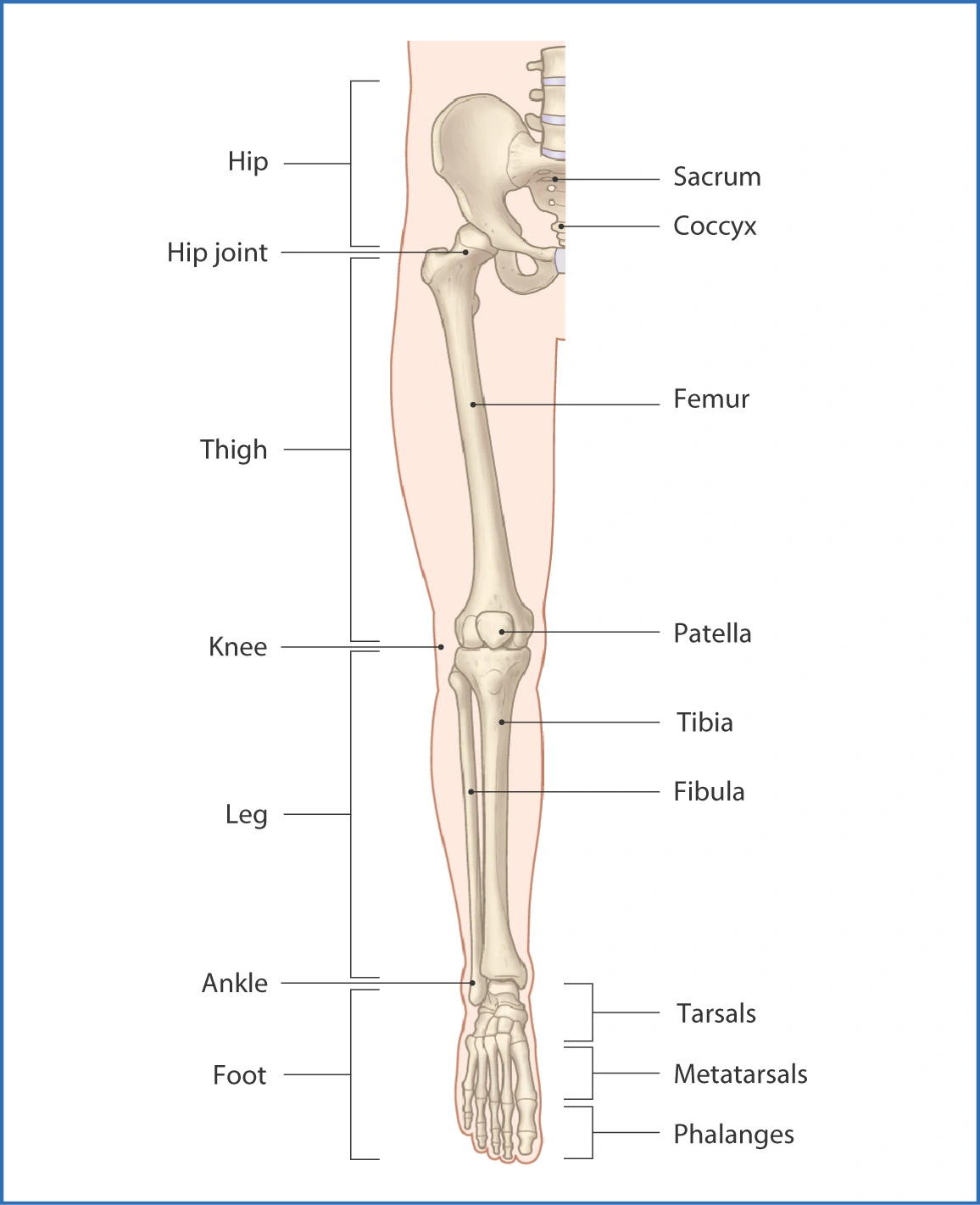
Lower Limb Bones
Table of Contents
Introduction
The lower limb consists of 60 bones, including the femur in the thigh, the tibia and fibula in the lower leg, 7 tarsals in the ankle, 5 metatarsals in the sole of the foot, and phalanges in each toe. These bones work together to provide support, stability, and mobility for walking, running, and other lower-body movements.
The lower limb also consists of various joints, muscles, ligaments, tendons, and cartilage that work together to facilitate movement and maintain stability. These structures enable actions such as walking, running, jumping, squatting, and kicking. They also help absorb shock and distribute forces during weight-bearing activities.
The lower limb is essential for mobility, balance, and stability. It allows us to perform a wide range of activities and plays a crucial role in our daily lives.
Femur bone
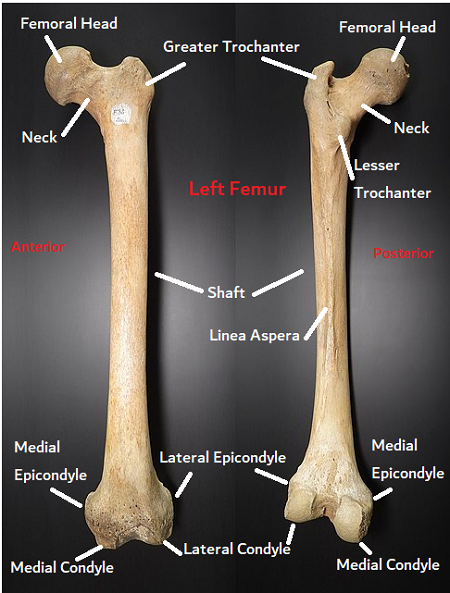
The femur is also called the thigh bone. It is the strongest & longest bone, located in the upper leg and connects the hip joint to the knee joint. The femur consists of several distinct parts that contribute to its function and structure
The structure of the femur allows it to withstand significant forces during weight-bearing activities such as walking, running, and jumping. Its shape and arrangement of different parts contribute to the stability and mobility of the hip and knee joints.
Parts of the bone
- Head: The head of the femur is a rounded structure that forms the ball-shaped portion of the ball-and-socket hip joint. It is covered with articular cartilage, which helps reduce friction and allows for smooth movement within the joint.
- Neck: The neck of the femur is a narrow region that connects the head to the shaft of the bone. It is angled slightly downward and outward, which contributes to the stability and range of motion of the hip joint.
- Greater Trochanter: The greater trochanter is a bony prominence placed on the lateral side of the proximal femur. It serves as an attachment site for various muscles, including those involved in hip abduction and rotation.
- Lesser Trochanter: The lesser trochanter is a smaller bony prominence located on the medial side of the proximal femur, just below the neck. Similar to the greater trochanter, it serves as an attachment site for muscles involved in hip flexion.
- Shaft: The shaft of the femur is the long, cylindrical portion of the bone that extends from the neck to the distal end. It is slightly curved and has a triangular cross-section, which provides strength and stability while minimizing weight.
- Medial and Lateral Condyles: The distal end of the femur features two rounded prominences called condyles. The medial condyle is located on the inner side, while the lateral condyle is on the outer side. These condyles connect the tibia to create the knee joint.
- Intercondylar Fossa: Between the medial and lateral condyles, there is a deep groove called the intercondylar fossa. It accommodates the cruciate ligaments of the knee, which help stabilize the joint during movement.
- Epicondyles: The femur also has two bony projections called epicondyles, located above the condyles. These serve as attachment sites for ligaments and tendons involved in stabilizing the knee joint.
Functions of the bones
The femur bone serves several important functions in the human body:
- Support and Weight Bearing: The femur is responsible for supporting the weight of the upper body and transferring it to the lower limbs. Its length and strength allow it to withstand the forces generated during activities such as walking, running, and jumping.
- Mobility and Range of Motion: The femur plays a crucial role in the mobility and range of motion of the hip joint. The ball-shaped head of the femur fits into the socket of the pelvis, forming a ball-and-socket joint that allows for a wide range of movements, including flexion, extension, abduction, adduction, and rotation.
- Muscle Attachment: The various prominences and projections on the femur serve as attachment sites for muscles involved in hip and knee movement. The greater and lesser trochanters provide attachment points for muscles responsible for hip abduction, rotation, and flexion. The epicondyles serve as attachment sites for ligaments and tendons involved in stabilizing the knee joint.
- Protection: The femur helps protect vital structures within the leg, such as blood vessels and nerves. Its strong and sturdy structure acts as a shield, reducing the risk of injury to these structures.
- Blood Cell Production: The femur contains bone marrow, which is responsible for producing red and white blood cells, as well as platelets. Red blood cells are essential for oxygen transport, while white blood cells help fight off infections and diseases.
- Bone Mineral Storage: Like other bones in the body, the femur serves as a reservoir for important minerals such as calcium and phosphorus. These minerals play a crucial role in maintaining bone strength and density.
