Supinator Syndrome (Radial Tunnel Syndrome)
Table of Contents
What is a Supinator Syndrome?
Supinator syndrome, also known as posterior interosseous nerve syndrome, is a condition characterized by compression or irritation of the posterior interosseous nerve as it passes through the supinator muscle of the forearm. The supinator muscle is responsible for turning the forearm from pronation (palm down) to supination (palm up).
When the radial nerve is pinched or irritated in the supinator muscle, it can cause symptoms such as pain, weakness, and difficulty moving the wrist and fingers. Activities that involve repetitive pronation and supination of the forearm and trauma can contribute to supinator syndrome.
Diagnosis is usually based on a thorough medical history, physical examination, and possible additional tests such as electromyography (EMG) or nerve conduction studies. Treatment options may include rest, activity modification, physical therapy, immobilization, medications, injections, or surgical procedures, depending on the severity and response to conservative measures. Generally, supinator syndrome refers to compression or irritation of the posterior interosseous nerve of the supinator muscle, resulting in forearm and hand symptoms.
Clinically relevant anatomy
Supinator syndrome is clinically relevant to the anatomy of the forearm. To understand the syndrome, it is important to know the corresponding anatomical structures. The following are the clinically important anatomical structures associated with supinator syndrome:
Radial nerve:
- The radial nerve is a large nerve that runs along the back of the hand and forearm.
- It is responsible for the innervation and sensory nutrition of various muscles in the upper arm, forearm, and back of the hand.
- The posterior interosseous nerve is a radial nerve branch that contributes to supinator syndrome.
Supinator muscle:
- The supinator muscle is located at the back of the forearm.
- It originates from the lateral epicondyle of the humerus and the proximal ulna and inserts on the proximal radius.
- The supinator muscle plays a vital role in forearm rotation, allowing the forearm to move from a prone position (palm down) to a supine position (palm up).
Posterior Interosseous Nerve:
- The posterior interosseous nerve is a radial nerve branch.
- It arises below the elbow and passes through the supinator muscle in a tunnel space called the arcade of Frohsen.
- The posterior intrinsic nerve provides motor nerve supply to several muscles of the forearm that control the extension of the finger and thumb.
- It does not provide a sensory nerve.
- In supinator syndrome, compression or irritation of the posterior interosseous nerve occurs as it passes through the supinator muscle.
- This can be caused by a number of reasons, including repetitive pronation and supination of the forearm, trauma, or anatomical variations.
- Understanding the anatomical relationship between the radial nerve, the supinator muscle, and the posterior interosseous nerve is critical to the effective diagnosis and treatment of supinator syndrome.
- Health professionals can provide appropriate treatment and relieve associated symptoms if they recognize compression or irritation of the posterior interosseous nerve of the supinator muscle.
Epidemiology
The epidemiology of supinator syndrome, also known as posterior interosseous nerve syndrome, has not been fully documented. However, information about its prevalence and occurrence can be inferred from available studies and clinical observations. It is important to note that the exact prevalence and incidence of supinator syndrome may vary by population and diagnostic criteria. Here are some important points about the epidemiology of supinator syndrome:
Incidence:
- The exact incidence of supinator syndrome has not been established.
- It is considered a relatively rare condition compared to other nerve entrapment syndromes such as carpal tunnel syndrome.
- The overall incidence is unknown and epidemiological data are limited.
Age and gender:
- Supinator syndrome can occur in different age groups.
- This has been reported in both younger and older populations.
- There does not appear to be a significant gender bias and cases have been reported in both males and females.
Occupation and Activities:
- Supinator syndrome is often associated with occupational or recreational activities that involve repetitive pronation and supination of the forearm.
- This includes occupations such as mechanics, carpenters, assembly line workers, and athletes who participate in sports such as tennis or baseball.
- These activities can increase stress on the supinator muscle and intercostal nerve.
