Upper Limb Bones
Table of Contents
Introduction
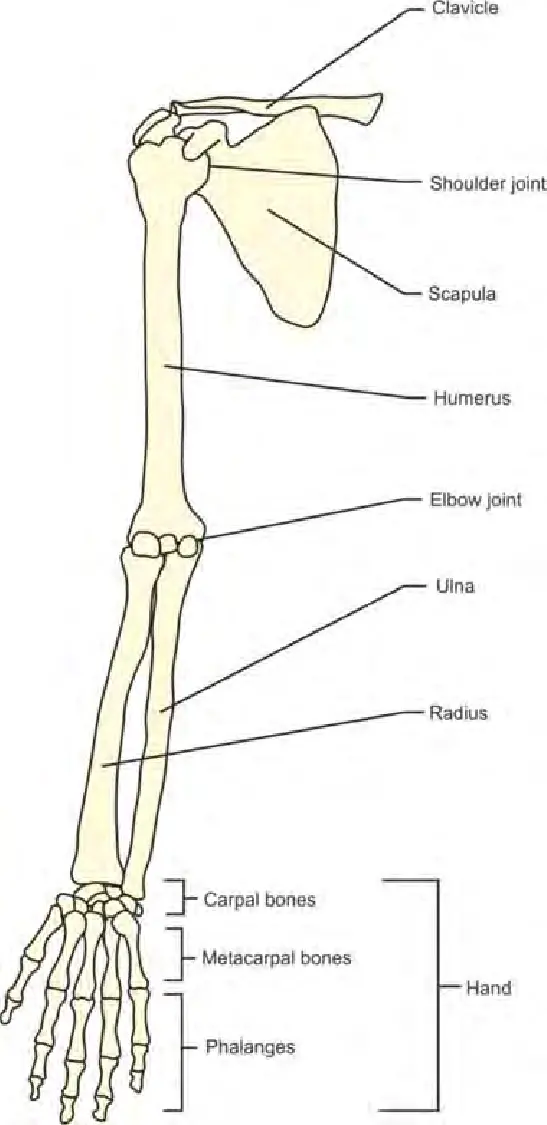
The upper limb bones, also known as the bones of the upper extremity, form the framework and support for the upper limbs of the human body. They play a crucial role in providing structural stability, facilitating movement, and allowing for interaction with the surrounding environment.
The upper limb consists of several major bones, including the humerus, radius, ulna, carpals, metacarpals, and phalanges. Each bone has its own unique characteristics and functions.
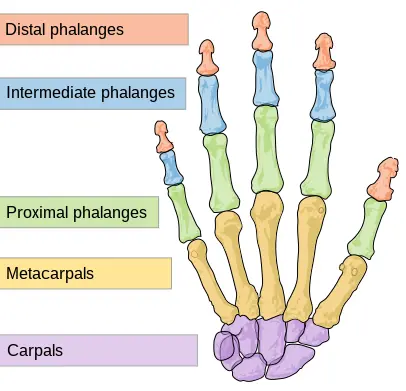
There are a total of 30 bones present in each upper limb. The humerus is the single bone of the upper arm, the ulna is located medially, and the radius is located laterally. These are the paired bones of the forearm. The bottom of the hand involves 8 bones, which are called the carpal bone, and the palm of the hand is created of 5 bones, which are called the metacarpal bone. The fingers and thumb include a total of 14 bones, that of which is a phalanx bone of the hand.
Humerus
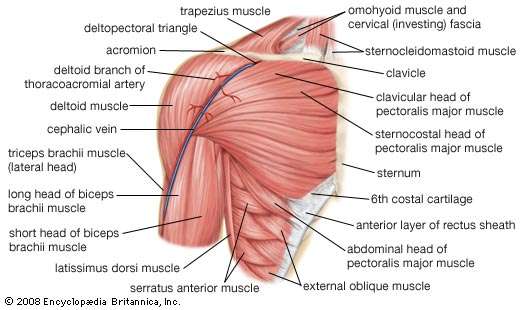
The humerus bone has a complex structure with various anatomical features that contribute to its function. It provides support and stability to the upper limb, allows for a wide range of movements at the shoulder and elbow joints, and serves as an attachment site for numerous muscles involved in arm and forearm movements.
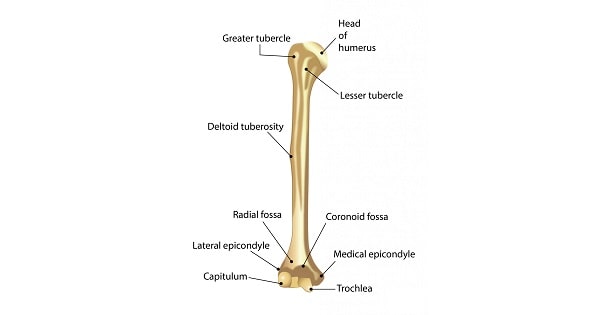
Parts of the humerus
The humerus bone is the long bone located in the upper arm, between the shoulder and the elbow. It is the largest bone in the upper limb and plays a crucial role in the movement and stability of the arm.
- Head: The proximal end of the humerus has a rounded structure called the head. It articulates with the glenoid cavity of the scapula, forming the shoulder joint (glenohumeral joint). The head of the humerus is covered with smooth articular cartilage to reduce friction during movement.
- Greater and Lesser Tubercles: These are two bony projections located on the anterior surface of the proximal humerus. The greater tubercle is larger and serves as an attachment site for muscles of the rotator cuff, which stabilize the shoulder joint. The rotator cuff muscles involve the teres minor, supraspinatus, infraspinatus, and subscapularis. The lesser tubercle is smaller and lies on the front of the humerus, just below the greater tubercle. It also serves as an attachment site for muscles involved in shoulder movement.
- Anatomical and Surgical Neck: The neck of the humerus is a constriction just below the head. The anatomical neck is the slightly narrower region, while the surgical neck is a common site for fractures. The anatomical neck provides an attachment site for ligaments and joint capsules that help stabilize the shoulder joint.
- Deltoid Tuberosity: On the lateral side of the humerus, about halfway down its length, there is a roughened area called deltoid tuberosity. It serves as an attachment site for the deltoid muscle, which is responsible for lifting the arm. The deltoid muscle covers the shoulder joint and helps with various movements of the arm.
- Shaft: The shaft of the humerus is long and cylindrical, extending from the tubercles to the distal end. It is slightly curved and has three borders: anterior, lateral, and medial. These borders provide attachment sites for muscles and serve as landmarks for surgical procedures.
