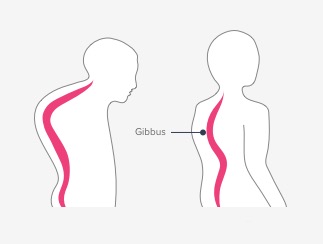
Gibbus Deformity
Table of Contents
What is a Gibbus Deformity?
Gibbus deformity, also known as kyphotic deformity, is a spinal condition characterized by an abnormal, sharp angulation of the spine. It results in a hunchback appearance where the upper back becomes excessively rounded. This deformity is most commonly associated with tuberculosis of the spine, also known as Pott’s disease, although it can also be caused by other conditions such as trauma, tumors, or congenital abnormalities.
In Pott’s spine disease, the tuberculosis infection primarily affects the vertebral bodies, leading to the destruction of the bone. As a result, the affected vertebrae collapse, causing the spine to bend forward sharply at that level. The resulting angular deformity produces the characteristic hump-like appearance seen in the Gibbus deformity.
Definition
Gibbus deformity, also known as kyphotic deformity or kyphosis, refers to an abnormal curvature of the spine characterized by an exaggerated outward rounding of the back.
Introduction
An abnormal curvature of the spine that is characterized by a sharp, angular protrusion at the posterior aspect of one or more vertebrae is referred to as gibbus deformity, which is also referred to as kyphotic deformity or angular kyphosis. This condition brings about a noticeable protuberance or conspicuousness in the mid-back district, regularly seen when an individual is seen from the side. The hump or hunchback is referred to by the Latin word “gibbus.”
The most common underlying cause of gibbus deformity is spinal tuberculosis (also known as Pott’s spine). Congenital spinal abnormalities, spinal trauma or injury, osteoporosis-related fractures, and certain genetic disorders affecting bone development are additional potential causes.
When one or more vertebral bodies collapse or weld together, the deformity occurs, resulting in an exaggerated forward curvature of the spine in the affected area. As a result, the affected vertebrae become compressed and deformed and the spine loses its normal alignment. For people who have a gibbus deformity, this can result in discomfort, decreased mobility, and a number of cosmetic issues.
Determination of gibbus distortion normally includes an intensive actual assessment, clinical history survey, and imaging concentrates like X-beams, figured tomography (CT) checks, or attractive reverberation imaging (X-ray). Treatment choices rely upon the hidden reason, the seriousness of the disfigurement, and related side effects. Moderate administration might include tormenting the executives, non-intrusive treatment, and the utilization of orthotic gadgets to help the spine. In more severe cases, spine stabilization and deformity correction may necessitate surgery.
Individuals with gibbus deformity must collaborate closely with healthcare professionals, including orthopedic specialists, to select the most effective treatment strategy and manage any complications that may arise. Early mediation and legitimate administration can assist with limiting torment, further develop capability, and upgrade the personal satisfaction of those impacted by this condition.
Types of Gibbus Deformity
Gibbus deformity is a spinal deformity characterized by a hump-like appearance caused by a sharp angular curvature of the spine. It is frequently linked to spinal tuberculosis (also known as Pott’s disease) or congenital kyphosis. The following are examples of gibbus deformities:
- Gibbus Tuberculosis: This is the most prevalent form of gibbus deformity and is linked to Pott’s disease, also known as spinal tuberculosis. It happens because of the annihilation of the vertebral bodies by tuberculosis contamination, prompting breakdown and precise disfigurement of the spine.
- Gibbus at birth: Inborn gibbus deformation is available upon entering the world and is brought about by formative irregularities of the spine. It could be connected to conditions like congenital kyphosis or scoliosis.
- Gibbus Post-Traumatic: This kind of gibbus deformity is caused by severe spine injuries like fractures or dislocations. The trauma causes the vertebral bodies to compress or collapse, resulting in an angular deformity.
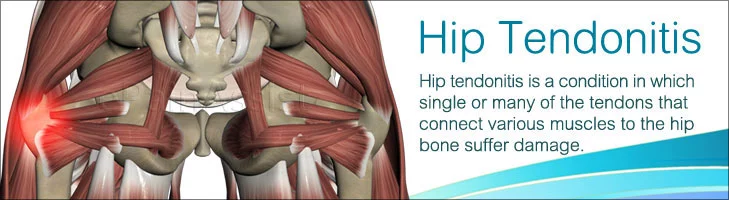
- Gibbus neuromuscular: Gibbus deformity can be caused by neuromuscular conditions that affect the muscles and nerves that control the spine. Muscular dystrophy, spinal muscular atrophy, and cerebral palsy are examples. Progressive curvature and the formation of a gibbus can be caused by imbalance or weakness in the muscles that support the spine.