Overall, the femur bone is essential for providing support, mobility, protection, and blood cell production in the human body. Its unique structure and functions contribute to the overall strength and functionality of the lower limbs.
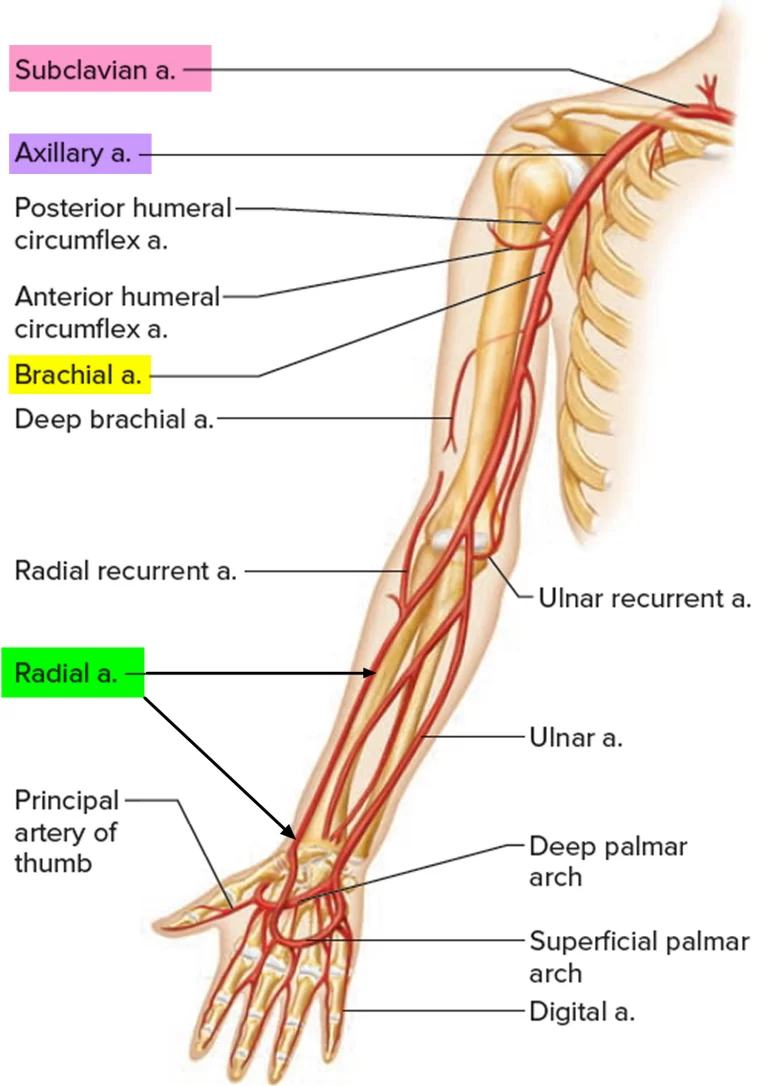
Blood supply of femur bone
The femur bone receives its blood supply from several arteries that branch off from the main arteries in the pelvis and thigh. These arteries include the medial and lateral circumflex femoral arteries, the deep femoral artery, and the nutrient artery.
The medial and lateral circumflex femoral arteries supply blood to the head and neck of the femur. These arteries wrap around the femur and provide a rich blood supply to this region, which is crucial for maintaining the health and integrity of the bone.
The deep femoral artery, also known as the profunda femoris artery, supplies blood to the posterior aspect of the femur. It gives off numerous branches that penetrate into the bone and provide blood to the bone marrow and surrounding tissues.
The nutrient artery is a small branch that enters the femur through a nutrient foramen, which is a small hole in the bone. This artery supplies blood to the inner part of the femur, including the bone marrow.
Additionally, there are numerous smaller arteries that branch off from these main arteries and supply blood to different regions of the femur. These arteries form an extensive network of blood vessels within the bone, ensuring that all areas receive an adequate blood supply.
The blood supply to the femur is essential for maintaining its health and function. It provides oxygen and nutrients to the bone cells, allowing them to carry out their metabolic processes and maintain their integrity. Additionally, the blood supply plays a crucial role in bone healing and repair in case of injury or fracture.
It is important to note that disruptions or injuries to the blood supply of the femur can have serious consequences. For example, if the blood supply to the head and neck of the femur is compromised, it can lead to a condition called avascular necrosis, where the bone tissue dies due to a lack of blood supply. This can result in pain, limited mobility, and eventually, joint degeneration.
Conditions that affect the femur
There are several conditions that can affect the femur bone, each with its own causes, symptoms, and treatments. Here are a few examples:
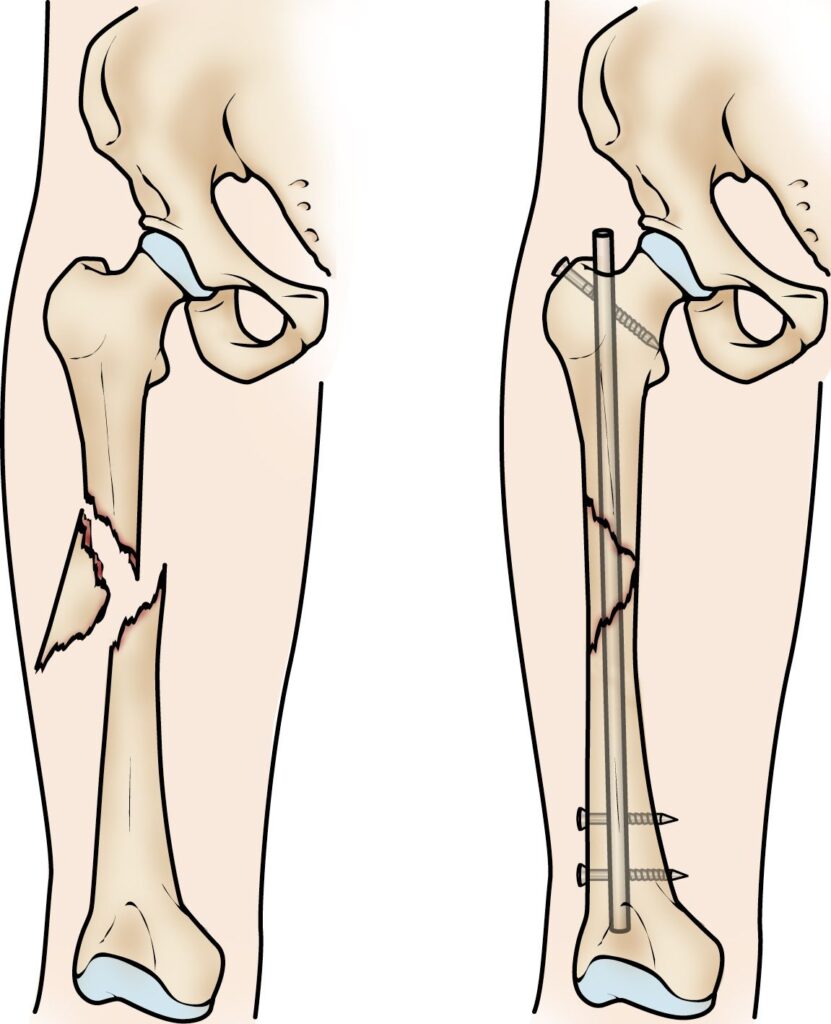
- Fractures: Femur fractures are relatively common and can occur as a result of trauma, such as a car accident or a fall from a height. Fractures can be classified as either traumatic fractures, which occur due to a sudden impact or force, or stress fractures, which develop over time due to repetitive stress on the bone. Treatment for femur fractures typically involves immobilization with a cast or brace, and in severe cases, surgery may be necessary to realign the bone fragments.
- Osteoporosis: Osteoporosis is a condition characterized by weakened bones that are more at risk of fractures. It happens when the body loses too much bone mass or fails to generate enough new bone. Osteoporosis can affect any bone in the body, including the femur. Risk factors for osteoporosis include age, gender (women are more at risk), hormonal changes (such as menopause), and certain medications. Treatment for osteoporosis may involve lifestyle changes, such as diet and exercise, as well as medications to improve bone density.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that commonly affects weight-bearing joints like the hip and knee, including the hip joint where the femur connects. It happens when the protective cartilage that cushions the ends of bones wears down over time, resulting in pain, stiffness, and reduced mobility. Treatment for osteoarthritis of the femur may involve pain management strategies, physical therapy, assistive devices (such as canes or walkers), and in severe cases, joint replacement surgery.
- Avascular Necrosis: Avascular necrosis (AVN), also known as osteonecrosis, is a condition where bone tissue dies due to a lack of blood supply. AVN can affect any bone, including the femur. It is often caused by trauma, such as a fracture or dislocation, or by conditions that disrupt the blood supply to the bone, such as sickle cell disease, alcoholism, or long-term corticosteroid use. Symptoms of AVN may include pain, limited range of motion, and joint stiffness. Treatment options for AVN depend on the severity and location of the affected bone and may include medication, physical therapy, or surgical interventions.