- Medial and Lateral Epicondyles: These are bony projections located at the distal end of the humerus. The medial epicondyle is larger and can be felt on the inner side of the elbow. It serves as an attachment site for muscles involved in flexing the wrist and fingers, such as the flexor carpi radialis and pronator teres. The lateral epicondyle is smaller and can be felt on the outer side of the elbow. It serves as an attachment site for muscles involved in extending the wrist and fingers, such as the extensor carpi radialis brevis and extensor carpi radialis longus.
- Trochlea and Capitulum: These are two distinct condyles located at the distal end of the humerus. The trochlea is a spool-shaped structure that articulates with the ulna bone of the forearm, forming the elbow joint. It gives permission for flexion and extension motion of the forearm. The capitulum is a rounded structure located on the lateral side of the trochlea, which articulates with the radius bone of the forearm. It allows for rotational movements of the forearm, such as supination and pronation.
- Olecranon Fossa: This is a deep depression placed on the posterior surface of the distal humerus, just over the trochlea. It accommodates the olecranon process of the ulna when the arm is extended. The olecranon process forms the bony prominence of the elbow.
Functions of the humerus
The humerus bone plays a very important role in the movement and stability of the arm. It serves as a structural support for the upper limb and provides attachment sites for muscles involved in arm and forearm movements.
One of the main functions of the humerus bone is to form the shoulder joint, also known as the glenohumeral joint. The head of the humerus articulates with the glenoid cavity of the scapula, allowing for a wide range of movements such as flexion, extension, abduction, adduction, and rotation of the arm. The smooth articular cartilage covering the head of the humerus reduces friction during these movements.
The greater and lesser tubercles on the anterior surface of the proximal humerus serve as attachment sites for the muscles of the rotator cuff. The rotator cuff muscles, including the supraspinatus, infraspinatus, teres minor, and subscapularis, help stabilize the shoulder joint and facilitate its movements.
The anatomical and surgical necks of the humerus provide attachment sites for ligaments and joint capsules that help stabilize the shoulder joint. Fractures commonly occur at the surgical neck, which can impact the stability and function of the arm.
The deltoid tuberosity, situated on the lateral side of the humerus, works as a connection site for the deltoid muscle. The deltoid muscle covers the shoulder joint and is responsible for lifting the arm and various movements of the arm.
The shaft of the humerus, extending from the tubercles to the distal end, provides support and structure to the bone. Its three borders (anterior, lateral, and medial) serve as attachment sites for muscles and landmarks for surgical procedures.
At the distal end of the humerus, the medial and lateral epicondyles serve as attachment sites for muscles involved in flexing and extending the wrist and fingers. The medial epicondyle is larger and can be felt on the inner side of the elbow, while the lateral epicondyle is smaller and can be felt on the outer side of the elbow.
The trochlea and capitulum, two distinct condyles at the distal end of the humerus, articulate with the ulna and radius bones of the forearm, respectively. The trochlea gives permission for flexion and extension motion of the forearm, while the capitulum allows for rotational movements such as supination and pronation.
Finally, the olecranon fossa, located on the posterior surface of the distal humerus, accommodates the olecranon process of the ulna when the arm is extended. The olecranon process forms the bony prominence of the elbow.
In summary, the humerus bone’s functions include providing support and stability to the upper limb, allowing for a wide range of movements at the shoulder and elbow joints, and serving as an attachment site for numerous muscles involved in arm and forearm movements.
Conditions that occur at the humerus
There are several conditions that can affect the humerus bone, ranging from fractures and dislocations to infections and tumors. Here are a few examples:

- Fractures: Fractures of the humerus bone can occur due to trauma, such as falls or direct blows to the arm. These fractures can be classified as proximal (near the shoulder), shaft (middle portion), or distal (near the elbow) fractures. Treatment for humerus fractures depends on the location and severity of the fracture and may involve casting, splinting, or surgical intervention.
- Dislocations: Dislocations of the humerus bone occur when the bone is forced out of its normal position in the joint. This can happen as a result of trauma or during sports activities. Shoulder dislocations are the most common type and often require relocation of the joint and immobilization to allow for healing.
- Osteomyelitis: Osteomyelitis is an infection of the bone that can affect the humerus bone. It can occur through direct contamination, such as from an open fracture or surgery, or through bloodstream spread from another infected site. Symptoms may include pain, swelling, redness, and fever. Treatment usually involves antibiotics and, in severe cases, surgical debridement.
- Osteosarcoma: Osteosarcoma is a type of bone cancer that can develop in the humerus bone. It typically affects children and young adults and presents with bone pain, swelling, and a mass or lump in the affected area. Treatment may include radiation therapy, chemotherapy, and surgical removal of the tumor.
- Rotator cuff tears: A rotator cuff is a group of muscles and tendons that are around the shoulder joint and useful in its stability and movement. Tears in the rotator cuff can occur due to repetitive use or acute trauma, leading to pain, weakness, and limited range of motion. Treatment may involve physical therapy, anti-inflammatory medications, and in some cases, surgery.
These are just a few examples of conditions that can affect the humerus bone. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan for any specific condition or injury.
Blood supply
The blood supply to the humerus bone, which is the upper arm bone, is provided by several arteries. These arteries include the brachial artery, the profunda brachii artery, and the nutrient artery.
The brachial artery is the main artery that supplies blood to the upper arm. It arises from the axillary artery in the armpit region and continues down the arm along the medial side. The brachial artery gives off branches along its course, which supply blood to various structures in the arm, including the humerus bone. These branches include the nutrient artery, muscular branches, and collateral branches.
The nutrient artery is a small branch of the brachial artery that enters the humerus bone through a small hole called the nutrient foramen. It travels through the medullary canal of the humerus, providing blood supply to the bone marrow and inner layers of the bone. This artery helps in nourishing and maintaining the health of the humerus bone.
The profunda brachii artery is another important artery that contributes to the blood supply of the humerus bone. It arises from the brachial artery in the upper arm region and descends along with the radial nerve in a groove on the back of the humerus called the radial groove. The profunda brachii artery gives off branches that supply blood to the muscles surrounding the humerus bone. These branches also contribute to the blood supply of the bone itself.
In addition to these arteries, there are also collateral branches that arise from other arteries in the arm and provide additional blood supply to the humerus bone. These collateral branches help ensure adequate blood flow to the bone in case of any blockages or disruptions in the main arteries.
Overall, the blood supply to the humerus bone is crucial for its growth, repair, and overall function. Adequate blood flow ensures that the bone receives oxygen and nutrients necessary for its metabolic processes and helps in maintaining its structural integrity.