Bilateral involvement:
Supinator syndrome can be unilateral (affects one arm) or bilateral (affects both arms). Bilateral involvement is less common but may occur in some cases.
Associated Conditions:
- Supinator syndrome can sometimes be associated with other conditions that can contribute to nerve compression or irritation.
- These include trauma, fractures, anatomical variations, and diseases such as rheumatoid arthritis.
Because epidemiological data on supinator syndrome are limited, it is difficult to provide accurate data on its prevalence or specific risk factors. It is generally considered a relatively rare disease, but further research is needed to better understand its true prevalence and associated factors.
Causes of Supinator Syndrome
The etiology or causes of supinator syndrome, also known as posterior interosseous nerve syndrome, can vary. The condition is usually caused by compression or irritation of the intercostal nerve as it passes through the supinator muscle of the forearm. Here are some common etiologic factors associated with supinator syndrome:
Overuse or repetitive motion:
- Activities that involve repetitive forearm pronation and supination can contribute to supinator syndrome.
- People who perform repetitive tasks or sports activities that require frequent and forceful rotation of the forearm, such as using power tools, playing tennis, or throwing a baseball, may be at greater risk.
Trauma or injury:
A direct blow or trauma to the forearm can cause supinator syndrome. Fractures or dislocations around the elbow or forearm bones can cause swelling, inflammation, or anatomical changes that compress the intercostal nerve.
Anatomical Variations:
- Certain anatomical variations or anomalies of the forearm may predispose to the development of supinator syndrome.
- For example, a tight or narrowed Arcadi de Frohsen (the tunnel space through which a nerve passes) can increase the risk of nerve compression.
Rheumatoid arthritis:
- In some cases, supinator syndrome can be associated with rheumatoid arthritis, an autoimmune disease characterized by inflammation of the joints.
- Inflammation of the forearm joints can cause swelling and compression of the interosseous nerve.
Ganglion cysts:
- Ganglion cysts are noncancerous sacs that can form near joints, including the wrist and elbow.
- If a ganglion cyst forms near the intercostal nerve or the supinator muscle, it can put pressure on the nerve, causing symptoms of supinator syndrome.
Other Factors:
- Other factors that may contribute to the development of supinator syndrome include anatomical abnormalities, tumors, infections, or iatrogenic causes (due to medical procedures or interventions).
- It is important to note that although these factors are often associated with supinator syndrome, the exact etiology can vary from person to person.
- Correct diagnosis and assessment by a health professional are crucial to determine the specific cause and direct appropriate treatment in each specific case.
Symptoms of Supinator Syndrome
The clinical presentation of supinator syndrome, also known as posterior interosseous nerve syndrome, can vary from person to person. Symptoms are usually caused by compression or irritation of the posterior nerve as it passes through the supinator muscle of the forearm. Here are the common clinical signs associated with supinator syndrome:
Pain:
- Forearm pain is a common symptom of supinator syndrome.
- The pain is usually located on the back of the forearm, although it can also radiate to the back of the hand and fingers.
- The pain may worsen with activities that involve turning or grasping the forearm.
Weakness:
- Weakness of the muscles that control finger and thumb extension.
- This weakness can cause difficulty in performing activities that require a strong grip or manipulation, such as holding objects or fully extending the fingers.
Difficulty with wrist and finger movements:
- People with supinator syndrome may have limited or difficult wrist and finger movements.
- Full extension of the wrist, fingers, or thumb may be difficult, resulting in a reduced range of motion.
Tendency:
- The tendency can occur along the course of the nerve between the dorsal bones of the forearm. Palpation around the supinator muscle or Frohsen’s arch may cause tenderness.
Sensory changes:
- Unlike some other nerve compression syndromes, supinator syndrome usually does not cause sensory disturbances or numbness.
- The posterior interosseous nerve provides mainly a motor nerve and does not have a significant sensory component.
- It is necessary to note that the severity of symptoms may differ.
