalin-fixed and paraffin-embedded tissue specimen blocks typically gives a granulomatous pattern with caseating necrosis & giant-cell granuloma.
Molecular diagnosis
Various types of molecular techniques are utilized for diagnosis with high sensitivity and specificity. Polymerase chain reaction (PCR) with a sensitivity of 75% and specificity of 97% is used in paucibacillary, extrapulmonary TB infections. Fully automated Gene Xpert MTB/RIF help in the diagnosis of resistance towards antibiotics with high sensitivity & specificity. In between 72% and 97% of patients, specific features such as Langhans large cells, epithelioid cell granuloma, and caseating necrosis can be found through histopathological examinations.
Tests to detect latent tuberculosis
The skin hypersensitivity test has been advocated as a low-cost test; nevertheless, it is not a reliable test in areas where patients are immunocompromised. Some studies also recommend the use of the enzyme-linked immunosorbent test (ELISA) and the interferon-gamma release assay.
What is the treatment plan for pott’s paraplegia?
Before treatment of Pott’s paraplegia, it is important to determine the severity of the spinal tuberculosis disease, based on presentation & symptoms. The uncomplicated disease is treated with antitubercular treatment or chemotherapy & complicated cases usually need surgical intervention with chemotherapy. There are various types of surgical procedures are available.
The most useful classification for Pott paraplegia with spinal cord involvement is the modified version of Tuli’s classification which consist of five stages. The First stage involves intense tendon reflexes, ankle clonus, plantar or Babinski extensor. During the second stage, the patient has a motor deficit (UMN-type) with spasticity. In stage three patient becomes spastic and bedridden. The patient becomes bedridden including severe sensory deficit/pressure sores in the 4th stage. The final or 5th stage is the same as the 4th stage of bladder or bowel involvement.
Oguz et al. proposed a new classification system for Pott’s disease called Gulhane Askeri Tıp Akademisi widely known as GATA. Where they classified Pott’s Paraplegia elicited from clinical & radiological status into three categories (IA/B, II, and III). GATA suggested surgical treatment for patients with Type IB with no neurological deficit, Type II and Type III (with or without neurological deficit). M. Turgut et al. (2017) presented a new easily modified classification system from the GATA system. The modified system is a simple guide for treatment plans in patients with Pott’s disease for young spinal surgeons.
Medical treatment for pott’s paraplegia:
In patients with spinal tuberculosis, antitubercular treatment should be initiated as early as possible. Antituberculous treatment frequently needs to be instituted empirically, much before an etiological diagnosis is established. In poor countries, etiological diagnoses might not be established at all. In patients with established complications of spinal tuberculosis, surgery might also be needed. Sequelae like kyphosis require surgical intervention.
Almost all antituberculous drugs penetrate easily into tuberculous vertebral abrasions. The marketing of antituberculosis drugs such as rifampin, isoniazid, and pyrazinamide was assessed in pretentious vertebral tissues of spinal tuberculosis. In patients with left-out vertebral sclerotic walls around the tuberculous foci, the isoniazid concentrations in foci were of bactericidal levels.
Levels of rifampin & pyrazinamide in foci corresponded to the minimal inhibitory concentrations of each drug, separately. The sclerotic bone of the affected vertebra played a role in resisting the antituberculosis drug’s penetration. In another study, three drugs resulted in an effective bactericidal concentration level in osseous tissues around the foci of spinal tuberculosis excluding the 4 mm of osseous tissue surrounding the sclerotic wall. The output recommended that osseous tissues within 4 mm surrounding the sclerotic wall should be removed during the surgery.
Antituberculous treatment
Various studies have shown that the majority (82–95%) of patients with spinal tuberculosis respond very well to medical treatment. The treatment response is apparent in form of pain relief, a decrease in neurological deficit, & even correction of spinal deformity.
Patients with potentially dangerous craniovertebral junction tuberculosis respond satisfactorily to medical treatment. Patients with medically resistant spinal tuberculosis require a careful reassessment of the differential diagnosis before surgery is planned surgery.