Ulna and Radius
Parts of the bones
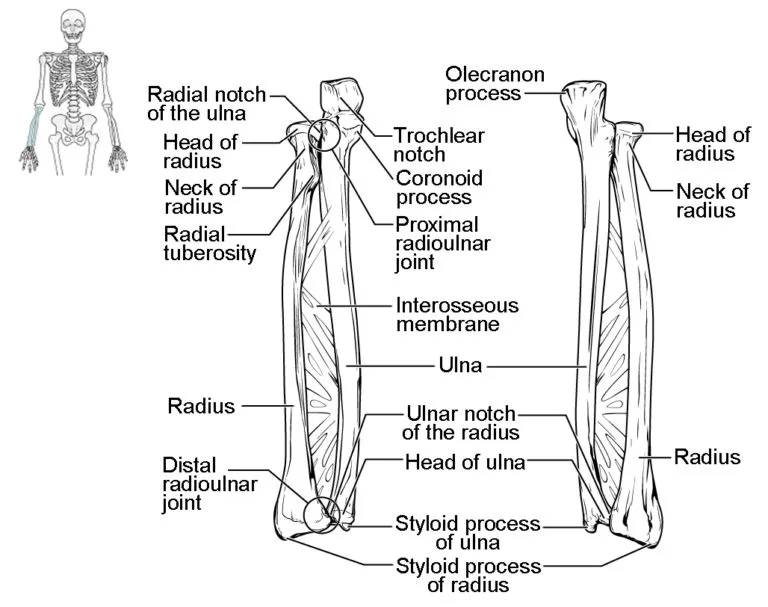
The ulna and radius bones of the forearm work together to allow for a variety of movements, including flexion and extension at the elbow joint, as well as rotational movements of the forearm. They also provide support and stability to the wrist joint through their respective styloid processes.
The ulna and radius are the two bones that create the forearm. They run parallel to each other and are connected by the interosseous membrane, a fibrous tissue that helps to stabilize and support the bones.
The radius is located on the lateral side of the forearm, which is the side of the thumb. It is shorter and smaller compared to the ulna. The proximal end of the radius has a disc-shaped structure called the radial head. This head articulates with the capitulum of the humerus, forming the elbow joint. The radial head allows for rotational movements of the forearm, such as supination (turning the palm upward) and pronation (turning the palm downward).
The shaft of the radius is thin and curved. It becomes wider towards its distal end. At the distal end, there is a bony prominence called the styloid process. This can be felt on the lateral side of the wrist. Ligaments attach to the styloid process, providing stability to the wrist joint.
On the other hand, the ulna is located on the medial side of the forearm, which is the side of the pinky finger. It is longer and larger compared to the radius. The proximal end of the ulna has a hook-like structure called the olecranon process. This process forms the bony prominence of the elbow. When the arm is extended, the olecranon process fits into the olecranon fossa of the humerus, providing stability to the elbow joint.
Below the olecranon process, there is a depression called the trochlear notch. This notch articulates with the trochlea of the humerus, forming a hinge joint at the elbow. This joint allows for flexion (bending) and extension (straightening) movements of the forearm.
The shaft of the ulna is triangular in shape and becomes progressively thinner towards its distal end. At the distal end, there is a bony prominence called the styloid process. This can be felt on the medial side of the wrist. Similar to the radius, ligaments attach to the styloid process of the ulna, providing stability to the wrist joint.
Functions of the bones
The radius and ulna are the two long bones found in the forearm. They run parallel to each other and are connected by a joint called the proximal radioulnar joint at the elbow, and another joint called the distal radioulnar joint at the wrist.
- Support and Structure: The radius and ulna provide structural support to the forearm, allowing it to move and function properly. They help maintain the overall shape and stability of the arm, enabling us to perform various activities such as lifting, pushing, and pulling.
- Movement: The radius and ulna bones play a crucial role in the movement of the forearm and hand. The elbow joint, formed by the articulation of the humerus with the ulna, allows for flexion and extension of the forearm. This movement is essential for performing tasks such as bending the elbow to lift an object or extending it to push something away.
- Pronation and Supination: The radius bone is responsible for pronation and supination movements of the forearm. Pronation refers to the rotation of the forearm inwards, where the palm faces downwards, while supination is the opposite movement, where the palm faces upwards. These movements are important for activities like turning a doorknob, using a screwdriver or pouring liquid from a container.
- Transfer of Forces: The radius bone plays a significant role in transferring forces from the hand to the elbow joint. It acts as a lever during actions such as throwing a ball or swinging a racket. The radial tuberosity, a bony prominence on the radius, serves as an attachment site for muscles involved in these forceful movements.
- Protection: The ulna bone provides protection to vital structures within the forearm. It acts as a shield for the nerves, blood vessels, and muscles present in the region. The olecranon process, a bony prominence at the back of the ulna, forms the tip of the elbow and serves as a protective cover for the joint.
- Blood Cell Production: The bone marrow within the radius and ulna bones is responsible for the production of blood cells, including red blood cells, white blood cells, and platelets. This hematopoietic function is crucial for maintaining a healthy immune system and ensuring proper oxygenation of tissues throughout the body.
In summary, the radius and ulna bones work together to provide structural support, enable movement, transfer forces, protect vital structures, and facilitate blood cell production. They are essential for various activities and functions of the forearm and hand.
Conditions occur at the bone
There are several conditions that can affect the radius and ulna bones. Here are a few examples:
- Fractures: Fractures are breaks in the bone and can occur in either the radius or ulna or both. Fractures can be caused by trauma, such as a fall or a direct blow to the forearm, or by repetitive stress injuries. Fractures can vary in severity, from hairline fractures to complete breaks, and may require immobilization, casting, or surgical intervention to heal properly.
- Dislocations: Dislocations happen when the bones in a joint are forced out of their original positions. In the case of the radius and ulna, a dislocation can happen at the proximal radioulnar joint or the distal radioulnar joint. Dislocations can be caused by trauma or excessive force applied to the joint, and they often result in pain, swelling, and limited range of motion. Treatment typically involves manual reduction of the joint followed by immobilization and rehabilitation.
- Osteoporosis: Osteoporosis is a condition characterized by a decrease in bone density and strength, making the bones more susceptible to fractures. While osteoporosis can affect any bone in the body, it commonly affects the radius and ulna due to its weight-bearing function in the forearm. Treatment for osteoporosis may involve lifestyle modifications, medication, and calcium and vitamin D supplementation to improve bone health.
- Osteomyelitis: Osteomyelitis is an infection of the bone that can affect any bone in the body, including the radius and ulna. It is usually caused by bacteria entering the bone through an open fracture, surgical procedure, or bloodstream infection. Symptoms include pain, swelling, redness, and fever. Treatment typically involves intravenous antibiotics and sometimes surgical intervention to remove infected tissue.