- Gibbus caused by injury: Gibbus deformities that arise as a result of a medical procedure or intervention are referred to as iatrogenic gibbus deformities. It can happen after spinal surgery, especially if there are problems like hardware failure, implant migration, or not enough correction
for the curve of the spine.
These are some of the more typical forms of gibbus deformity; however, it is essential to keep in mind that each patient’s specific characteristics and underlying conditions may differ. The therapy and the board of gibbus distortion rely upon the hidden reason, the seriousness of the deformation, and individual patient factors, and may incorporate clinical administration, propping, or careful intercession.
Symptoms of Gibbus Deformity
Gibbus distortion is a spinal deformation described by a sharp precise shape in the thoracic or thoracolumbar district of the spine. Trauma, congenital anomalies, and tuberculosis of the spine (Pott’s disease) are all possible causes. The underlying cause and severity of the gibbus deformity can influence the symptoms. Some frequent symptoms include:
- Deformity visible: The most perceptible side effect is a mound or rakish noticeable quality in the upper or center back. The unusual curvature results in a prominent protrusion that resembles a hump.
- Back torment: Chronic back pain is experienced by many people with gibbus deformity. The pain can be mild or severe, and it may get worse if you move or do something that puts pressure on the area.
- Mobility limitations: The deformation can confine spinal development and lead to diminished adaptability in the impacted area. This limitation can make it hard to do things every day and make it harder to twist, bend, or rotate the spine.
- Having difficulty breathing: Gibbus deformity can disrupt the normal function of the respiratory system in severe cases. The lungs and chest cavity may be compressed by the abnormal curvature, resulting in difficulty breathing, shortness of breath, and reduced lung capacity.
- Neurological side effects: Neurological symptoms may result if the deformity puts pressure on the spinal cord or nerve roots. These can incorporate deadness, shivering, or shortcoming in the arms, legs, or different pieces of the body provided by the impacted nerves.
- Slackness and fatigue: Fatigue and muscle weakness can result from gibbus deformity’s persistent pain and limited movement. This can be especially noticeable in the muscles of the back and core.
It’s essential to take note that these side effects can differ contingent on the particular reason and individual conditions. If you have any of these symptoms or think you might have gibbus deformity, you should see a doctor right away for a diagnosis and the best course of treatment.
Causes of Gibbus Deformity
An abnormal curvature of the spine characterized by a sharp angulation or hump-like protrusion in the upper back is referred to as gibbus deformity, which is also known as kyphotic deformity. Numerous underlying conditions and factors may be to blame. Common causes of gibbus deformity include the following:
- M. tuberculosis: The most common cause of gibbus deformity is spinal tuberculosis, also known as Pott’s disease. A gibbus deformity can occur when a TB infection in the spine causes the vertebral bodies to break down and the affected segments to collapse.
- Abnormalities born at birth: Congenital spinal deformities, such as kyphosis or scoliosis, can occur at birth in some people. These circumstances can add to the advancement of gibbus deformation.
- Osteoporosis: Extreme osteoporosis, a condition portrayed by low bone thickness and expanded hazard of breaks, can debilitate the vertebral bodies. Compression fractures are more likely to occur in the weaker vertebrae, which can result in gibbus deformity.
- Trauma: A vertebral collapse and subsequent gibbus deformity can be caused by severe spinal trauma, such as fractures or dislocations. Compression fractures as a result of high-impact injuries or accidents can also cause trauma-induced deformities.
- Tumors: The structural integrity of the vertebral bodies can be impacted by both benign and malignant spinal tumors. Cancer development can prompt vertebral breakdown and resulting gibbus deformation.
- Spondylitis ankylosing: Ankylosing spondylitis is a constant incendiary condition that fundamentally influences the spine. Ankylosis, or the fusion of the spinal joints, and the development of kyphotic deformities, such as the gibbus deformity, can occur over time as a result of the inflammation.
- Neuromuscular problems: Muscle atrophy and muscular dystrophy, two neuromuscular conditions, can make the muscles that support the spine weak and out of balance. This lopsidedness can add to the advancement of gibbus disfigurement.