Therapeutic regimen:
World Health Organization (WHO) advocates a category-based treatment for tuberculosis. Spinal tuberculosis is put down under category 1 of the WHO treatment category. The category-1 antituberculosis treatment program is classified into two phases: an intensive or initial phase & a continuation phase. In the 2-month intensive phase, antituberculous therapy involves a combination of four first-line drugs: isoniazid, rifampicin, streptomycin, & pyrazinamide. In the continuation phase, two drugs isoniazid and rifampicin are allowed for 4 months.
Due to the serious risk of disability & mortality and because of difficulties in assessing treatment response, WHO suggests 9 months of treatment for tuberculosis of bones or joints.
The American Thoracic Society recommended 6 months of chemotherapy for spinal tuberculosis in adults and 12 months in children.
The British Thoracic Society suggests 6 months of daily treatment with rifampicin and isoniazid, supplemented in the starting 2 months with pyrazinamide and either ethambutol or streptomycin, regardless of age.
Although 6 months of treatment is considered sufficient, many experts still prefer a time period of 12–24 months or until radiological or pathological confirmation of regression of disease occurs. To avoid poor compliance, directly observed treatment and short-course regimens might be administered. There is no certain role for corticosteroids in spinal tuberculosis excluding cases of spinal arachnoiditis or nonosseous spinal tuberculosis.
Supportive measures:
Common supportive measures, together with prolonged recumbency & rest, formed the basis of treatment for a patient with tuberculosis of the spine before the phase of antituberculous chemotherapy. Sanatorium care was formerly the avenue of treatment for patients with pulmonary & bone tuberculosis.
Today, the majority of patients with bone tuberculosis are healed with ambulatory care without prolonged recumbency and rest. Although cast or brace immobilization was a typical form of treatment, it was found to be inefficient and has usually been abandoned.
Surgical treatment for pott’s paraplegia:
There is debate about the precise role of surgery in the treatment of spinal tuberculosis. This difference of opinion goes back to 1960 when Hodgson and Stock suggested surgical treatment, & Konstam and colleagues advised conservative treatment. However, many experts feel that not either all cases of tuberculosis of the spine should be treated conventionally, or not all cases need surgery.
Approx 40% of the cases of tuberculosis of the spine with paraplegia present recovery with antituberculous treatment, rest, & traction. Tuli advocated a ‘middle-path regimen’ for the treatment of spinal tuberculosis. It advocated conservative treatment with multi-drug chemotherapy & surgery reserved for specific indications.
In some circumstances, nevertheless, surgery appears to be beneficial & might be indicated. Potential profits of surgery were rapid pain relief, less kyphosis, immediate decreased symptoms of compressed neural tissue, a higher percentage of bony fusion, quicker bony fusion, less relapse, earlier return to previous normal activities, & less bone loss. It might also avert late neurological problems because of kyphosis of the spine if fusion does not occur. One expert advocated that indications for surgery were pan-vertebral damage, severe kyphosis, refractory disease, an evolving neurological deficit, & clinical deterioration or less clinical improvement.
Two types of surgical techniques are performed. 1st is the debridement of the infected material. In this type of surgery, no effort is built to stabilize the spine. The 2nd process is debridement with stabilization of the spine. This is a more extensive process & the reconstructions occur with bone grafts. Stabilization might also be done using fabricated materials like carbon fiber, steel, or titanium.
The combined surgical and medical treatment gave very good results. The surgical treatment consists of extensive posterior decompression/instrumented fusion & three-level posterior vertebral column resection, followed by anterior debridement/fusion with cage reconstruction. For a patient with progressive Pott’s paraplegia & severe kyphotic deformity, for patients whom medical treatment failed, posterior vertebral column resection, multiple-level posterior decompression, & instrumented fusion, followed by an anterior interbody fusion with cage were used to decompress the spinal cord, restore sagittal alignment, & debride the infection.
Currently, the treatment of spinal tubercular infections needs a multidisciplinary team that includes infectious disease experts, neuroradiologists, & spine surgeons. The key to successful management is early identification & timely and judicious surgical management, the decision of which needs to be taken in view of clinical-radiological compression of the spinal cord & nerve roots, age of the patient, and the response of antitubercular therapy (ATT).