- Arthritis: Arthritis is a condition characterized by inflammation of the joints, which can lead to pain, stiffness, and limited range of motion. Rheumatoid arthritis and osteoarthritis are two common types of arthritis that can affect the radius and ulna joints. Treatment for arthritis may involve medication, physical therapy, joint injections, or in severe cases, surgical intervention.
It is important to note that these are just a few examples of conditions that can affect the radius and ulna bones. There are many other conditions and injuries that can impact the health and function of these bones. If you suspect you have a condition affecting your radius and ulna, it is recommended to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Blood supply
The radius and ulna bones are mainly blood provided by branches of the radial and ulnar arteries.
- Radial Artery: The radial artery is the main artery that supplies blood to the radius bone. It originates from the brachial artery in the upper arm and travels down the forearm on the thumb side (radial side). Along its course, the radial artery gives off several branches that contribute to the blood supply of the radius bone. These branches include the anterior interosseous artery, which runs along the interosseous membrane between the radius and ulna bones, and the posterior interosseous artery, which supplies the back of the forearm.
- Ulnar Artery: The ulnar artery is responsible for supplying blood to the ulna bone. It also originates from the brachial artery in the upper arm but travels down the forearm on the pinky side (ulnar side). Like the radial artery, the ulnar artery gives off branches that contribute to the blood supply of the ulna bone. These branches include the anterior ulnar recurrent artery, which travels along the front of the forearm, and the posterior ulnar recurrent artery, which travels along the back of the forearm.
The blood supply to the radius and ulna bones is important for their nourishment and maintenance of healthy bone tissue. Adequate blood flow ensures that oxygen and nutrients are delivered to the bones, promoting their growth, repair, and overall health. Impaired blood supply to these bones can result in decreased bone density, delayed healing of fractures, and increased risk of bone-related complications.
It is worth noting that in addition to these arterial branches, there are also accompanying veins and a network of smaller vessels that provide venous drainage and further support the blood supply to the radius and ulna bones.
Overall, a well-functioning blood supply is crucial for maintaining the health and integrity of the radius and ulna bones, enabling them to perform their important roles in the forearm and upper limb.
Carpal bones
These carpal bones are interconnected by strong ligaments, forming a complex structure that allows for a wide range of movements in the wrist joint. They also provide attachment sites for various muscles and tendons, enabling the movement of the hand and fingers.
Parts of the bones
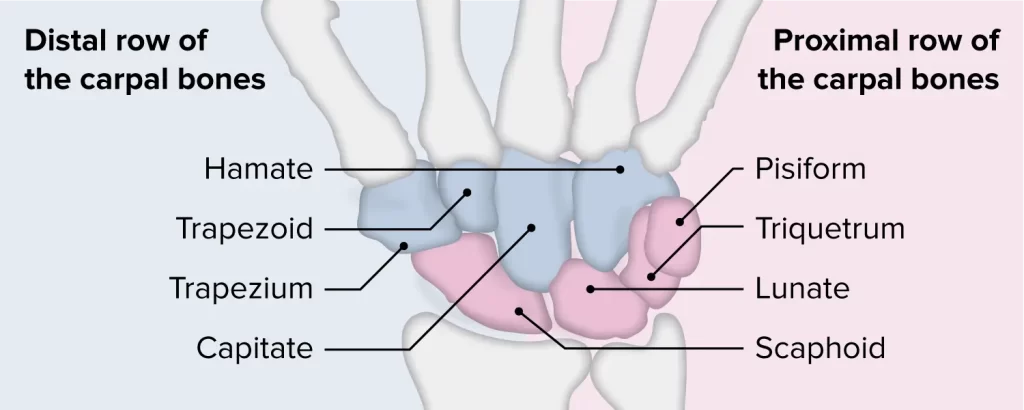
The carpal bones are a group of eight small bones placed in the wrist area. These bones are st in two rows, with four bones in every row. They are responsible for providing stability, flexibility, and support to the wrist joint.
Let’s discuss each carpal bone in detail:
Proximal Row:
- Scaphoid (Navicular) Bone: This bone is located on the thumb side of the wrist. It has a boat-like shape and is the largest bone in the proximal row. It is attached to the radius bone.
- Lunate Bone: Positioned next to the scaphoid bone, the lunate bone has a crescent shape. It connects the scaphoid bone to the triquetrum bone.
- Triquetrum (Triangular) Bone: This bone is triangular in shape and is located on the little finger side of the wrist. It articulates with the lunate bone and the pisiform bone.
- Pisiform Bone: The smallest bone in the carpal bones, it is pea-shaped and located near the triquetrum bone. It serves as a pulley for tendons.
Distal Row:
- Trapezium (Greater Multangular) Bone: Located on the thumb side of the wrist, it has a four-sided shape. It articulates with the scaphoid bone and metacarpal bone of the thumb.
- Trapezoid (Lesser Multangular) Bone: Positioned next to the trapezium bone, it is smaller and wedge-shaped. It connects the trapezium bone to the second metacarpal bone.
- Capitate (Os Magnum) Bone: The largest bone in the distal row, it is located in the center of the wrist. It articulates with the third metacarpal bone and provides stability to the wrist joint.
- Hamate (Unciform) Bone: Located on the little finger side of the wrist, it has a hook-like projection called the hamulus. It connects with the fourth and fifth metacarpal bones.
Functions of the carpal bone
The carpal bones play several important functions in the wrist joint. Here are some key functions of these bones:
- Stability: The arrangement of the carpal bones in two rows provides stability to the wrist joint. They form a strong and stable foundation, allowing for movements while maintaining the integrity of the joint.
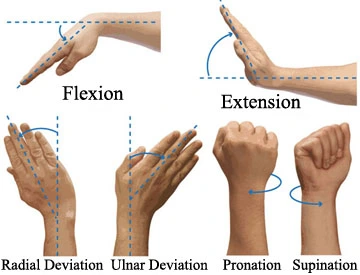
- Flexibility: The carpal bones allow for a wide range of movements in the wrist joint, including flexion, extension, abduction, adduction, and circumduction. These movements are essential for performing various activities such as writing, typing, gripping objects, and playing sports.
- Support: The carpal bones support the weight and load transmitted from the forearm to the hand. They distribute the forces evenly across the wrist joint, preventing excessive stress on any particular bone or joint.
- Attachment Sites: The carpal bones provide attachment sites for various muscles and tendons. These attachments allow for the movement of the hand and fingers. For example, the flexor tendons of the fingers pass through the carpal tunnel, formed by the carpal bones and a ligament, enabling finger flexion.