- Mechanical factors and bad posture: Poor posture for an extended period of time, particularly excessive slouching or forward bending of the spine, can gradually alter the spinal alignment and contribute to gibbus deformity development. Mechanical factors like muscle or spinal imbalances can also play a part.
It’s important to remember that gibbus deformity treatment and management depend on the condition’s severity and underlying cause. To determine the best course of action for each case, a healthcare professional must conduct a comprehensive medical examination.
Diagnosis
Gibbus disfigurement, otherwise called kyphotic deformation or hunchback, alludes to an unusual ebb and flow of the spine that outcomes in a noticeable mound-like appearance in the upper back. Congenital (present at birth) and acquired (developed later in life) abnormalities are two possible causes. A combination of medical history, physical examination, and imaging studies is typically used to make the diagnosis of gibbus deformity. Here is an outline of the demonstrative cycle:
- Medical History: The first step is for the doctor to take a thorough medical history and inquire about any symptoms like back pain, limited range of motion, or changes in posture. Additionally, they will inquire about any pertinent previous medical conditions, injuries, or procedures.
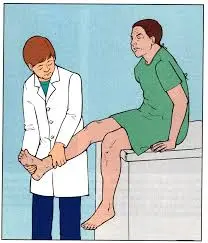
- Examining the body: The curvature of the spine will be evaluated and any associated abnormalities will be discovered during a comprehensive physical examination. The doctor will look at the patient’s posture to see if there are any indications of a visible hump or an abnormally rounded upper back. They might also look for any neurological problems, like weakness in the muscles or loss of sensation.
- Imaging Studies: Imaging studies are typically ordered to confirm the diagnosis and assess the severity of the gibbus deformity. Some examples include:
A. X-rays A detailed view of the vertebral column and the degree of curvature, as well as any structural abnormalities, can be obtained from spine X-rays.
B. Computed Tomography (CT) scan: To obtain cross-sectional images of the spine, a CT scan may be ordered. It allows for a more in-depth look at the bones and can help determine the extent of any bony abnormalities or spinal cord or nerve compression.
C. Magnetic Resonance Imaging, or MRI: An MRI scan uses radio waves and magnetic fields to produce detailed images of the spine and soft tissues that surround it. It may assist in the identification of any underlying causes of the gibbus deformity, such as infections, spinal tumors, or compression of the spinal cord.
- Extra Tests: To determine the underlying cause of the gibbus deformity, additional tests may be required in some instances. Depending on the suspected cause, these may include blood tests, genetic testing, or additional imaging studies like bone scans or ultrasounds.
Based on the underlying cause and severity of the gibbus deformity, a treatment plan can be developed once the diagnosis is confirmed. Treatment choices might incorporate exercise-based recuperation, muscular support, tormenting the executives, careful intercession, or a mix of these methodologies. For a precise diagnosis and individualized treatment recommendations, it is essential to consult a qualified healthcare professional, such as an orthopedic surgeon or spine specialist.
Radiology
A spinal abnormality characterized by a sharp angular kyphosis is referred to as gibbus deformity, which is also known as kyphotic deformity or humpback deformity. It is most frequently associated with Pott’s disease or spinal tuberculosis, but it can also be brought on by congenital anomalies, trauma, or degenerative diseases.
Radiological imaging assumes a vital part in surveying and diagnosing gibbus distortion. Commonly used imaging techniques include:
- X-rays: The first imaging technique used to evaluate the spine is X-rays.
Anteroposterior (AP) and sidelong perspectives on the spine are gotten. In gibbus distortion, the horizontal view is especially significant as it shows the unusual kyphotic ebb and flow. In the case of spinal tuberculosis, X-rays can also assist in determining the underlying cause of the deformity, such as the collapse or destruction of vertebrae.
- Figured Tomography (CT): CT checks give point-by-point cross-sectional pictures of the spine and can be utilized to additionally assess the hard life
systems and the degree of vertebral association. The evaluation of spinal stability and the degree of vertebral destruction and deformity can both benefit from CT scans.
- Imaging with Magnetic Resonance (MRI): X-ray is valuable for assessing the delicate tissues encompassing the spine, including the spinal line, intervertebral circles, tendons, and paraspinal structures. It is able to provide in-depth information regarding the extent of spinal cord compression, the involvement of nerve roots, and the abnormalities of associated soft tissues. MRI is especially useful for determining the extent of disease involvement and identifying infectious or inflammatory processes.