Anterior decompression/corpectomy, strut grafting/ posterior column shortening, or posterior instrumented stabilization
Indications:
- neurologic deficit
- acute severe paraplegia
- with panvertebral inclusion with or without subluxation or dislocation
- spinal instability
- kyphosis correction > 60° in adult
- progressive kyphosis in a child
- ≥3 vertebrae involved in the thoracic spine
- children ≤ 7 years affected in T/TL spine and ≥ 2 at-risk signs are likely to have progression and should undergo correction
- late-onset paraplegia
- advanced disease with caseation averting access to antibiotics
- failing of nonoperative treatment after 3 to 6 months
- diagnosis uncertain
- panvertebral lesion
Advantages of surgical treatment:
- less progressive kyphosis
- decreased sinus formation
- earlier healing
- in patients with neurologic deficits, early debridement & decompression lead to the improved neurologic recovery
Technical aspects:
- Autogenous & allograft stride grafts are acceptable with good results
- continue medical management program with isoniazid, rifampin, and pyrazinamide
- chronic implant colonization is less common in tuberculosis & other granulomatous infections compared to more common pyogenic infections
Halo traction, bone grafting, anterior plating, anterior decompression
Indications:
- cervical kyphosis
Pedicle subtraction osteotomy
Indications:
- lumbar kyphosis
Direct decompression / internal kyphectomy
Indications:
- correction of treated thoracic/thoracolumbar kyphosis
- allows the spinal cord to relocate anteriorly
Physiotherapy treatment for pott’s paraplegia:
The aim of treatment is to achieve healing of disease, and to prevent, and detect early and promptly any complication like paraplegia. Rest- bed rest for pain relief and to restrict further collapse and dislocation of diseased vertebrae
Spinal orthosis
Indications:
- might be used for pain control and prevention of deformity
- for the cervical spine: Minerva jacket, collar
- taylor’s brace
The most important factor in the SCI rehabilitation program is early rehabilitation. The positioning in the acute phase and early starting of passive, active-assisted, and active exercises will greatly contribute standing of the patient earlier and to mobilization. Standing and mobilization are not recommended in the acute duration for these patients. Generally, standing and ambulation are suggested during the subacute period. For patients with spinal tuberculous, bracing with a conforming orthosis has been used in combination with antituberculous drugs as initial treatment. Bracing is continued 3 months after the first radiologic sign of bony fusion.
The onset of pain or elevation in pain during exercise programs in the early period should be evaluated carefully. Pain-aggravating exercises should be avoided & the exercise program should be discontinued if there is a significant increase in pain intensity disturbing the patient following the rehabilitation program. The patient should not be exhausted during exercise and mobilization and should have an adequate resting period after exercise. High-calorie diet regimens should be given since metabolic requirements are increased during both disease and the rehabilitation period.
The rehabilitation program is given with respect to the neurologic status of the patient. For this purpose, the levels at which the spinal cord injury might occur and the involved segments are determined before implementation of the program. Following a detailed physical and neurologic assessment, the determination of the region in the lesion affects the type of paralysis, the urologic & neurologic status, concomitant diseases, the age of the patient, and the involved area is crucial to establish a realistic & optimal rehabilitation program. Following this assessment, patients should be monitored closely in terms of maintaining bed care, good posture, & positioning during early rehabilitation. The presence of instability and the type of surgical process is important for the implementation of a rehabilitation program. Musculoskeletal problems & secondary problems as a result of immobilization should be monitored and prevented.
In patients with severe neurologic findings because of spinal cord compression, the rehabilitation program differs according to acute, subacute, and chronic stages. In cases with spinal infections, medical treatment should be considered at first, even in cases with spinal cord compression because of a paravertebral abscess. Nevertheless, both surgery and medical treatments are necessary in cases of neurologic involvement.