- Protection: The carpal bones protect the delicate structures within the wrist joint, such as nerves and blood vessels. They form a bony enclosure that shields these structures from external trauma or compression.
- Load Transmission: The carpal bones transmit forces from the hand to the forearm and vice versa. This load transmission is crucial for activities that involve gripping or pushing objects, as it allows for efficient force transfer and prevents excessive strain on the surrounding structures.
Overall, the carpal bones play a vital role in maintaining the stability, flexibility, and support of the wrist joint. Their proper functioning is essential for normal hand and wrist movements and for performing various daily activities.
Conditions that affect carpal bone
There are several conditions that can affect the carpal bones, leading to pain, dysfunction, and limited mobility in the wrist joint. Here are some common conditions:
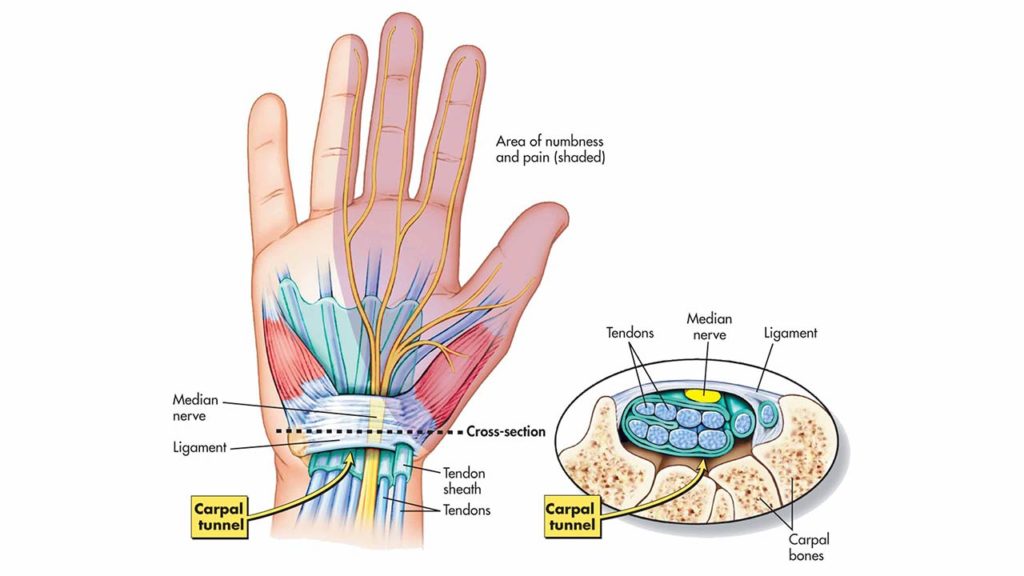
- Carpal Tunnel Syndrome: This is a condition characterized by compression of the median nerve as it passes through the carpal tunnel, a narrow pathway created by the carpal bones and a ligament. It often occurs due to repetitive hand and wrist movements, such as typing or using tools. Symptoms include pain, numbness, tingling, and weakness in the hand and fingers.
- Fractures: Fractures of the carpal bones can occur due to trauma, such as a fall or direct impact on the wrist. Fractures can various types from minor hairline cracks to complete breaks. Symptoms involve bruising, pain, swelling, and difficulty moving the wrist.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that can impact the carpal bones. It occurs when the protective cartilage that cushions the joints wears down over time, leading to pain, stiffness, and limited mobility in the wrist joint.
- Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune disease that causes inflammation and damage to the joints, including the carpal bones. It can lead to pain, swelling, stiffness, and deformity in the wrist joint.
- Kienbock’s Disease: This is a condition where one of the carpal bones, called the lunate bone, loses its blood supply and begins to deteriorate. It can occur due to trauma or unknown reasons. Symptoms include pain, swelling, limited wrist motion, and weakness in the hand.
- Ganglion Cysts: Ganglion cysts are fluid-filled sacs that develop near joints or tendons, often on the back of the wrist. They can arise from the carpal joints and cause pain, swelling, and limited mobility.
Treatment for these conditions may include rest, immobilization, physical therapy, pain medication, and in severe cases, surgery. It is important to seek medical attention if you experience persistent wrist pain or have difficulty using your hand and wrist.
Metacarpal bones
The metacarpal bones are a group of five long bones located in the palm of the hand, between the wrist and the fingers. They connect the wrist bones (carpal bones) to the bones of the fingers (phalanges). The metacarpal bones play a crucial role in hand function, providing support, stability, and mobility. They allow for precise movements and grip strength, enabling activities such as writing, grasping objects, and performing fine motor tasks.
Parts of metacarpal bones
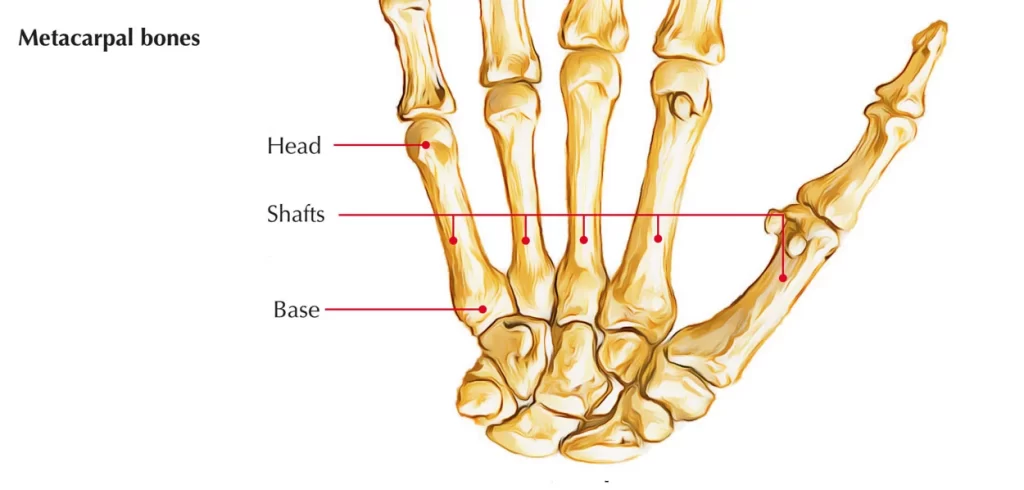
Each metacarpal bone consists of several important parts:
- Base: The base is the proximal end of the metacarpal bone, closest to the wrist. It is wider and thicker than the shaft of the bone and articulates with the carpal bones. The base provides stability and support for the hand.
- Shaft: The shaft is the middle portion of the metacarpal bone. It is long, cylindrical, and slightly curved. The shaft provides attachment sites for muscles, ligaments, and tendons, contributing to hand movement and function.