These are just a few examples of conditions that can affect the femur bone. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan if you are experiencing any symptoms or concerns related to your femur bone.
Patella
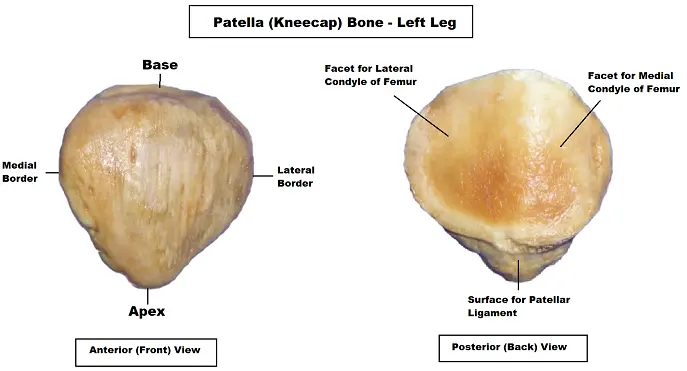
The patella is also known as the kneecap. It is a small, triangular bone placed in front of the knee joint. It plays an important role in the function and stability of the knee joint.
the patella serves to protect the knee joint, improve the mechanical advantage of the thigh muscles, and enhance stability during various movements. It is crucial for proper knee function and plays a significant role in activities that involve lower limb mobility and strength.
Parts of the patella
The patella has several important parts, including:
- Apex: The apex is the pointed lower end of the patella. It is the attachment point for the patellar tendon, which connects the patella to the tibia (shinbone). The patellar tendon helps to transmit forces from the thigh muscles to the lower leg, allowing for movements such as jumping, running, and walking.
- Base: The base is the broad superior end of the patella. It is attached to the quadriceps tendon, which connects the quadriceps muscles (thigh muscles) to the patella. The quadriceps tendon helps to extend the knee joint, allowing for movements such as kicking and straightening the leg.
- Articular Surface: The articular surface of the patella is the smooth, cartilage-covered area on the posterior side of the bone. It articulates with the femur (thighbone) to form the patellofemoral joint. This joint allows for gliding and rotational movements of the patella during knee flexion and extension.
- Medial and Lateral Facets: The articular surface of the patella is divided into two distinct areas called the medial and lateral facets. These facets provide contact points between the patella and the femur, ensuring proper alignment and distribution of forces during knee movement.
Functions of the patella
The patella, or kneecap, serves several important functions in the knee joint:
- Protection: The patella acts as a protective shield for the knee joint. It covers and shields the front of the knee, providing a layer of protection against direct impact or injury. The patella also helps to prevent damage to the underlying structures of the knee, such as the femur, tibia, and ligaments.
- Mechanical Advantage: The patella improves the mechanical advantage of the thigh muscles (quadriceps muscles). When the quadriceps muscle contract, they tug on the patellar tendon, which in turn pulls on the tibia. This mechanism increases the leverage and efficiency of the quadriceps muscles, allowing for more effective extension of the knee joint. This is particularly important during activities that require forceful leg extension, such as jumping or kicking.
- Stabilization: The patella plays a crucial role in stabilizing the knee joint. It helps to maintain proper alignment of the femur and tibia during movement, preventing excessive lateral or rotational movements that could lead to injury or instability. The patella also helps to distribute forces evenly across the knee joint, reducing the risk of localized stress or strain on specific structures.
- Enhancing Joint Function: The patella contributes to the smooth functioning of the knee joint. The articular surface of the patella, along with the corresponding surface on the femur, forms the patellofemoral joint. This joint allows for gliding and rotational movements of the patella during knee flexion and extension. These movements help to improve joint mobility and reduce friction between the patella and femur during knee movements.
- Force Transmission: The patella, along with its associated ligaments and tendons, helps to transmit forces from the thigh muscles to the lower leg. The patellar tendon, which attaches to the tibial tuberosity, acts as a strong connection between the patella and the tibia. This tendon helps to transmit forces generated by the quadriceps muscles during activities such as running, walking, and jumping. By transmitting these forces efficiently, the patella contributes to the overall strength and power of the lower limb.
The patella is a small but crucial bone that plays multiple important roles in the knee joint. It protects the knee, improves mechanical advantage, stabilizes the joint, enhances joint function, and facilitates force transmission. These functions are essential for proper knee function and mobility during various activities.
Blood supply of patella
The patella, like any other bone in the body, requires a blood supply to nourish its cells and maintain its health. The blood supply to the patella comes from several sources.
- Superior Genicular Artery: The superior genicular artery is a branch of the popliteal artery, which is located behind the knee joint. This artery gives rise to branches that supply blood to the upper part of the patella. These branches penetrate the bone through small holes called nutrient foramina and provide oxygen and nutrients to the bone cells.
- Inferior Genicular Artery: The inferior genicular artery is another branch of the popliteal artery that supplies blood to the lower part of the patella. Similar to the superior genicular artery, it gives off branches that enter the bone through nutrient foramina and provide blood to the patellar bone cells.
- Periosteal Blood Vessels: The periosteum is a dense connective tissue membrane that covers the outer surface of bones, including the patella. It contains a network of blood vessels called periosteal blood vessels that supply blood to the outer layers of the patella. These vessels penetrate the bone through small channels in the periosteum and provide nutrients and oxygen to the bone cells.
- Patellar Ligament Blood Supply: The patellar ligament, which connects the patella to the tibia, also has its own blood supply. The blood vessels that supply the ligament can also contribute to the blood supply of the patella, especially in the lower part where the ligament attaches to the tibial tuberosity.
It is important to note that the blood supply to the patella may vary between individuals, and there can be individual variations in the exact pattern and distribution of blood vessels. However, these are the general sources of blood supply to the patella.
Adequate blood supply to the patella is crucial for the maintenance of its health and function. It ensures the delivery of oxygen and nutrients to the bone cells, supports bone remodeling and repair processes and helps in the removal of waste products. Without a proper blood supply, the patella may be at an increased risk of developing conditions such as avascular necrosis (death of bone tissue due to lack of blood supply) or delayed healing of fractures.
Conditions that affect the patella
There are several conditions that can affect the patella, leading to pain, instability, or dysfunction. Here are a few common conditions:

- Patellar Tendinitis: Also known as jumper’s knee, patellar tendinitis is an overuse injury that causes inflammation and irritation of the patellar tendon. This condition is commonly seen in athletes who participate in activities that involve repetitive jumping or running. Symptoms include pain and tenderness around the patellar tendon, especially during physical activity.
- Patellofemoral Pain Syndrome: This condition refers to pain and discomfort around the front of the knee, specifically behind or around the patella. It is often caused by imbalances in muscle strength or tightness, poor alignment of the patella, or overuse. Activities such as running, squatting, or climbing stairs can aggravate the pain. Patellofemoral pain syndrome is commonly seen in young adults and athletes.
- Patellar Dislocation: Patellar dislocation occurs when the patella is forced out of its normal position within the patellofemoral groove. This can happen due to a sudden twisting motion of the knee, direct trauma, or underlying structural abnormalities. Symptoms are joint pain, swelling, and difficulty to moving the knee. Patellar dislocation may require immediate medical attention to relocate the patella and prevent further damage.
- Chondromalacia Patellae: Chondromalacia patellae, also known as the runner’s knee, is a condition characterized by softening and degeneration of the cartilage on the undersurface of the patella. It is often caused by repetitive stress on the knee joint, muscle imbalances, or abnormal patellar tracking. Symptoms include a dull, aching pain behind or around the patella, especially during activities that involve bending or kneeling.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that commonly affects weight-bearing joints, including the knee. Over time, the cartilage that cushions the joint wears away, leading to pain, stiffness, and swelling. Osteoarthritis of the patellofemoral joint can cause pain behind or around the patella, especially during activities that involve bending or squatting.
These are just a few examples of conditions that can affect the patella. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment if you are experiencing any knee pain or dysfunction.