- Some people may experience mild discomfort and functional limitations, while others may experience more severe pain and weakness.
- Symptoms may worsen with activities that involve repetitive twisting or gripping of the forearm.
- If you suspect supinator syndrome or symptoms in your forearm or hand, it is recommended that you see a doctor for an accurate diagnosis and appropriate treatment.
- They can perform a thorough evaluation, including a physical exam and, if possible, additional tests to confirm the diagnosis and guide the most appropriate treatment plan.
Differential diagnosis
When evaluating a patient with symptoms suggestive of supinator syndrome, healthcare professionals should consider other conditions that may cause similar symptoms. Differential diagnosis involves differentiating supinator syndrome from other conditions that may present with forearm or hand pain, weakness, and limited range of motion. Some common conditions that may include the differential diagnosis of supinator syndrome include:
Radial tunnel syndrome:
- Radial tunnel syndrome is a condition characterized by compression or irritation of the radial nerve in the forearm.
- This can cause symptoms similar to supinator syndrome, including forearm pain, weakness, and difficulty with wrist and finger movements.
- However, in radial tunnel syndrome, the pain is usually more localized to the lateral aspect of the forearm and may be aggravated by activities that involve forearm extension or resistance to supination.
Cubital Tunnel Syndrome:
- Cubital Tunnel Syndrome is a condition caused by compression or irritation of the ulnar nerve at the elbow.
- Although it mainly affects the ulnar nerve, it can also affect the interosseous nerve and cause symptoms similar to supinator syndrome.
- Patients may experience forearm pain, weakness, and difficulty moving the wrist and fingers, especially when extending the fingers.
Cervical radiculopathy:
- Cervical radiculopathy refers to nerve root compression or irritation in the cervical spine (neck).
- This can cause symptoms that radiate down the arm, including forearm pain, weakness, and altered sensation.
- Differentiating cervical radiculopathy from supinator syndrome may require a detailed clinical examination and possible imaging studies such as an MRI of the cervical spine.
Tennis elbow (lateral epicondylitis):
- Tennis elbow is a condition characterized by inflammation or degeneration of tendons on the lateral (outer) side of the elbow.
- This can cause pain and weakness in the forearm, such as supinator syndrome.
- However, tennis elbow pain is usually localized to the lateral aspect of the elbow and can be aggravated by holding or extending the wrist.
De Quervain Tenosynovitis:
- De Quervain Tenosynovitis is a condition distinguishes by inflammation of the tendons on the radial side of the wrist.
- This can indicate pain, weakness, and limited movement of the thumb and wrist.
- Although it mainly affects the wrist and thumb, it can cause symptoms that can be confused with supinator syndrome when the interosseous nerve is involved.
Other conditions that may be considered in the differential diagnosis include forearm muscles, arthritis, fractures, and other nerve entrapment syndromes. Proper evaluation by a healthcare professional, including a detailed medical history, physical examination, and possible imaging or electrodiagnostic studies, can help differentiate supinator syndrome from other conditions and guide appropriate treatment.
Other pathologies associated with pain in the lateral elbow joint are:
- Pigmented villous nodular synovitis
- Lateral epicondylitis
- Radial nerve damage/paralysis
- Cervical radiculopathy
- Extensor Carpi radialis brevis tendinosis
- Cervical spine C5-C7
- Extensor tendon tear
- Triangular finger
- Rupture of the sagittal ligament
- Inflammatory involvement of the metacarpophalangeal joints
- Tendinitis of the anconeus muscle
- Supinator syndrome
- Brachial neuritis
- Arthritis/arthritis of the radiohumeral joint
- The meniscus of the radiohumeral joint
- Olecranon bursitis
- Neuralgic amyotrophy
- Interpalm tear
- Wartenberg disease (sensory only)
Diagnosis of Supinator Syndrome
A diagnosis of supinator syndrome, also known as posterior interosseous nerve syndrome, involves a thorough evaluation that includes a medical history, physical examination, and possibly other diagnostic tests. Here are the main considerations when diagnosing supinator syndrome:
Physical Examination:
- The healthcare professional begins by gathering information about the patient’s symptoms, including the location, onset, and duration of forearm and hand pain, weakness, or limited movement.