- Head: The head is the distal end of the metacarpal bone, closest to the fingers. It is rounded and smooth, and it articulates with the proximal phalanx (the first bone of each finger). The head allows for smooth movement and flexibility of the fingers.
- Neck: The neck is a narrowed region between the head and the shaft of the metacarpal bone. It is a common site for fractures due to its relatively weak structure compared to other parts of the bone.
- Articular Surface: The articular surface is the area of the base and head that connects with other bones. It is covered with cartilage, which helps facilitate smooth movement at the joints.
Functions of the metacarpal bones
The metacarpal bones are a group of five long bones present in the hand, in between the carpal bones of the wrist and the phalanges of the fingers. They play several important functions in the hand:
- Support and Structure: The metacarpal bones provide a framework and support for the palm of the hand. They form the base of the hand and help maintain its shape and structure.
- Movement and Flexibility: The metacarpal bones serve as attachment points for muscles and tendons that control movement in the hand. They allow for flexion, extension, abduction, adduction, and rotation of the fingers and thumb, enabling a wide range of movements and fine motor skills.
- Grip and Grasping: The metacarpal bones contribute to the strength and stability of the hand, allowing for a strong grip and effective grasping of objects. They provide a solid foundation for the muscles and tendons involved in gripping activities.
- Transmission of Forces: The metacarpal bones transmit forces from the wrist to the fingers during activities such as pushing, pulling, lifting, and carrying. They distribute these forces evenly across the hand, reducing the risk of injury and strain.
- Sensation and Feedback: The metacarpal bones contain numerous sensory nerves that provide feedback to the brain about touch, pressure, temperature, and pain sensations in the hand. This information helps with dexterity, coordination, and proprioception (awareness of body position).
- Protection: The metacarpal bones protect the underlying soft tissues, such as blood vessels, nerves, and tendons. They act as a shield against external forces or trauma, reducing the risk of injury to vital structures in the hand.
The metacarpal bones play a crucial role in hand function, enabling a wide range of movements, providing support and structure, transmitting forces, and protecting delicate structures. Their health and proper blood supply are essential for maintaining hand function and preventing conditions that can affect hand mobility and dexterity.
Conditions that affect metacarpal bones
There are several conditions that can affect the metacarpal bones, each with its own specific causes, symptoms, and treatment options. Some common conditions include:
- Fractures: Fractures of the metacarpal bones are a common injury, often caused by direct trauma or excessive force to the hand. Symptoms may include pain, swelling, bruising, deformity, and difficulty moving the hand or fingers. Treatment typically involves immobilization with a splint or cast, pain management, and rehabilitation exercises.
- Dislocations: Metacarpophalangeal (MCP) joint dislocations occur when the metacarpal bone is displaced from its normal position at the base of the finger. This can result from a sudden impact or forceful movement. Symptoms involve deformity, pain, swelling, and limited range of motion. Treatment involves reducing the dislocation (putting the bone back in place), immobilization, and sometimes surgery.
- Arthritis: Arthritis can affect the metacarpophalangeal (MCP) joints and cause inflammation, pain, stiffness, and limited mobility. Osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis are common types of arthritis that can affect the metacarpal bones. Treatment may include medication, physical therapy, splinting, injections, and in severe cases, surgery.
- Infections: Infections can occur in the metacarpal bones, usually as a result of an open fracture or penetrating injury. Symptoms may include pain, redness, swelling, warmth, fever, and pus drainage. Treatment typically involves antibiotics, wound care, and sometimes surgical drainage or debridement.
- Tumors: Tumors can develop in the metacarpal bones, although they are relatively rare. These can be anyone, benign (non-cancerous) or malignant (cancerous). Symptoms may include pain, swelling, a lump or mass, and changes in the appearance or function of the hand. Treatment depends on the type and stage of the tumor and may involve surgery, radiation therapy, chemotherapy, or a combination of treatments.
It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment if you suspect any issues with your metacarpal bones. Early intervention and proper management can help prevent complications and promote optimal hand function and mobility.
Blood supply to carpal and metacarpal bones
The blood supply to the carpal and metacarpal bones is provided by a network of arteries and veins. This blood supply is crucial for the health and function of these bones.
The main arteries that supply blood to the metacarpal bones are the radial artery and the ulnar artery. These arteries originate from the brachial artery in the upper arm and travel down the forearm. As they reach the wrist, they divide into smaller branches that supply blood to the hand and fingers.
The radial artery gives off several branches that supply blood to the carpal bones. These branches include the dorsal carpal branch, which runs along the back of the wrist, and the palmar carpal branch, which travels along the palm side of the wrist. These branches provide blood to the carpal bones, including the scaphoid, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, and hamate bones.
The ulnar artery also gives off branches that supply blood to the carpal bones. These branches include the deep palmar branch and the superficial palmar branch. The deep palmar branch supplies blood to the carpal bones on the palm side of the hand.
In addition to these main arteries, there are smaller arteries called perforating branches that provide additional blood supply to the carpal bones. These perforating branches arise from nearby arteries, such as the radial or ulnar arteries, and penetrate through the surrounding tissues to reach the carpal bones.
Veins accompany the arteries and help drain deoxygenated blood from the metacarpal and carpal bones. The veins follow a similar course as the arteries and eventually join larger veins in the forearm.
The blood supply to the metacarpal and carpal bones is important for maintaining their health and function. Adequate blood flow ensures that these bones receive oxygen and nutrients necessary for their growth, repair, and overall well-being. Insufficient blood supply can lead to conditions such as avascular necrosis, where the bone tissue dies due to lack of blood flow.
Phalanges
The phalanges are connected by joints, including the MCP, PIP, and DIP joints, which allow for various movements of the fingers and thumb. These joints are supported by ligaments, tendons, and muscles, which provide stability and control the range of motion.