Tibia and Fibula
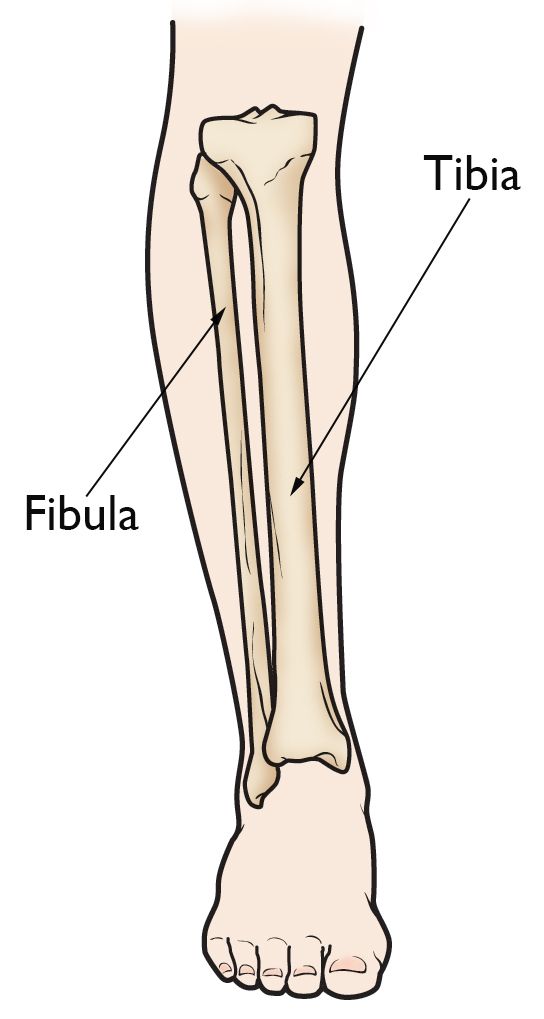
The tibia and fibula are two bones that make up the lower leg. The tibia is the large weight-bearing bone situated on the inner side, while the fibula is the small bone situated on the outer side. Both bones have distinct parts that contribute to their functions of support, stability, and movement.
Parts of the bones
The tibia and fibula are the two long bones present in the lower leg. They run parallel to each other, with the tibia being the larger and stronger bone, and the fibula being thinner and more slender.
- Tibia: The tibia, also known as the shinbone, is the larger of the two bones and is located on the inner side of the leg. It is weight-bearing and plays a crucial role in supporting body weight during activities such as walking, running, and jumping. The tibia consists of several important parts:
- Proximal end: The proximal end of the tibia forms the knee joint with the femur bone of the thigh. It consists of two prominent bony structures called the medial and lateral condyles, which articulate with the corresponding condyles of the femur. The proximal end also has a depression called the intercondylar eminence, which separates the condyles.
- Shaft: The shaft of the tibia is the long, straight portion that extends from the proximal end to the distal end. It is triangular and has three borders – medial, lateral, and posterior. The shaft is responsible for providing stability and strength to the bone.
- Medial malleolus: The medial malleolus is a bony prominence located at the distal end of the tibia on the inner side of the ankle. It serves as an attachment point for ligaments that stabilize the ankle joint.
- Fibula: The fibula is the smaller bone located on the outer side of the leg, running parallel to the tibia. Although it is not directly involved in bearing weight, it plays a vital role in providing support and stability to the leg. The fibula consists of several important parts:
- Head: The head of the fibula is located at the proximal end and articulates with a corresponding surface on the tibia. It forms a joint called the proximal tibiofibular joint, which allows for limited movement between the two bones.
- Shaft: The shaft of the fibula is long and slender, extending from the proximal end to the distal end. It is responsible for providing support and acting as a site for muscle attachment.
- Lateral malleolus: The lateral malleolus is a bony prominence located at the distal end of the fibula on the outer side of the ankle. It serves as an attachment point for ligaments that stabilize the ankle joint.
Functions of the tibia and fibula
The tibia and fibula have distinct functions in the lower leg:
- Tibia:
- Weight-bearing: The tibia is the main bone that tolerates weight. It supports the body’s weight during activities such as walking, running, and jumping.
- Stability: The tibia provides stability to the leg by connecting the knee joint with the ankle joint. It acts as a strong anchor for muscles, tendons, and ligaments, allowing for controlled movement.
- Shock absorption: The tibia helps absorb and distribute forces generated during weight-bearing activities. It has a larger cross-sectional area compared to the fibula, which enhances its ability to withstand impact and reduce stress on the leg.
2. Fibula
- Support: While the fibula is not directly involved in weight-bearing, it plays a crucial role in supporting the leg. It acts as a reinforcement to the tibia and helps distribute forces from the tibia to the foot.
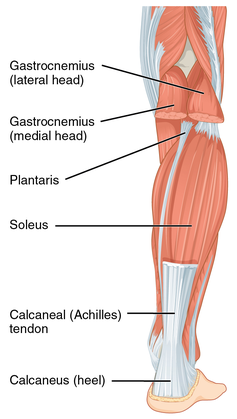
- Muscle attachment: The fibula serves as an attachment site for various muscles in the lower leg. These muscles, such as the calf muscles, help with movements like plantarflexion (pointing the foot downward) and eversion (turning the foot outward).
- Stabilization: The fibula contributes to the stability of the ankle joint by providing support to the lateral (outer) side of the joint. It helps prevent excessive sideways movement of the ankle, reducing the risk of sprains or other injuries.
Overall, the tibia and fibula work together to provide support, stability, and mobility to the lower leg. The tibia bears most of the body’s weight and plays a crucial role in weight-bearing activities, while the fibula supports the tibia and contributes to muscle attachment and ankle stabilization.
Blood supply of tibia and fibula
The blood supply to the tibia and fibula is provided by several arteries that branch off from the main blood vessels in the leg. These arteries ensure that both bones receive adequate oxygen and nutrients for their proper functioning.
- Tibial arteries:
- Anterior tibial artery: This artery originates from the popliteal artery behind the knee and travels down the front of the leg. It gives off branches that supply blood to the muscles, tendons, and ligaments surrounding the tibia and fibula.
- Posterior tibial artery: This artery also arises from the popliteal artery but travels down the back of the leg. It gives off branches that supply blood to the posterior muscles, tendons, and ligaments around the tibia and fibula. It also sends smaller branches to the bone itself.
2. Peroneal artery:
- This artery is a division of the posterior tibial artery. It runs along the outer side of the leg, providing blood supply to the muscles and tissues surrounding the fibula.
These arteries form an extensive network of smaller blood vessels called perforating arteries that penetrate into the bone itself. These vessels supply oxygen and nutrients to the bone cells (osteocytes) and help with bone growth, repair, and remodeling.
Additionally, there are several smaller arteries that contribute to the blood supply of the tibia and fibula, including nutrient arteries. Nutrient arteries enter the bones through small openings called nutrient foramina and provide blood supply to the inner regions of the bones.
The veins accompanying these arteries drain deoxygenated blood from the tibia and fibula back to the heart. The venous drainage follows a similar pattern to the arterial supply, with anterior tibial veins and posterior tibial veins collecting blood from their respective areas.
Overall, the blood supply to the tibia and fibula is essential for maintaining bone health, supporting bone growth and repair, and ensuring proper functioning of the surrounding muscles, tendons, and ligaments.
Conditions that affect the tibia and fibula
There are several conditions that can affect the tibia and fibula, ranging from traumatic injuries to chronic conditions. Here are some common conditions that can affect these bones:
- Fractures: Fractures are breaks or cracks in the bone. They can occur due to trauma, such as a fall or a direct blow to the leg, or due to repetitive stress on the bone. Fractures can be divided in severity, from hairline fractures to very complete breaks. Treatment for fractures may involve immobilization with a cast or brace, surgical fixation with plates and screws, or in severe cases, external fixation devices.
- Stress fractures: Stress fractures are small cracks in the bone that develop due to repetitive stress or overuse. They commonly occur in athletes or individuals who engage in activities that involve repetitive impact, such as running or jumping. Rest, activity modification, and sometimes immobilization are typically recommended for stress fracture healing.
- Osteomyelitis: Osteomyelitis is an infection of the bone, which can affect the tibia and fibula. It can occur due to an open fracture, surgery, or the spread of infection from nearby tissues. Symptoms may involve redness, pain, swelling, and fever. Treatment often involves antibiotics and sometimes surgical debridement to remove infected tissue.
- Osteoporosis: It is a condition characterized by reduced bone density and raising the risk of fractures. While it primarily affects the spine, hips, and wrists, it can also affect the tibia and fibula. Osteoporosis weakens the bones, making them more dangerous fractures. Treatment may involve lifestyle modifications, calcium, and vitamin D supplementation, medications to improve bone density, and fall prevention strategies.
- Osteosarcoma: Osteosarcoma is a type of bone cancer that can affect the tibia and fibula. This condition generally happens in children and young adults. Symptoms may involve swelling, bone pain, and fractures. Treatment typically includes a combination of surgery, radiation therapy, and chemotherapy, radiation therapy.
- Compartment syndrome: Compartment syndrome is a condition characterized by increased pressure within a muscle compartment, which can affect the tibia and fibula. It can occur due to trauma, such as fractures or crush injuries, or due to excessive exercise. Symptoms may include severe pain, swelling, numbness, and decreased range of motion. Immediate medical attention is necessary, as compartment syndrome can lead to tissue damage and nerve injury. Treatment often involves surgical decompression to relieve pressure.