- They will ask about any activities or occupations that involve repetitive rotation or impact of the forearm, and about any trauma or previous injuries to the elbow or forearm.
- A full physical examination is performed to evaluate the affected hand, arm, and hand.
- The doctor will palpate around the supinator muscle and the course of the posterior interosseous nerve to check for tenderness or swelling.
- They assess muscle strength, range of motion, and sensory changes. Special attention is given to the supination and pronation of the forearm.
- History
- Functional limitations or deficiencies
Palpate:
Expect abnormal tenderness over Frohsen’s arch and possibly the lateral epicondyle
Nervous system stress test
- Nerve stress tests, also known as neurodynamic tests or nerve stress tests, are commonly used to assess nerve mobility and sensitivity.
- Although there is no specific nerve stress test for supinator syndrome alone, certain nerve stress tests can help evaluate posterior interosseous nerve (PIN) involvement when supinator syndrome is suspected.
- Here is an example of a stress test that can be performed to evaluate a PIN.
Radial nerve tension test (neurodynamic test of upper extremity 2A):
- Starting position: The patient sits comfortably with his legs extended.
- PROCEDURE:
- The examiner stands behind the patient and grasps the patient’s wrist with one hand, keeping the elbow extended.
- The other hand supports the shoulder to prevent compensatory movements.
- The examiner slowly moves the patient’s shoulder into abduction (away from the body) and external rotation (turning the arm outward).
- While maintaining the shoulder position, the examiner passively flexes the patient’s wrist and fingers.
Test Interpretation:
- A test is considered positive for PIN if it reproduces the patient’s symptoms, such as pain, weakness or abnormal sensations in the forearm and back of the hand.
- It is important to note that nerve stress tests must be performed by trained health professionals who know the proper techniques and interpretations.
- These tests should be used as part of a comprehensive evaluation and should be considered in conjunction with other clinical findings and diagnostic tests.
- In addition, the nerve stress test used may vary according to the patient’s appearance and the suspicion of other nerves besides the PIN.
- Therefore, it is very important to consult with a doctor who can determine the most appropriate tests and interpret the results accurately based on a person’s specific condition.
Muscle test (resistance):
- The wrist extensors are partially or completely paralyzed:
- The patient cannot extend the thumb and other fingers of the affected side at the metacarpophalangeal joints.
- Wrist extension is possible, usually in a radially deviated direction, due to the extensor carpi radialis longus and weakened extensor carpi ulnaris
- Supination and pronation of the forearm can cause pain, as can extending the middle finger
- The brachioradialis and extensor carpi radialis longus are innervated by the closer branches of the radial nerve, so they can be spared.
Provocative tests:
- Specific tests can be done to repeat or worsen symptoms.
- For example, the resisted supination test, also known as the “middle finger test,” requires the patient to resist supination while the examiner provides resistance.
- This can help cause pain or weakness associated with supinator syndrome.
Electrodiagnostic studies:
- In some cases, electromyography (EMG) and nerve conduction studies (NCS) may be recommended to assess the function of the posterior interosseous nerve and confirm the diagnosis.
- EMG can help assess the electrical activity of muscles innervated by a nerve, while NCS can assess nerve conduction velocity and identify any abnormalities.
Imaging studies:
- Imaging studies, such as X-rays, ultrasound, or MRI, may be ordered to rule out other possible causes of symptoms or to evaluate anatomical abnormalities, fractures, or soft tissue pathologies that may cause compression or irritation.
- Intercostal nerve It is important to note that the diagnosis of supinator syndrome is often based on a combination of clinical findings, as there is no definitive diagnostic test.