Problem list and Physiotherapy Strategies:
- Pain: Tens were given for bilateral lower limbs, frequent positioning, and ergonomic advice was given
- Sensory deficits: Sensory re-education was given to bilateral lower limbs
- Decreased Strength: Active Range of motion exercise training, Mild resisted exercise training was given for weak muscles
- Respiratory issues: Breathing exercises, Thoracic expansion exercises, and Autogenic drainage techniques were taught
Acute stage
The most important factor in the acute rehabilitation duration is to determine the patient’s physical capacity. According to the degree of infection, muscle weakness can be seen in varying degrees in the lower, upper extremity, and trunk muscles. Bed positioning in appropriate dermatomal areas, passive joint movements, and breathing exercises are important in the acute phase of flaccidity. Each group of muscles must be evaluated individually if there is muscle weakness. Isometric, passive, active-assisted, & active exercises are performed to improve the functional capacity of muscles. This should be done at least daily, which will assist to prevent contractures. The shoulder, elbow, hip flexors, and ankles are most important to the range because contractures are most frequently observed in these joints in the acute rehabilitation unit. The most important aspects in the acute period include bowel, bladder, and pulmonary management, deep venous thrombosis, gastrointestinal prophylaxis, and proper positioning in bed with turning at least every 2 h. The trunk and extremities should be properly positioned & the feet should be supported in a neutral position. If the level of spinal infection is in thoracic vertebrae, respiratory exercises are advised. The pressure must be decreased in order to prevent decubitus ulcers. While in the supine position, the patient is turned from one side to the other every 2 hours to reduce pressure and monitored constantly for erythema formation. An indwelling catheter is arranged if urinary incontinence is present.
In the acute stage, isometric exercises are initiated during the pre-operative period & continued during the early postoperative period. The patient is assisted to be mobilized within the bed by turning from one side to the other side. Isometric contraction is sustained by isometric compression of the lumbar, thoracic, & sacrospinal muscles towards the bed. Isometric exercises are performed in cervical, thoracic, and sacrospinal muscle groups & all lower extremity muscles; the patient in the supine position continues to elevate the head and shoulder until the toes are visible. Gluteal muscles are contracted and relaxed bilaterally and isometric contraction of the pelvic muscle group is given.
Subacute stage
The subacute period is the out-of-bed ambulation period of the patients. According to the width of the area of infection & the patient with appropriate assistive devices bodice & on the side of the bed before backing out of bed by then, with crutches or walker is aimed at mobilization. Also bearing exercises and quadriceps exercises in addition to the side of the mattress are required to be done in an active way. Standing on the edge of the bed and standing properly ways are taught.
Active and active assisted exercises are performed in the subacute phase. Feet are raised straightly and contraction of hip flexors and lumbar extensors is performed by raising the bilateral quadriceps muscles around 20 cm. The patient is helped with the corset to sit on the bed (supported or unsupported). Balance exercises are performed at this position. The patient is assisted in walking by cane or walker. Mobilization is repeated up to 3 to 4 times daily. The patient should leave to rest after the onset of signs of fatigue. Assistive equipment is withdrawn after the successful independent mobilization of the patient. Clean intermittent catheterization is positioned instead of continuous indwelling catheters to prevent urinary infections. The patient should be examined at certain intermissions for urinary infection, should drink enough water, & should be ambulated continuously. The patient should be fed high-fiber food to prevent constipation which may be a significant problem. The patient should be taken to the restroom once or twice a day to stimulate defecation. If the upper extremities are preserved, active strengthening exercises should be applied to all upper extremity joints.
Chronic stage
The chronic period is a term when the patients return back to his previous life and regain maximum independence. For this purpose, the patients should be away from the bed. Mobilization should be given independently supported or unsupported. Lying down, sitting and standing exercises should include active and resistive exercises. The balance and gait exercise assets should be studied in parallel bars. Climbing stairs, squatting, and sitting on the ground activities like lifting should be done. The patients are assisted to walk via using crutches or orthotics during the chronic stage. Patients who achieve trunk and pelvic stabilization are taken to the parallel bar by wearing a corset for standing exercises. In standing position, forward, backward, & sideways stepping exercises, as well as neutral position exercises such as forward flexion-extension, are performed. Cat and camel stretching exercises are performed to strengthen abdominal & dorsal muscles. These exercises may also be performed in bed without wearing a corset.