It is important to note that this is not an exhaustive list, and there are other conditions that can affect the tibia and fibula. If you are experiencing any symptoms or have concerns about your leg bones, it is recommended to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Tarsal
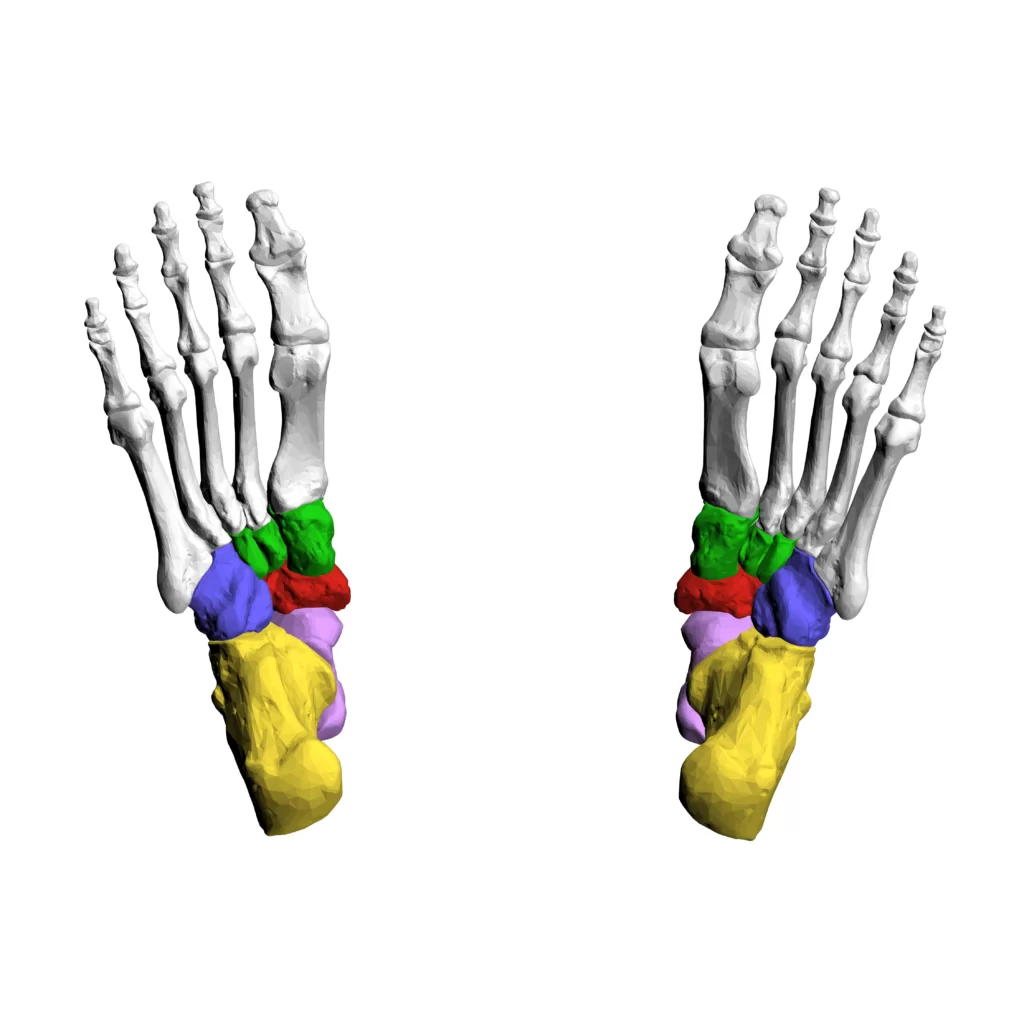
The tarsal bones are a group of seven bones located in the foot, between the tibia and fibula of the lower leg and the metatarsal bones of the midfoot. They play a crucial role in providing stability, support, and flexibility to the foot.
Parts of the tarsal bone
Here are the details of each tarsal bone:
- Calcaneus: The calcaneus, also known as the heel bone, is the largest tarsal bone. It forms the prominence of the heel and provides attachment for several muscles, tendons, and ligaments. The calcaneus transfers the weight of the body from the talus to the ground during walking and running.
- Talus: The talus is a small bone that sits above the calcaneus and forms the lower part of the ankle joint. It connects the leg bones (tibia and fibula) to the foot bones (calcaneus and navicular). The talus allows for up-and-down movement of the foot, enabling actions like pointing and flexing the toes.
- Navicular: The navicular bone is located on the medial (inner) side of the foot, between the talus and the cuneiform bones. It helps support the arches of the foot and provides stability during walking and running.
- Cuboid: The cuboid bone is located on the lateral (outer) side of the foot, in front of the calcaneus. It plays a role in transferring weight from the foot to the toes and helps maintain stability during walking and running.
- Cuneiforms: There are three cuneiform bones: medial cuneiform, intermediate cuneiform, and lateral cuneiform. They are wedge-shaped bones located between the navicular bone and the base of the metatarsal bones. The cuneiforms contribute to maintaining the arches of the foot, providing stability, and facilitating weight distribution.
- Medial cuneiform: The medial cuneiform is the largest and most centrally located of the three cuneiform bones. It articulates with the first metatarsal bone, helping to support the inner arch of the foot.
- Intermediate cuneiform: The intermediate cuneiform is situated in between the lateral and medial cuneiform bones. It articulates with the second metatarsal bone and provides support to the middle part of the foot.
- Lateral cuneiform: The lateral cuneiform is the smallest of the three cuneiform bones. It articulates with the third metatarsal bone and contributes to the stability of the outer arch of the foot.
These tarsal bones are connected by various ligaments, tendons, and joints, allowing for movement and providing stability to the foot. They work together to absorb shock, bear weight, and facilitate movements like walking, running, and jumping.
Functions of the tarsal bones
The tarsal bones have several important functions in the foot:
- Stability: The tarsal bones, along with the ligaments and tendons that connect them, provide stability to the foot. They form a strong framework that supports the weight of the body and helps maintain balance during standing, walking, and running.
- Weight-bearing: The tarsal bones, particularly the calcaneus, bear a significant amount of the body’s weight. When we walk or run, the calcaneus transfers the weight from the talus to the ground, allowing for efficient movement and reducing stress on other structures in the foot.
- Shock absorption: The tarsal bones, along with the surrounding soft tissues, help absorb shock during activities like walking, running, and jumping. They act as a cushion, distributing the forces generated by these activities and protecting the more delicate structures of the foot, such as the joints and cartilage.
- Flexibility: The tarsal bones, especially the talus, and navicular, play a crucial role in foot flexibility. They allow for up-and-down movement of the foot, which is essential for actions like pointing and flexing the toes. This flexibility enables us to adapt to different terrains and perform various movements.
- Arch support: The tarsal bones, along with the ligaments and muscles of the foot, contribute to maintaining the arches of the foot. The arches help distribute weight evenly across the foot, absorb shock, and provide stability during walking and running. The cuneiform bones, in particular, play a significant role in supporting and maintaining the arches.
- Joint articulation: The tarsal bones form several important joints within the foot, such as the ankle joint (formed by the talus and tibia/fibula) and the midfoot joints (formed by the tarsal bones and metatarsal bones). These joints allow for smooth movements and facilitate actions like dorsiflexion (bringing the foot upward) and plantarflexion (pointing the foot downward).
Overall, the tarsal bones are essential for maintaining the structural integrity, stability, and flexibility of the foot. They work in conjunction with other structures in the foot to support our body weight, absorb shock, and enable various movements.
Blood supply of tarsal
The tarsal bones receive their blood supply from several arteries, which provide oxygen and nutrients to the bone tissue. The main arteries involved in the blood supply of the tarsal bones are:
- Dorsalis pedis artery: This artery originates from the anterior tibial artery and runs along the top of the foot. It gives off branches that supply blood to the tarsal bones, including the talus, navicular, and cuneiform bones.
- Posterior tibial artery: This artery is a major branch of the popliteal artery and travels down the back of the leg. It gives off branches, such as the medial and lateral plantar arteries, which supply blood to the hindfoot and midfoot, including the calcaneus and cuboid bones.
- Peroneal artery: This artery is another branch of the posterior tibial artery and runs along the outer side of the leg. It gives off branches that supply blood to the lateral aspect of the foot, including the cuboid bone.
These arteries enter the foot and form an intricate network of smaller vessels that supply blood to the tarsal bones. Within the bones, the blood supply reaches the bone tissue through small arteries called nutrient arteries. These arteries enter the bones through small openings called nutrient foramina and branch out to supply blood to different areas of the bone.
The blood supply to the tarsal bones is crucial for their health and proper functioning. It provides oxygen and nutrients to the bone cells, allowing them to carry out metabolic processes and maintain their structural integrity. Additionally, a healthy blood supply helps in the healing of any injuries or fractures that may occur in the tarsal bones.
