Osteochondritis dissecans
Table of Contents
What is a Osteochondritis dissecans?
Osteochondritis dissecans (os-tee-o-kon-DRY-tis DIS-uh-kanz) is a joint condition in which bone underneath the cartilage of a joint dies due to lack of blood flow. This bone and cartilage can then break loose, causing pain and possibly hindering joint motion.
Osteochondritis dissecans occurs most often in children and adolescents. It can cause symptoms either after an injury to a joint or after several months of activity, especially high-impact activity such as jumping and running, that affects the joint. The condition occurs most commonly in the knee,
Anatomy of OCD:
OCD mostly affects the femoral condyles of the knee. The femoral condyle is the rounded end of the lower thighbone, or femur. Each knee has two femoral condyles, referred to as the medial femoral condyle (on the inside of the knee) and the lateral femoral condyle (on the outside). Like most joint surfaces, the femoral condyles are covered in articular cartilage.
Articular cartilage is a smooth, rubbery covering that allows the bones of a joint to slide smoothly against one another. The problem occurs where the cartilage of the knee attaches to the bone underneath. The area of bone just under the cartilage surface is injured, leading to damage to the blood vessels of the bone. Without blood flow, the area of damaged bone actually dies.
This area of dead bone can be seen on an X-ray and is sometimes referred to as the: The lesions usually occur in the part of the joint that holds most of the body’s weight. This means that the problem area is under constant stress and doesn’t get time to heal. It also means that the lesions cause pain and problems when walking and putting weight on the knee. It is more common for the lesions to occur on the medial femoral condyle, because the inside of the knee bears more weight.
Stages of Osteochondritis dissecans (OCD):

Stage one: ischemic osteonecrose begin to arise in a part of the subchondral bone, because the tissue is not well vascularized.
Stage two: a subchondral osteonecrose.
Stage three: partially detached lesions, a dissecans ‘in situ’.
Stage four: ‘Dissecans’, this is the loosening of the affected bone fragment and the corresponding cartilage of the articular surface. This fragment falls between the moving parts of the knee joint and blocks it. A ‘joint mouse’ is the bone fragment that roams in the joint, because it moves and it is white
What are the Signs and symptoms of Osteochondritis dissecans?
inflammation, swelling, and soreness in the joint
catching and locking in the joint during movement
reduced range of movement in the joint
crepitus, a grating, cracking, or popping sound when moving the joint
weakness in the joint
limping
effusion, or abnormal collection of fluid in the joint area, leading to swelling
pain, especially after physical activity
stiffness after a period of inactivity
tenderness
Which are the Causes of Osteochondritis Dissecans?
Trauma or repetitive stress injury in an active, athletic, and growing child or adolescent may cause subchondral bone disturbance or overlying cartilage damage.
Disruption of a tenuous blood supply with ensuing vascular compromise to the subchondral area is another etiologic theory.
OCD is more common in growing children.
Diagnosis:
x-rays :
X-rays show lucency of the ossification front in juveniles. In older people, the lesion typically appears as an area of osteosclerotic bone with a radiolucent line between the osteochondral defect and the epiphysis. The visibility of the lesion depends on its location and on the amount of knee flexion used. Harding described the lateral X-ray as a method to identify the site of an OCD lesion.[36]
Magnetic resonance imaging (MRI) :
MRI is useful for staging OCD lesions, evaluating the integrity of the joint surface, and distinguishing normal variants of bone formation from OCD by showing bone and cartilage edema in the area of the irregularity. MRI provides information regarding features of the articular cartilage and bone under the cartilage, including edema, fractures, fluid interfaces, articular surface integrity, and fragment displacement.[37][38] A low T1 and high T2 signal at the fragment interface is seen in active lesions. This indicates an unstable lesion or recent microfractures.[30] While MRI and arthroscopy have a close correlation, X-ray films tend to be less inductive of similar MRI results.[38]
Computed tomography (CT) scans and Technetium-99m bone scans :
CT scan are also sometimes used to monitor the progress of treatment. Unlike plain radiographs (X-rays), CT scans and MRI scans can show the exact location and extent of the lesion.[39] Technetium bone scans can detect regional blood flow and the amount of osseous uptake. Both of these seem to be closely correlated to the potential for healing in the fragment
Treatment of Osteochondritis dissecans
Non-surgical Treatment:
Resting the elbow
Physical therapy
Splint or brace
Cortisone injection
Surgical treatment:
Drilling. Your doctor will use a drill to make a small hole in the affected area. This encourages new blood vessels to form, increasing blood flow to the area and helping it heal.
Pinning. This involves inserting pins and screws to hold the lesion of a joint in place.
Grafting. Your doctor takes bone or cartilage from other areas of your body and places it in the damaged area, grafting new bone or cartilage onto the damaged area.
Physiotherapy treatment in Osteochondritis dissecans:
ice and heat, to aid in pain management.
Modalities – iontophoresis
1)STATIC QUADRICEPS EXERCISE :

Lay on your back. Place a rolled up towel or a small foam roller beneath the knee. Activate the thigh muscles in order to straighten the knee and hold the contraction for 5 seconds. Release. Repeat 10 times on each side.
2)Knee Bending :

Bend your knee and hip and bring back to starting point.
3)sitting quats:
sit with good posture in a chair. Straighten one of your legs, hold for a slow count to 10 and then slowly lower your leg. Repeat 10 times with each leg.
4)STRAIGHT LEG RAISING :-
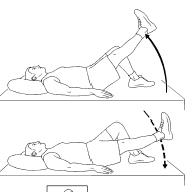
Lay down and bend one of your legs at the knee. Hold your other leg straight and lift your foot just off your bed or floor. Hold for a slow count of five, then lower.
5)Side Leg Raises :

Lie on one side with your legs stacked. Bend the bottom leg for support. Straighten the top leg and raise it to 45 degrees. Hold for 5 seconds, lower and relax briefly, then repeat 10-15 times. Switch sides and start over.
6)Prone Knee Bending::-

Lie on stomach and bend the knee and bring to starting position
7)Prone Straight Leg Raises :
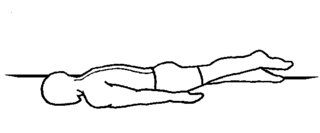
Lie on your stomach with your legs straight. Tighten the muscles in your bottom and the hamstring of one leg, and lift toward the ceiling. Hold 3-5 seconds, lower, and repeat. Do 10-15 lifts and switch sides.
8)squats :
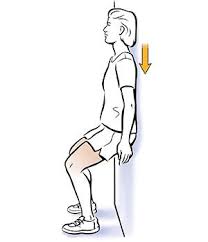
Lean against a wall or a door, so that your feet are about a foot away from you.
Slide your body downward while keeping your back against the wall.
Hold for three seconds, then return back to an upright position.

Lie on the floor or bed with both legs bent.
Slowly lift one leg, still bent, and bring your knee back toward your chest.
Link your hands behind your thigh, not your knee, and straighten your leg.
Pull your straight leg back toward your head until you feel the stretch.
Hold for 30 to 60 seconds, then slowly bend your knee and lower your leg back to the floor.
10)Stationary Bike :
Biking is a good way to increase strength and range of motion. Make sure you have the right positioning of the legs. At the bottom of the pedal stroke, the bend in the knee should be 15 degrees. Start with 10 minutes and slowly increase your time.
How to Prevent Osteochondritis dissecans?
Adolescents participating in organized sports might benefit from education on the risks to their joints associated with overuse. Learning the proper mechanics and techniques of their sport, using the proper protective gear, and participating in strength training and stability training exercises can help reduce the chance of injury.




One Comment