- Scintigraphy of Bones: A nuclear medicine technique known as bone scintigraphy, or a bone scan, can be used to find areas of increased bone turnover or inflammation. In situations where spinal tuberculosis is suspected, it may aid in the identification of active infection or inflammation in the spine.
The underlying cause of gibbus deformity determines the radiological findings. In spinal tuberculosis, for instance, X-beams might show vertebral breakdown, obliteration, or hard sequestration. In contrast to MRI, which can reveal paraspinal abscesses, cord compression, or epidural extension, CT can show the extent of vertebral involvement.
It’s important to remember that a trained radiologist or other medical professional with experience in musculoskeletal imaging should interpret radiological findings. They will think about the patient’s clinical history, actual assessment discoveries, and other significant elements to give an exact conclusion and guide fitting treatment.
Pathology
The spine deformity known as gibbus deformity is distinguished by a sharp, angular protrusion. Most often, it is linked to spinal tuberculosis, also known as Pott’s disease or spinal tuberculosis. The destructive effects of tuberculosis on the vertebral bodies are primarily responsible for the pathology of gibbus deformity.
The pathological process that results in gibbus deformity is broken down as follows:
- Tuberculous Disease: The initial stage involves the hematogenous spread of Mycobacterium tuberculosis from primary tuberculosis focus elsewhere in the body to the spine.
- Vertebral Body Inclusion: The primary area of the vertebral body that is affected by the tuberculosis infection is the anterior part, which results in bone loss and necrosis. The contamination causes the obliteration of the intervertebral circles and contiguous endplates.
- Formation of Tissue by Granulation: Because of the disease, the body structures granulation tissue, which comprises incendiary cells, fibroblasts, and veins. The granulation tissue attempts to contain the infection and serves as a protective response.
- Vertebral Extinction: The annihilation of the vertebral body debilitates its primary trustworthiness, bringing about the breakdown of the impacted vertebra. The gibbus deformity’s angular deformity is caused by this collapse.
- Stability of the Spine As the vertebral bodies break down, the impacted spinal portion loses its soundness, prompting the gradual deterioration of the deformation. Impingement on the spinal cord or nerve roots as a result of the collapse may also result in neurological deficits.
- Formation of a Paravertebral Abscess: Paravertebral abscesses are caused when the tuberculosis infection spreads beyond the vertebral bodies and into the soft tissues that are nearby. These abscesses can additionally add to the distortion and may require careful waste.
If left untreated, the characteristic gibbus deformity will develop over time as a result of the ongoing destruction and collapse of multiple vertebral bodies. The distortion presents as a precise kyphotic bend, most usually influencing the thoracic spine. It can cause severe pain, spinal instability, neurological deficits, cosmetic issues, and neurological problems.
Preventing the deformity’s progression and minimizing its complications necessitates an accurate diagnosis and prompt administration of the appropriate medical treatment, such as antituberculous medication. Stabilizing the spine, decompressing neural structures, and correcting the deformity may sometimes necessitate surgery.
Treatment of Gibbus Deformity
A condition known as gibbus deformity, which is also known as angular kyphosis, is characterized by a hump-like spine deformity. It is most frequently associated with Pott’s disease, spine tuberculosis, but it can also be brought on by congenital anomalies, trauma, or certain metabolic disorders. The underlying cause, severity, and presence of associated symptoms all play a role in the treatment of gibbus deformity.
- Methodical treatment: Conservative treatment may be sufficient when the deformity is mild and does not cause significant symptoms.
This mostly requires a combination of the following:
- Brace work: Wearing spinal support or orthosis to help the spine and forestall further movement of the distortion.
- Exercise therapy: stretches and exercises to strengthen the muscles that support the spine, improve posture, and increase flexibility.
- Torment the executives: treatments or medications to alleviate the deformity’s pain and discomfort.
- Operative treatment: In cases of severe gibbus deformity or when conservative treatment fails to alleviate symptoms, surgery may be required. The specific surgical procedure is determined by a number of factors, including the deformity’s cause and location. Careful choices might include:
- Fusing the spine: To stabilize the spine and correct the deformity, this involves fusing the affected vertebrae together. Bone joins or embeds might be utilized to advance combination.
- Osteoplasty: A wedge osteotomy, in which a wedge-shaped portion of the deformed vertebra is removed to correct the angular kyphosis, may be performed by a surgeon in some instances.