It’s important to note that disruptions or blockages in the blood supply to the tarsal bones can lead to avascular necrosis, a condition where bone tissue dies due to a lack of blood flow. This can result in pain, deformity, and loss of function in the affected bones.
Conditions that affect tarsal bones
There are several conditions that can affect the tarsal bones, leading to pain, deformity, and loss of function. Some of these conditions include:
- Tarsal coalition: This is a condition where two or more tarsal bones are abnormally fused together. It can occur as a result of abnormal development during childhood or due to trauma. Tarsal coalition can cause foot pain, stiffness, and difficulty with walking or running.
- Tarsal tunnel syndrome: Similar to carpal tunnel syndrome in the wrist, tarsal tunnel syndrome involves compression of the tibial nerve as it passes through a narrow tunnel in the ankle. This can result in pain, numbness, tingling, and weakness in the foot and ankle.
- Stress fractures: Stress fractures are small cracks or breaks in the bone that occur due to repetitive stress or overuse. They commonly affect the metatarsal bones in the foot, including the tarsal bones. Stress fractures can cause localized pain, swelling, and difficulty with weight-bearing activities.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that commonly affects weight-bearing joints such as the ankles and feet. It happens when the protective cartilage that a type of cushions the ends of bones breaks down with time. Osteoarthritis of the tarsal bones can cause pain, stiffness, swelling, and difficulty with movement.
- Rheumatoid arthritis: Rheumatoid arthritis is an autoimmune disease that causes chronic inflammation and destruction of joint tissues. It can affect multiple joints in the body, including the tarsal joints. Rheumatoid arthritis can cause pain, swelling, stiffness, and deformity in the affected joints.
- Gout: Gout is a type of arthritis that happens because of the creation of uric acid crystals in the joints. It commonly affects the big toe joint but can also involve the tarsal joints. Gout attacks can cause sudden and severe pain, swelling, redness, and warmth in the affected joint.
- Osteochondritis dissecans: This condition involves the detachment of a piece of bone and cartilage from the joint surface. It can occur in the tarsal bones, causing pain, swelling, and limited joint movement.
These are just a few examples of conditions that can affect the tarsal bones. Treatment for these conditions may include conservative measures such as rest, physical therapy, medication, and orthotics. In some cases, surgery may be necessary to repair or remove damaged bone or tissue.
Metatarsals
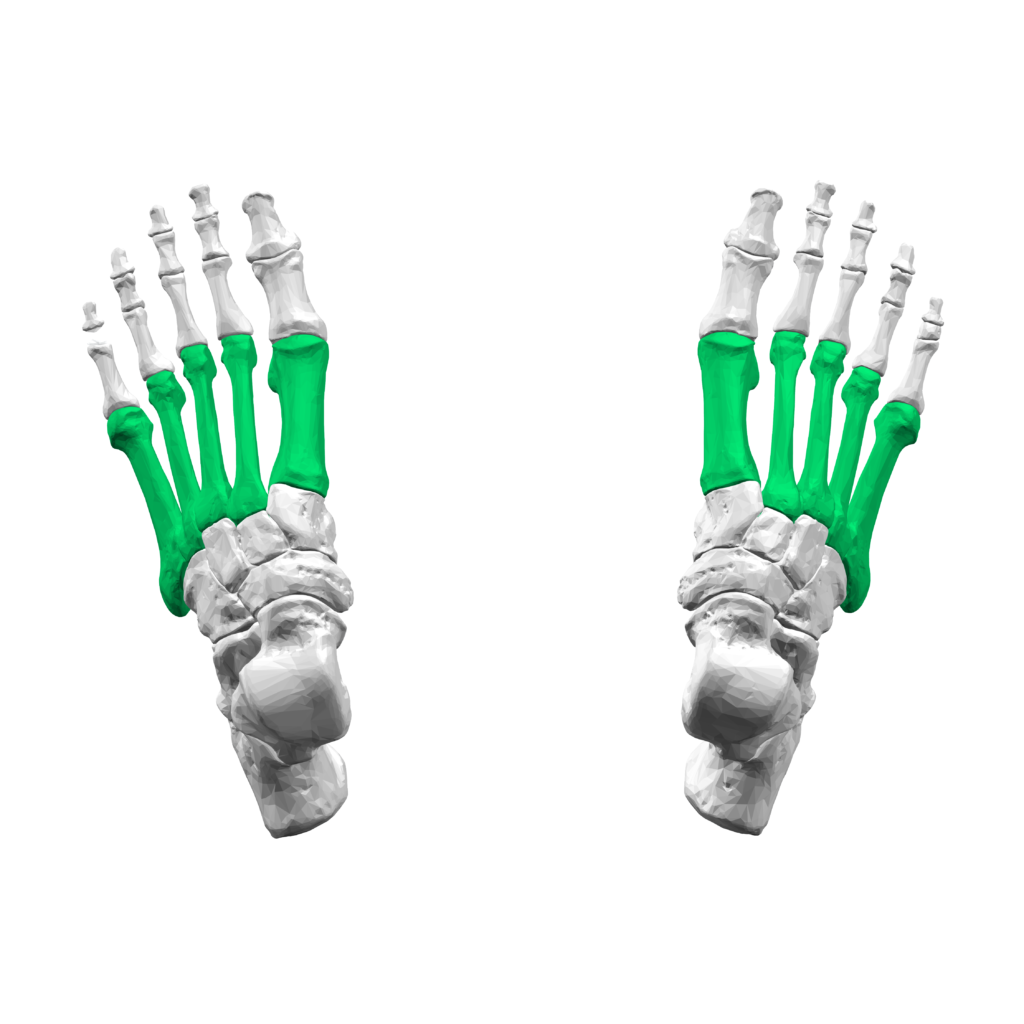
The metatarsal bones are a group of five long bones located in the midfoot region of the foot. They are numbered from one to five, starting from the big toe side (first metatarsal) to the little toe side (fifth metatarsal). These bones play a crucial role in supporting the body’s weight during standing, walking, and running.
The metatarsal bones collectively form an arch-like structure called the transverse arch, which runs across the width of the foot. This arch helps in weight-bearing and shock absorption, allowing for efficient movement and stability.
Additionally, various ligaments, tendons, and muscles attach to the metatarsals, providing stability, flexibility, and control of foot movements. The metatarsal bones also contain nutrient foramina, which are small openings that allow blood vessels and nerves to enter and supply the bones.
Injuries or conditions that affect the metatarsal bones can lead to pain, swelling, deformities, and difficulty in walking or bearing weight on the affected foot. Common injuries include fractures, stress fractures, and metatarsalgia (pain in the ball of the foot). Proper diagnosis and treatment by a healthcare professional are essential to ensure proper healing and restoration of foot function.
Parts of metatarsal bones
Each metatarsal bone consists of three main parts:
- Base: The base is the proximal end of the metatarsal bone, which connects to the tarsal bones in the midfoot. It is wider and thicker than the shaft and provides stability and support to the foot. The base articulates with the corresponding tarsal bone and forms a joint called the tarsometatarsal joint.
- Shaft: The shaft is the long, slender middle part of the metatarsal bone. It is slightly curved and tapers from the base to the head. The shaft provides flexibility and acts as a lever during walking and running movements. It also serves as an attachment site for various muscles, tendons, and ligaments that help in foot movement and stability.
- Head: The head is the distal end of the metatarsal bone, which connects to the phalanges (toe bones). It is wider and more rounded than the base and has a smooth articular surface that forms a joint with the proximal phalanx of each toe. The heads of the metatarsals bear a significant amount of pressure during walking and running, distributing the weight evenly across the foot.
Functions of the metatarsal bones
The metatarsal bones have several important functions in the foot:
- Weight-bearing: The metatarsals bear a significant amount of the body’s weight during standing, walking, and running. They provide a stable foundation for the foot and help distribute the weight evenly across the foot to prevent excessive pressure on any one area.
- Shock absorption: The metatarsals, along with the arches of the foot, play a crucial role in absorbing and dissipating the impact forces generated during activities like walking or running. The structure and flexibility of the metatarsals allow them to bend and absorb shock, reducing the stress on other structures such as joints and ligaments.
- Foot movement: The metatarsals, particularly their shafts, act as levers during walking and running movements. They provide a platform for the muscles, tendons, and ligaments in the foot to generate and control movement. The flexibility of the metatarsals allows for smooth and efficient foot motion, facilitating activities like pushing off the ground and propelling the body forward.
- Stability: The metatarsals, along with the surrounding ligaments and tendons, help maintain the stability of the foot. They provide a solid base for the foot to support the body’s weight and resist excessive movements or forces that could lead to injury or instability.