Parts of the phalanges
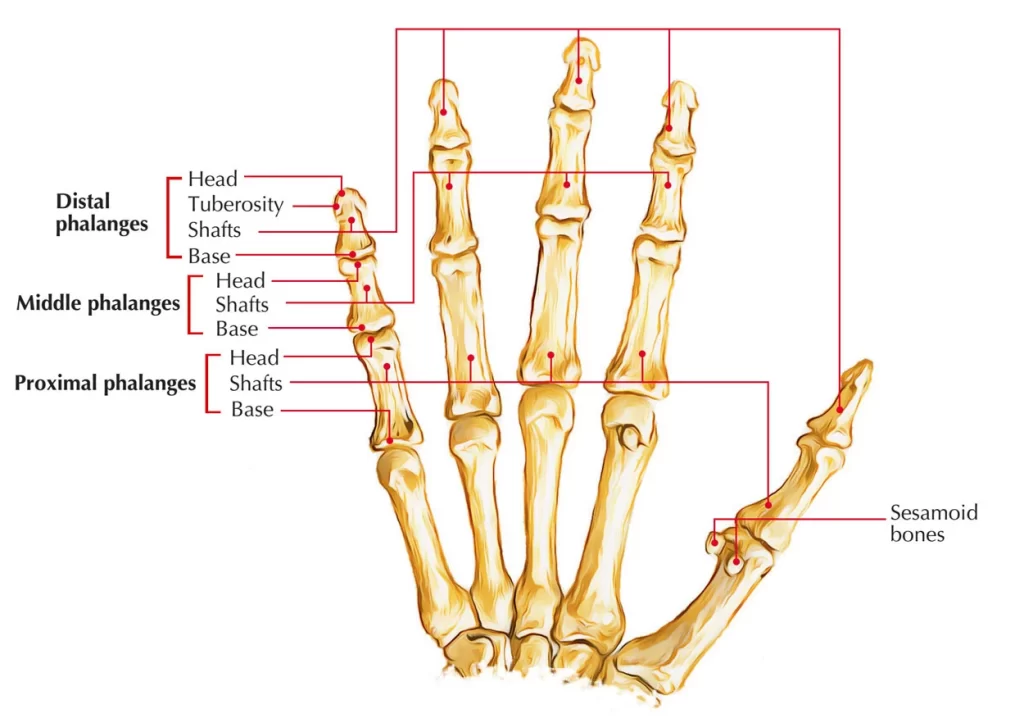
The phalanges are the bones that create the fingers and the thumb. Each finger has three phalanges, while the thumb has two phalanges. The phalanges are categorized into three types: proximal, middle, and distal.
- Proximal Phalanx: The proximal phalanx is the bone closest to the metacarpal bone. It is larger and longer than the other two phalanges in each finger. The proximal phalanx connects to the metacarpal bone at the metacarpophalangeal (MCP) joint. It has a rounded head that articulates with the corresponding metacarpal bone and a base that connects to the middle phalanx. The proximal phalanx provides stability and allows for flexion and extension movements at the MCP joint.
- Middle Phalanx: The middle phalanx is located between the proximal and distal phalanges. It is shorter than the proximal phalanx but longer than the distal phalanx. The middle phalanx also has a head that articulates with the base of the proximal phalanx, and a base that connects to the distal phalanx. Like the proximal phalanx, it allows for flexion and extension movements at the proximal interphalangeal (PIP) joint.
- Distal Phalanx: The distal phalanx is the bone at the tip of each finger. It is the smallest and most distal of the three phalanges. The distal phalanx has a head that articulates with the base of the middle phalanx, and it also contains the nail bed and nail. The distal interphalangeal (DIP) joint allows for flexion and extension movements of the distal phalanx.
Functions of the phalanges
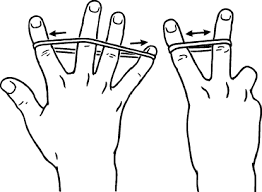
- Movement: The primary function of the phalanges is to facilitate movement in the fingers and toes. They provide a framework and support for the muscles, tendons, and ligaments that control these movements. The phalanges allow for flexion (bending) and extension (straightening) of the fingers and toes, as well as abduction (spreading apart) and adduction (bringing together) of the digits.
- Grasping and Manipulation: The phalanges play a crucial role in our ability to grasp and manipulate objects. The distal phalanges, located at the tips of the fingers and toes, have specialized structures called nail plates that protect the sensitive fingertip and enhance tactile sensitivity. These structures, along with the joints between the phalanges, allow for precise movements and fine motor control necessary for activities such as writing, typing, playing musical instruments, and picking up small objects.
- Support and Stability: The phalanges provide support and stability to the hand and foot. They form the foundation for the muscles, tendons, and ligaments that connect the hand and foot to the rest of the body. The alignment and proper functioning of the phalanges are crucial for maintaining balance, stability, and coordination during activities such as walking, running, and gripping objects.
- Protection: The phalanges help protect the delicate structures within the fingers and toes. They serve as a shield for the nerves, blood vessels, and soft tissues that run through these regions. Additionally, the phalanges contribute to the overall structural integrity of the hand and foot, providing a protective framework against external forces and potential injuries.
- Sensation: The phalanges contain numerous sensory receptors that contribute to our sense of touch and proprioception (awareness of the position and movement of our body parts). These receptors, located in the skin, joints, and connective tissues surrounding the phalanges, provide valuable feedback to the brain, allowing us to perceive and respond to different tactile stimuli.
The phalanges play a vital role in hand and foot function. They enable movement, support and stabilize the hand and foot, protect underlying structures, and contribute to our sense of touch and proprioception. Without the phalanges, our ability to perform intricate tasks, maintain balance, and interact with our environment would be significantly impaired.
Conditions that affect phalanges
There are several conditions that can affect the phalanges, leading to impaired blood supply and potential complications. Here are a few examples:
- Peripheral artery disease (PAD): PAD is a condition characterized by the narrowing or blockage of arteries that supply blood to the extremities, including the fingers and toes. The reduced blood flow can result in pain, numbness, and poor wound healing in the affected phalanges.
- Raynaud’s disease: Raynaud’s disease is a condition that causes episodes of reduced blood flow to the fingers and toes, typically triggered by cold temperatures or emotional stress. During an episode, the blood vessels in the phalanges constrict, leading to color changes (white, blue, and then red) and discomfort.
- Vasculitis: Vasculitis refers to inflammation of the blood vessels, which can affect the arteries and veins supplying the phalanges. This inflammation can lead to narrowing or blockage of the vessels, impairing blood flow and causing symptoms such as pain, swelling, and skin changes.
- Atherosclerosis: Atherosclerosis is a medical condition characterized by the buildup of plaque within the arteries. This plaque can narrow the blood vessels supplying the phalanges, reducing blood flow and potentially causing complications such as pain, ulceration, and tissue death.
- Thromboangiitis obliterans (Buerger’s disease): Buerger’s disease is a rare condition that primarily affects the small and medium-sized arteries and veins in the extremities. It is characterized by inflammation and clot formation within these vessels, leading to reduced blood flow. Symptoms may include pain, ulcers, and gangrene in the fingers and toes.
- Trauma or fractures: Injuries to the fingers or toes, such as fractures or crush injuries, can damage the blood vessels supplying the phalanges. This can result in compromised blood flow and potential complications such as tissue ischemia and necrosis.