- The instruments: During the fusion process, additional stability and support may be provided by means of metal rods, screws, or other devices.
The patient’s overall health, the severity of the deformity, and the potential risks and benefits of each treatment option should all be taken into consideration when selecting a treatment plan. To figure out the best way to treat gibbus deformity, a spine specialist or orthopedic surgeon needs to do a thorough evaluation.
- Physiotherapy treatment:-
The term “gibbus deformity” refers to an abnormal, kyphotic, angular curvature of the spine that is frequently associated with conditions like “Pott’s disease” or other infections of the spine. By addressing pain relief, improving posture, enhancing mobility, and promoting overall functional well-being, physiotherapy can support the management of gibbus deformity. It means a lot to take note that the essential therapy for gibbus deformation normally includes clinical administration, for example, antitubercular meds or careful intercession, contingent upon the hidden reason and seriousness of the
disfigurement. Physiotherapy can help with rehabilitation and complement these treatments.
The following are some physiotherapy treatments that may be used to treat gibbus deformity:
- Management of pain: Physiotherapists can utilize different strategies to lighten torment related to gibbus disfigurement. Hot/cold therapy, electrical modalities like TENS, ultrasound, and manual therapy techniques like joint mobilization and soft tissue mobilization are all examples of these.
- Correction for posture: In order to slow the deformity’s progression and ease the pain it causes, physiotherapists can concentrate on improving postural alignment and muscle balance. They might offer specific stretches and exercises to lengthen tight muscles and strengthen weak muscles. This
could include practices focusing on the back extensors, muscular strength, and hip flexors, among others. - Exercises for the range of motion: Physiotherapy can incorporate activities pointed toward keeping up with or working on the scope of movement in the spine and adjoining joints. The spine, hips, and shoulders may all benefit from gentle stretching, joint mobilization techniques, and flexibility exercises.
- Stabilizing the core: Strengthening the core muscles, such as the back extensors and deep abdominal muscles, can help improve posture and overall spinal stability. To improve core strength, physiotherapists may recommend specific exercises like planks, bridges, and abdominal bracing.
- Practical preparation: With the right body mechanics and movement strategies, physiotherapists can help people with gibbus deformity perform ADLs and functional tasks. This can assist in maximizing functional independence and minimizing the deformity’s impact on day-to-day activities.
It’s essential to take note that the treatment approach might shift relying upon the singular’s condition, the basic reason for the gibbous disfigurement, and the seriousness of the distortion. A physiotherapist will look at the individual needs of the patient and create a customized treatment plan that addresses their particular situation. Cooperation with other medical care experts, like muscular-trained professionals and irresistible illness-trained professionals, may likewise be important for exhaustive administration.
Summary
Gibbus distortion alludes to a strange ebb and flow of the spine portrayed by a sharp precise conspicuousness in the upper back, normally in the thoracic district. It is frequently associated with spine tuberculosis, also known as Pott’s disease, but it can also be caused by other conditions.
FAQs
What issues does gibbus deformity cause?
Patients with Gibbus deformities are susceptible to paraplegia, myelopathy, and progressive kyphosis if untreated.
What distinguishes kyphosis from gibbus?
Structural kyphosis is a gibbus deformity. The curve is not smooth; it appears sharply angled from behind. A humpback with this malformation could be observed to be more obvious when bending forward. The phrase “extreme” (hyper) curvature” refers to the curvature that is greater than usual.
Describe the Gibbus.
The adjective gibbous derives from the Latin word gibbus, which means “hump.” It became part of Middle English to refer to rounded, convex objects.
What causes Gibbus formation?
Gibbus deformity is most frequently caused by TB osteomyelitis, although it can also be brought on by metabolic conditions or hereditary abnormalities such achondroplasia or cretinism, making it more common in youngsters than in adults.
How do you examine gibbus?
The physician could do Adam’s forward bending test: You sag forward at the waist while doing that. A rounded curve (more suggestive of postural kyphosis) or an angular curve will be looked for by the doctor. When you bend forward, the angular curve, also known as a gibbus deformity, is more obvious.
What is gibbus on the spine?
The collapse of one or more vertebral bodies, which causes kyphosis and is known as a gibbus deformity, is characterised by these anomalies in the vertebrae and is frequently caused by infection, metabolic abnormalities, or congenital defects.