- Attachment site for muscles and tendons: The metatarsals serve as attachment points for various muscles and tendons in the foot. These structures help control and stabilize foot movements, allowing for precise control during activities like balancing, walking on uneven surfaces, or engaging in sports.
- Joint formation: The base and head of each metatarsal bone form joints with other bones in the foot. These joints allow for smooth articulation and movement between different parts of the foot, enhancing overall foot function.
- Arch support: The metatarsals, along with other bones and ligaments in the foot, contribute to the formation of the transverse and longitudinal arches of the foot. These arches provide structural support and distribute weight evenly, enhancing stability and shock absorption.
In summary, the metatarsal bones play a crucial role in supporting the body’s weight, absorbing shock, facilitating foot movement, providing stability, and serving as attachment points for muscles and tendons. Their proper function is essential for maintaining foot health and overall mobility.
Blood supply of metatarsal
The metatarsal bones receive their blood supply from a network of arteries and veins that run along the length of the foot. The main arteries that supply blood to the metatarsals are the dorsal metatarsal arteries and the plantar metatarsal arteries.
The dorsal metatarsal arteries arise from the dorsalis pedis artery, which is a branch of the anterior tibial artery. These arteries run along the top of the foot, between the metatarsal bones, and give off branches that supply blood to the dorsal aspect of the metatarsals.
The plantar metatarsal arteries arise from the medial and lateral plantar arteries, which are branches of the posterior tibial artery. These arteries run along the bottom of the foot, between the metatarsal bones, and give off branches that supply blood to the plantar aspect of the metatarsals.
As the arteries travel along the foot, they divide into smaller branches that penetrate the bone and provide blood supply to the medullary cavity (the central part of the bone) as well as the outer cortical bone (the hard outer layer of the bone).
In addition to these arteries, there are also numerous small branches that arise from adjacent arteries and contribute to the blood supply of the metatarsals. These include branches from the arcuate artery, which is a branch of the dorsalis pedis artery, and branches from the deep plantar arch, which is formed by the anastomosis (connection) between the dorsalis pedis artery and the lateral plantar artery.
The blood supply to the metatarsal bones is important for their nourishment and maintenance. It provides oxygen and nutrients to the bone cells, allowing for growth, repair, and remodeling. Adequate blood supply is also crucial for bone healing after fractures or other injuries.
In addition to the arterial blood supply, the metatarsal bones also have a venous drainage system that allows for the removal of waste products and deoxygenated blood. The veins accompanying the arteries in the foot drain into the dorsal and plantar venous arches, which eventually join to form the great saphenous vein or the small saphenous vein.
Overall, the blood supply of the metatarsal bones is a complex network of arteries and veins that ensures proper nourishment and oxygenation of the bones, supporting their function and health.
Conditions that affect metatarsals
There are several conditions that can affect the metatarsal bones, causing pain and discomfort. Here are a few examples:
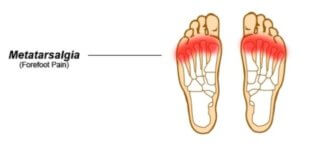
- Metatarsalgia: This is a general term used to describe pain in the ball of the foot, which is often caused by inflammation or irritation of the metatarsal heads (the rounded ends of the metatarsal bones). It can be caused by excessive pressure on the metatarsals, such as from wearing high-heeled shoes or participating in high-impact activities.
- Stress fractures: Stress fractures are small cracks in the bone that occur due to repetitive stress or overuse. They commonly occur in the metatarsal bones, particularly the second and third metatarsals. Athletes who engage in activities that involve repetitive impact, such as running or jumping, are at a higher risk of developing stress fractures.
- Morton’s neuroma: This condition involves the thickening of the tissue around the nerves that run between the metatarsal heads. It often affects the nerve between the third and fourth metatarsals, causing pain, tingling, or numbness in the ball of the foot. It is commonly associated with wearing tight or narrow shoes.
- Metatarsal fractures: Fractures can occur in any of the metatarsal bones due to trauma or injury. They can range from hairline fractures to complete breaks. Fractures can cause severe pain, swelling, and difficulty walking. Treatment may involve immobilization, casting, or surgery depending on the severity of the fracture.
- Sesamoiditis: The sesamoid bones are small bones located beneath the first metatarsal head. Sesamoiditis refers to inflammation or irritation of these bones, often caused by repetitive pressure or overuse. It can result in pain and tenderness in the ball of the foot, particularly beneath the big toe.
- Freiberg’s disease: This condition involves the death of bone tissue in the metatarsal heads, usually affecting the second metatarsal. It can be caused by trauma or repetitive stress and can lead to pain, stiffness, and limited range of motion in the affected joint.
Treatment for these conditions may vary depending on the severity and underlying cause. It may include rest, ice, elevation, pain medication, physical therapy, orthotics, or in some cases, surgery. Proper diagnosis and treatment are important to alleviate symptoms, promote healing, and prevent further complications.
Phalanx
The phalanges are long bones that have a shaft or body, which is cylindrical in shape. The shaft is composed of compact bone tissue, which provides strength and support. At each end of the shaft, there is an expanded region called the epiphysis. The epiphyses are covered with articular cartilage, which allows for smooth movement and reduces friction at the joints.
The phalanges also have several bony processes and structures that serve various functions. For example, there are tubercles and ridges on the surfaces of the bones that provide attachment points for ligaments, tendons, and muscles. These structures help to stabilize the toes and allow for movement and flexibility.
Overall, the phalanges play a crucial role in providing support, balance, and mobility to the foot. They work together with the metatarsal bones and other structures to bear weight, absorb impact, and facilitate walking, running, and other activities.
Parts of phalanx
The bones that make up the toes are called phalanges. Each toe, except for the big toe, consists of three phalanges, while the big toe only has two. The phalanges are named based on their position from the proximal end (closest to the foot) to the distal end (farthest from the foot).
- Proximal phalanx: This is the first phalanx closest to the metatarsal bone. It is relatively thicker and longer than the other two phalanges in each toe. At the metatarsophalangeal joint, the proximal phalanx joins the metatarsal bone.
- Middle phalanx: This is the second phalanx in each toe, located between the proximal and distal phalanges. It is smaller and shorter than the proximal phalanx. The middle phalanx connects to the proximal phalanx through the interphalangeal joint.
- Distal phalanx: This is the third and final phalanx in each toe. It is the smallest and thinnest of the three phalanges. The distal phalanx forms the tip of the toe and provides support for the nail. It connects to the middle phalanx through another interphalangeal joint.
Functions of the phalanx
The phalanges have several important functions in the foot:
- Support and Weight Bearing: The phalanges, along with the metatarsal bones, form the framework of the toes and provide support for the body’s weight. They help distribute the weight evenly across the foot, allowing for balance and stability.
- Mobility and Flexibility: The phalanges are essential for toe movement and flexibility. They allow for a wide range of motions, including bending, extending, and gripping. This mobility is crucial for activities such as walking, running, jumping, and maintaining balance.
- Shock Absorption: The phalanges, particularly the proximal phalanx, play a role in absorbing shock and protecting the foot from impact. When walking or running, the toes help to cushion the foot by absorbing and dispersing the forces generated during each step.
- Grip and Manipulation: The phalanges, especially the distal phalanx, are involved in gripping and manipulating objects. They provide strength and dexterity to the toes, allowing for tasks such as picking up small objects or maintaining balance on uneven surfaces.
- Nail Support: The distal phalanx forms the tip of the toe and provides support for the nail. It helps protect the sensitive tissues underneath the nail and maintains its shape and structure.
- Joint Stability: The phalanges articulate with other bones through various joints, including the metatarsophalangeal joint and interphalangeal joints. These joints allow for movement while providing stability and preventing excessive motion or dislocation.
- Attachment Points: The surfaces of the phalanges have tubercles, ridges, and other bony processes that serve as attachment points for ligaments, tendons, and muscles. These structures help stabilize the toes and allow for coordinated movement.
- Sensory Feedback: The phalanges contain numerous sensory receptors, such as nerve endings and pressure receptors. These receptors provide feedback to the brain about the position, pressure, and movement of the toes, contributing to proprioception (awareness of body position) and tactile sensation.
Overall, the phalanges are essential for the proper functioning of the foot, enabling support, balance, mobility, and manipulation. They work in conjunction with other bones, muscles, ligaments, and tendons to facilitate various activities and movements.
Blood supply of phalanx
The blood supply to the phalanges of the foot is provided by a network of arteries and veins.
Arteries: The main arteries supplying the phalanges are the digital arteries, which branch off from the dorsal and plantar metatarsal arteries. These arteries run along the sides of the toes and give off smaller branches that penetrate into the bones. The digital arteries supply oxygenated blood to the phalanges, ensuring their proper function and nourishment.