It is important to note that these conditions can have various causes and risk factors, including smoking, diabetes, high blood pressure, autoimmune disorders, and certain medications. Proper diagnosis and management by a healthcare professional are essential for treating these conditions and preserving the health of the phalanges.
Blood supply
The phalanges, which are the bones in the fingers and toes, receive their blood supply through a network of arteries and veins. The blood supply to the phalanges is essential for their proper functioning and overall health.
The arterial blood supply to the phalanges originates from several sources. The main arteries that supply the fingers and toes are the digital arteries, which arise from the palmar and plantar arches in the hand and foot, respectively. These arteries branch out into smaller vessels known as arterioles, which then supply every phalanges.
Within each phalanx, the arteries form a network of smaller blood vessels known as capillaries. Capillaries are tiny, thin-walled vessels that allow for the exchange of oxygen and nutrients with the surrounding tissues. They also remove waste products generated by cellular metabolism.
The venous drainage of the phalanges occurs through a network of veins that run parallel to the arteries. These veins collect deoxygenated blood and waste products from the capillaries and carry them back toward the heart. The veins in the fingers and toes eventually merge into larger vessels, such as the digital veins, which then drain into deeper veins in the hand or foot.
The blood supply to the phalanges is crucial for maintaining their normal function and health. Adequate blood flow ensures the delivery of oxygen and nutrients to the bone, muscles, tendons, ligaments, and other structures within the phalanges. It also helps remove waste products and toxins from these tissues.
Impaired blood supply to the phalanges can lead to various complications. Reduced blood flow, such as in cases of arterial occlusion or narrowing, can result in tissue ischemia (lack of oxygen) and necrosis (tissue death). This can cause pain, deformity, and functional limitations in the affected phalanx.
In some cases, conditions that affect the blood vessels, such as vasculitis or atherosclerosis, can disrupt the blood supply to the phalanges. Additionally, trauma or fractures can damage the blood vessels, leading to compromised blood flow.
Overall, maintaining a healthy blood supply to the phalanges is crucial for their optimal function and overall well-being. If you experience any symptoms related to impaired blood flow, such as persistent pain, discoloration, or numbness in your fingers or toes, it is important to seek medical attention for proper evaluation and treatment.
Physiotherapy treatment
Physiotherapy treatment for upper limb conditions involves a range of interventions aimed at improving mobility, and function, and reducing pain. The specific treatment approach will depend on the underlying condition and individual needs of the patient. Here are some common physiotherapy techniques used in the treatment of upper limb conditions:
- Manual therapy: This involves hands-on techniques performed by the physiotherapist to mobilize joints, stretch muscles, and soft tissues, and improve joint alignment. Manual therapy can help reduce pain, increase range of motion, and improve function.
- Therapeutic exercises: Physiotherapists prescribe specific exercises to strengthen muscles, improve flexibility, and restore normal movement patterns. These exercises may include stretching, resistance training, and functional activities tailored to the individual’s condition and goals.
- Range of motion exercises: These exercises purpose to increase joint mobility and flexibility. They may involve passive movements performed by the therapist or active movements performed by the patient.
- Neuromuscular re-education: This technique focuses on improving coordination, proprioception (awareness of joint position), and motor control. It involves exercises and activities that challenge balance, coordination, and control of movement.
- Modalities: Physiotherapists may use various modalities to help manage pain and promote tissue healing. These may include heat or cold therapy, ultrasound, electrical stimulation, and laser therapy.
- Functional training: This involves practicing specific tasks or activities that are important for the individual’s daily life or work. The physiotherapist will assess the patient’s functional goals and design a program to improve performance and independence in these activities.
- Education and advice: Physiotherapists provide education on proper body mechanics, ergonomics, and strategies to prevent further injury or exacerbation of symptoms. They may also provide guidance on activity modification and self-management techniques.
- Assistive devices and orthotics: In some cases, the use of assistive devices or orthotic devices may be recommended to support and protect the upper limb during activities or to improve function.
It is important to note that physiotherapy treatment for upper limb conditions is individualized and may vary depending on the specific condition and patient’s needs. A thorough assessment by a qualified physiotherapist is essential to develop an appropriate treatment plan and monitor progress.
Exercise for upper limb
Exercise for the upper limb can help improve strength, flexibility, and function. Here are some common exercises that may be prescribed by a physiotherapist:

Shoulder exercises:
Shoulder flexion: Stand or sit upright and raise your arm forward and upward, reaching as high as possible. do this movement again for a set number of repetitions.
Shoulder abduction: Stand or sit upright and raise your arm out to the side, away from your body. do this movement again for a set number of repetitions.
Shoulder external rotation: Hold a resistance band or a lightweight in your hand and keep your elbow bent at 90 degrees. Do the rotation of your arm outward, away from your body. Do this movement again for a set number of repetitions.

Elbow exercises:
Bicep curls: Hold a dumbbell or resistance band in your hand, with your palm facing up. Bend your elbow and bring the weight towards your shoulder, then slowly lower it back down. do this movement again for a set number of repetitions.
Tricep extensions: Hold a dumbbell or resistance band in your hand, with your palm facing down. Straighten your elbow and extend your arm backward, then slowly bend it back to the starting position. Do this movement again for a set number of repetitions.
Wrist and hand exercises:
Wrist flexion and extension: Hold a lightweight or resistance band in your hand, with your palm facing down. Bend your wrist upward, then slowly lower it back down. do this movement again for a set number of repetitions.
Finger and thumb exercises: Squeeze a softball or use putty to strengthen the muscles in your fingers and thumb. Open and close your hand, spread your fingers apart, and touch each finger to your thumb.
Grip strengthening exercises:
Hand grip squeezes: take a softball or grip strengthener in your hand and squeeze it as hard as you can. Maintain the squeeze for a few seconds, then release it. do this movement again for a set number of repetitions.
Finger extensions: Place a rubber band around your fingers and spread them apart against the resistance of the band. Do this movement again for a set number of repetitions.
It is important to perform these exercises under the guidance of a physiotherapist to ensure proper technique and to avoid further injury. The number of repetitions and sets will depend on your individual needs and abilities. Gradually raising the intensity and challenges of the exercises as you progress.
FAQ
The bones that make up the upper limb include the humerus, radius, ulna, carpals, metacarpals, and phalanges.
Each finger has 3 phalanges, while the thumb has 2.
The humerus is the main bone in the upper arm.
The five long bones in the palm of the hand are called metacarpals.
The upper limb bones allow for movements such as flexion, extension, abduction, adduction, rotation, and gripping.
The upper limb bones provide strength, flexibility, and support to the upper limb, allowing for movement and manipulation of objects.