Decubitus ulcers are specific health problems in patients with paraplegia. Decubitus ulcers should be considered during the chronic stage as well. Depression might occur in patients with spinal cord compression, therefore psychological support should be provided for these patients.
Home exercise program
A home exercise program based on the patient’s capacity should be designed in such a way that she or he can understand. A home evaluation is an important aspect of the rehabilitation process, to allow the patients to return home. The main areas of concern in the home evaluation involve the entrances, bedroom, bathroom, kitchen, and general safety issues. The maximum ergonomic changes should be made as possible in the patient’s home environment (toilet, bathroom, bedroom, hallway, etc.) in order to ensure the patient’s independence. Patients’ check-ups and general conditions should be evaluated at regular intervals. Recommendations should be done specifically to facilitate the patient’s activities of daily living in the late stages when the patient can return back to the work.
After the completion of the rehabilitation program in the hospital, the patient is then discharged with a home exercise program and follow-up at regular intervals. In addition to the exercises performed during the subacute and chronic stages, hand & wrist joint exercises, full abduction, extension, and flexion exercises for abdominal, sacrospinal, iliopsoas, gluteus maximus, gluteus minimus, hamstring, & quadriceps muscles, and resistive exercises for oblique abdominal muscles are recommended to be performed at home. Exercises to increase respiratory capacity are performed. Cardiovascular endurance exercises are prescribed after the absolute improvement of vertebral bones. According to the presence of neurological findings, a rehabilitation program was suggested. A neurologic examination & laboratory tests are done at the follow-up visits. A multidisciplinary follow-up program is performed together with infectious diseases, pulmonary diseases, neurosurgery, and orthopedics clinics when needed.
We determined significant improvements in discharge scores of the patients with tuberculosis and brucella after their admission to the hospital when we evaluated motor scores for lower limbs and modified Barthel index (MBI). At the end of the rehabilitation, program patients experienced little pain and were able to perform their daily work with fewer complications. In the final radiological examinations of every patient, degenerative alterations at the pathologic disc space were found to be less than expected. Yen et al evaluated MBI and determined significant improvements in the discharge scores of patients with respect to their admission scores. They also found significant improvements in the discharge scores of the same patients in terms of the motor scores for the lower limbs.
What is the conclusion?
The treatment of spinal tuberculosis illness is difficult and intricate. Spinal tuberculosis can be treated by anybody who can cure Tuberculosis. The contributions of all levels of health service providers are highly important for the management of Pott’s paraplegia, even though the treating surgeon plays the majority of the patient management role. When there is a neurological deficiency or deformity, orthopedic surgeons are typically required. With very few exceptions, managing Pott’s spine and paraplegia based on paraplegia grading are straightforward, rational, effective, and simple to remember. Early diagnosis and efficient therapy are the main initial challenges in the management of the condition. The next specific step is determining the disease-related consequences and making the right choice regarding whether long-term treatment is necessary in addition to surgical procedures. The difficulties in managing long-term chemotherapy, such as side effects & complications from the medication, problems with compliance, socioeconomic variables, & others, are also very important.
FAQ (frequently asked questions)
Is Pott’s disease serious?
Pott disease is the most dangerous form of musculoskeletal tuberculosis because it can lead to bone destruction, deformity, and paraplegia. Pott disease most commonly includes the thoracic and lumbosacral spine. However, published series have shown some variation.
How long does tuberculosis of the spine last?
The progression of spinal tuberculosis is gradual and insidious. The total time period of the illness varies from a few months to a few years, with the average disease duration ranging from 4 to 11 months. Generally, patients seek advice only when there is marked deformity, severe pain, or neurological symptoms.
What is Pott’s disease prognosis?
Pott’s disease responds well to treatment with antitubercular treatment. Improvement in pain and neurological deficits are indicators of response to treatment. The prognosis is good in all patients, if a lack of improvement persists another differential must be considered
Is Pott’s disease curable?
Pott’s disease can be treated through a rigorous medication program or surgery. Pott’s Disease is a result of a lack of treatment over a long period of time; conversely, a lengthy period of medication is frequently needed to fully treat the condition.