Veins: The veins of the phalanges accompany the arteries and drain deoxygenated blood away from the toes. They form a network of superficial and deep veins that ultimately join larger veins in the foot, such as the dorsal venous arch and plantar venous arch.
Capillaries: The arteries and veins are joined by microscopic blood tubes called capillaries. They form an intricate network within the phalanges, allowing for the exchange of oxygen, nutrients, and waste products between the blood and surrounding tissues.
Lymphatic System: The phalanges also have a lymphatic system that helps drain excess fluid and waste products from the tissues. Lymphatic vessels accompany the blood vessels and carry lymph (a clear fluid) back to lymph nodes for filtration and immune response.
Nerves: Nerves accompany the blood vessels in the phalanges, providing sensory innervation and motor control to the toes. These nerves transmit signals related to touch, temperature, pain, and proprioception, contributing to overall foot function and awareness.
The blood supply to the phalanges is crucial for maintaining their health, supporting tissue repair, and facilitating proper function. Any disruption or compromise in blood flow can lead to various conditions, such as poor wound healing, bone necrosis, or nerve damage.
Conditions that affect phalanx
There are several conditions that can affect the phalanges of the foot. Here are a few examples:
- Fractures: Phalangeal fractures are common and can occur due to trauma or repetitive stress. Fractures can disrupt the blood supply to the phalanges, leading to impaired healing and potential complications such as nonunion or avascular necrosis.
- Osteoarthritis: It is a degenerative joint disorder that has an impact on the phalanges. It occurs when the cartilage that cushions the joints wears down, leading to pain, stiffness, and reduced range of motion. The compromised blood supply to the phalanges can contribute to the progression of osteoarthritis.
- Gout: Gout is a type of arthritis that happens to the creation of uric acid crystals in the joints. When it affects the phalanges, it can cause severe pain, swelling, and redness. The inflammation associated with gout can also affect the blood vessels, further compromising blood flow to the phalanges.
- Peripheral artery disease (PAD): PAD is a condition characterized by narrowed or blocked arteries that reduce blood flow to the extremities, including the phalanges. Symptoms may include pain, cramping, and weakness in the toes and feet. Reduced blood supply can lead to tissue damage and slow wound healing.
- Diabetic neuropathy: Diabetes can cause nerve damage, known as neuropathy, which can affect the phalanges. Diabetic neuropathy can lead to loss of sensation, tingling, and pain in the toes. The compromised blood supply can further contribute to nerve damage and increase the risk of foot ulcers and infections.
- Raynaud’s disease: Raynaud’s disease is a condition characterized by episodes of reduced blood flow to the extremities, typically triggered by cold temperatures or stress. When it affects the toes, it can cause them to turn white, blue, and then red as blood flow is restored. The reduced blood supply can lead to pain and tissue damage in severe cases.
These are just a few examples of conditions that can affect the phalanges of the foot. It is important to seek medical attention if you experience any symptoms or have concerns about the health of your toes.
Physiotherapy treatment
Physiotherapy treatment for lower limb conditions involves a comprehensive approach to address the underlying issues, alleviate pain, improve mobility, and enhance overall function. The specific treatment plan will depend on the individual’s condition and needs, but here are some common techniques and interventions used in physiotherapy for lower limb conditions:
- Manual therapy: This involves hands-on techniques such as joint mobilization, soft tissue mobilization, and stretching to restore normal joint and soft tissue mobility. Manual therapy can help reduce pain, improve range of motion, and promote healing.
- Exercise therapy: Therapeutic exercises are prescribed to strengthen muscles, improve flexibility, and enhance stability and balance. These exercises may include stretching, strengthening, and proprioceptive training to address muscle imbalances, improve gait patterns, and promote functional movements.
- Gait training: Gait training focuses on improving the individual’s ability to walk properly. It may involve correcting abnormal walking patterns, adjusting stride length and foot placement, and enhancing balance and coordination. Gait training can be particularly beneficial for individuals with conditions affecting the phalanges as it helps optimize foot function.
- Orthotics and footwear advice: Physiotherapists may assess the need for orthotic devices or recommend appropriate footwear to provide support, alignment, and cushioning to the feet. Orthotics can help correct foot biomechanics, redistribute pressure, and alleviate symptoms related to various foot conditions.
- Pain management techniques: Physiotherapists may utilize modalities such as heat or cold therapy, ultrasound, electrical stimulation, or acupuncture to help manage pain and reduce inflammation in the lower limbs. These techniques can provide temporary relief and facilitate the healing process.
- Education and self-management: Physiotherapists play a crucial role in educating individuals about their condition, providing advice on activity modification, self-care strategies, and preventive measures. They may also teach proper body mechanics and ergonomics to minimize stress on the lower limbs and promote optimal function.
- Functional training: As the individual progresses in their rehabilitation, functional training is incorporated to simulate real-life activities and improve their ability to perform daily tasks or return to sports or recreational activities. This may involve specific exercises or drills tailored to the individual’s goals and functional needs.
It is important to note that physiotherapy treatment for lower limb conditions is highly individualized and may vary depending on the specific condition, severity of symptoms, and individual goals. A qualified physiotherapist will assess and design a personalized treatment plan to address the unique needs of each individual.
Exercise for lower limb
Exercise therapy for lower limb conditions aims to improve strength, flexibility, stability, and overall function of the muscles and joints in the lower limbs. The specific exercises prescribed will depend on the individual’s condition and needs, but here are some common exercises used in physiotherapy for lower limb conditions:

Stretching exercises: Stretching helps improve flexibility and range of motion in the muscles and joints of the lower limbs. It can be particularly beneficial for conditions such as tight calf muscles, hamstring strains, or hip flexor tightness. Common stretching exercises may include calf stretches, hamstring stretches, quadriceps stretches, hip flexor stretches, and ankle mobility exercises.
Strengthening exercises: Strengthening exercises target the muscles of the lower limbs to improve their ability to support and stabilize the joints. These exercises can help address muscle imbalances, weakness, or instability that may contribute to lower limb conditions. Examples of strengthening exercises may include squats, lunges, leg presses, step-ups, calf raises, hip abduction/adduction exercises, and toe raises.
Proprioceptive training: Proprioceptive exercises focus on improving balance, coordination, and proprioception (the body’s sense of joint position and movement). These exercises can be beneficial for individuals with conditions affecting their ability to maintain balance or control movements in the lower limbs. Proprioceptive training exercises may involve standing on one leg, using balance boards or unstable surfaces, or performing dynamic movements while maintaining balance.
Functional exercises: Functional exercises aim to simulate real-life activities and movements to improve the individual’s ability to perform daily tasks or return to sports or recreational activities. These exercises are tailored to the individual’s specific goals and functional needs. Examples of functional exercises may include stair climbing, squats with weights, hopping or jumping exercises, or sport-specific drills.

Core strengthening: Core strengthening exercises target the muscles of the abdomen, lower back, and pelvis, which plays a crucial role in providing stability and support to the lower limbs. Strengthening the core can help improve overall lower limb function and reduce the risk of injuries. Common core strengthening exercises may include planks, bridges, Russian twists, or bird dogs.
It is important to perform these exercises under the guidance of a qualified physiotherapist to ensure proper technique, progression, and safety. The physiotherapist will assess the individual’s condition, develop a personalized exercise program, and provide instructions on how to perform the exercises correctly. They may also incorporate other techniques such as resistance training, balance training, or plyometric exercises based on the individual’s specific needs and goals. Regular adherence to the prescribed exercise program is essential for achieving optimal outcomes in lower limb rehabilitation.
FAQs
Some common conditions and injuries that can affect the lower limbs include fractures, sprains, strains, arthritis, tendonitis, plantar fasciitis, shin splints, and various musculoskeletal disorders.
To prevent lower limb injuries, it is important to maintain a healthy lifestyle, including regular exercise to strengthen the muscles and improve flexibility. Wearing appropriate footwear, using proper techniques during physical activities, and avoiding overuse or repetitive stress on the lower limbs can also help prevent injuries.
Yes, there are several exercises that can help strengthen and improve flexibility in the lower limbs. Some examples include squats, lunges, calf raises, leg presses, hamstring curls, and various stretching exercises targeting the hips, thighs, and calves.
Yes, obesity can have a significant impact on the lower limbs. Excess weight places increased stress on the joints and muscles of the lower limbs, which can lead to various conditions such as osteoarthritis, plantar fasciitis, and increased risk of fractures.
Yes, poor posture can affect the lower limbs. Incorrect alignment of the spine and pelvis can lead to imbalances in the muscles and joints of the lower limbs, causing pain, discomfort, and potential injury.
It is advisable to seek medical attention if you experience severe pain, swelling, inability to bear weight on the affected limb, deformity, or if the pain persists or worsens despite rest and home remedies. A healthcare professional can provide an accurate proper diagnosis and advise accurate treatment.