- In making a diagnosis, a healthcare professional considers the patient’s history, medical examination results and rules out other possible conditions.
- Consultation with a physician is recommended for accurate diagnosis and appropriate treatment of supinator syndrome.
- He can assess the individual’s specific symptoms, perform the necessary tests and offer personalized treatment options based on the results.
Outcome measures
- Disability of Arms, Shoulders, and Hands (DASH)
Medical Treatment of Supinator Syndrome
Medical treatment for supinator syndrome, also known as posterior interosseous nerve syndrome, focuses on relieving symptoms, reducing inflammation, and promoting nerve healing. Treatment can vary depending on the severity of the symptoms and the underlying cause of the condition. Here are some common treatment strategies for supinator syndrome:
Rest and activity modification:
- Initially, avoiding activities that worsen symptoms and resting the affected arm can help reduce compression of the intercostal nerve.
- As the nerve heals, it may be necessary to modify work or recreational activities that involve repetitive twisting or grasping of the forearm.
Nonsteroidal inflammatory drugs
- Over-the-counter or prescription medications such as ibuprofen or naproxen may be recommended to reduce pain and inflammation associated with supinator syndrome.
- These medicines should be used according to the instructions and under the guidance of a doctor.
Steroid injections:
- Corticosteroid injections may be considered in cases where conservative measures do not provide adequate relief.
- These injections are designed to reduce inflammation and can help relieve pain and swelling.
- They are usually administered by a healthcare professional experienced in joint or soft tissue injections.
Surgical intervention:
- Surgery is rarely necessary for supinator syndrome but may be considered for persistent symptoms or failure of conservative measures.
- The purpose of the surgical procedure is to relieve compression of the intercostal nerve. The specific surgical approach depends on the cause and extent of nerve damage.
- For an accurate diagnosis and proper treatment of supinator syndrome, it is important to consult a health professional such as a primary care physician, orthopedist, or physiatrist.
- He can assess the severity of the condition, direct the treatment plan and give individual recommendations based on the person’s special needs.
Indication for surgery
- With conservative treatment, improvement does not occur after 3-6 months
- The pain appears after 12 weeks
- Surgical decompression may be indicated to prevent nerve damage. The goal: complete recovery
- Recovery and Results: Depends on the extent of nerve damage and most neuropraxic problems resolve. Patient care after decompression involves a gradual return to activities over 6 weeks. Surgery: Depends on how and where the collision occurs
- Arcade of Frohse edition
- Resection of lesions
- Release of the posterior interosseous nerve
- Superficial radial nerve release
- Supinator extension
- Synovectomy
Physiotherapy Treatment in Supinator Syndrome
Physical therapy plays an essential role in the treatment of supinator syndrome (posterior interosseous nerve syndrome). The goals of physical therapy for supinator syndrome are to reduce pain and inflammation, improve muscle strength and flexibility, restore range of motion, and promote recovery of function. Here are some common physical therapy interventions that can be used:
Therapeutic exercises:
A physical therapist will prescribe specific exercises that target the affected muscles and restore strength and flexibility. These exercises may include:
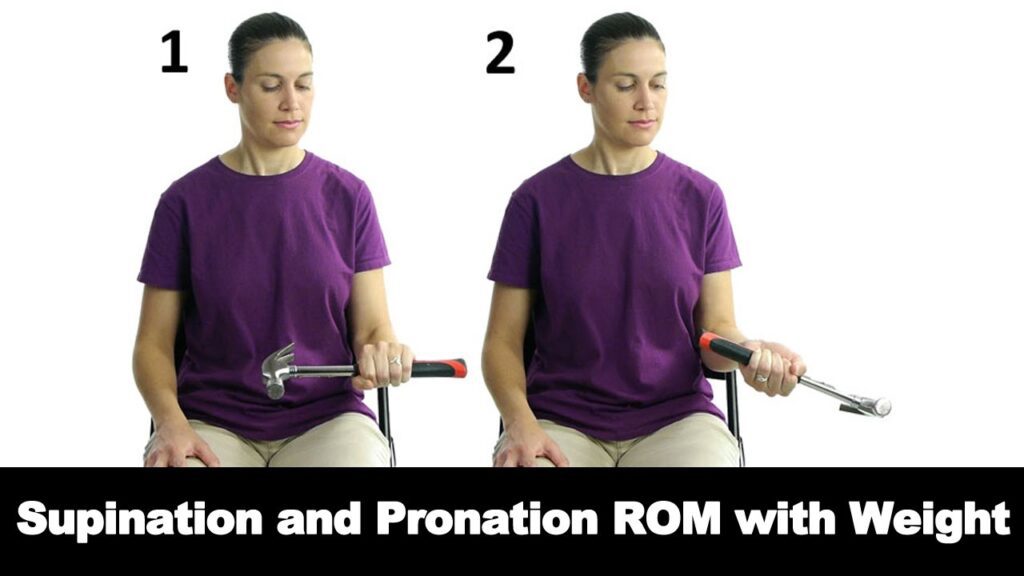
Movements:
- Passive and active movements to improve forearm pronation and supination, wrist flexion and extension, and finger movements.
Eccentric wrist supination

- This exercise can be done free or with resistance to strengthen the forearm muscles.
- Keep your other arm close to your side with your elbow at a 90-degree angle.
- Start with the palm down.
- Carefully rotate the forearm so that the palm is facing up.
- Hold a small stop in your hand to make the movement difficult.
- This can also be done with a resistance band, for this tie a resistance band to your arm and take the other end that goes around your arm.
- Gently rotate your forearm against the resistance of the strap until the palm is facing up.
Strengthening exercises:
- Resistance training strengthens the muscles that control forearm rotation and wrist and finger movements.
- This may require the use of weights, resistance bands, or special equipment.
Supination and pronation of the forearms:

- Pronation supination with resistance band
- Keeping your elbow at your side, bend your elbow to 90 degrees.
- Hold for 10 seconds while raising your palm.
- Then hold for 10 seconds while gently lowering your palm.
- During the exercise, remember to keep the elbow to the side and at a 90-degree angle.
Eccentric wrist supination

- This exercise can strengthen the wrist supinators.
- Start by holding one end of a dumbbell with your palm facing up.
- A, table or thigh may be utilized to support the forearm.
- Hold for 5-7 seconds and gently rotate the wrist inwards (pronation).
- To return the weight to its original position, the person can accomplish this with the free hand.
Half dumbell supination
- This exercise can strengthen the wrist supinators.
- Start by holding one end of a dumbbell with your palm facing up.
- Using pronation, internally rotate the wrist until the weight is level with the ground.
- Lower your wrists toward your back to lift the load back to the starting position.
Dumbbell supination
- This exercise can strengthen the wrist and forearm supinators.
- Begin by resting your forearm on a table, bench, or thigh.
- Start with your palms facing the floor and hold a small stop at one end.
- Take five-second steps and gently roll your wrists back, palms facing up. In the upward (concentration) phase of the movement, the person can support himself or the other hand.
Kettlebell goes down
- This exercise helps strengthen the wrists and forearms.
- Begin by resting your forearm on a table, bench, or thigh. Start with your palms facing the ground holding the kettlebell by the handle.
- Take five-second steps and gently roll your wrists back, palms facing up. In the upward (concentration) phase of the movement, a person can support himself with the other hand.
Band supination

- By doing this exercise, you can strengthen the wrist supinator.
- Place the tape on the palm, starting with the thumb, move it to the little finger, and wrap it once around the back of the hand.
- Hold the tape with your thumb.
- Hold the other end of the tape with your non-target hand.
- Turn the band so that the palm is now facing up as you start with the palm facing down.
- Do 10 repetitions and continue the cycle.
Isometric wrist supination

- This exercise uses the uneven weight distribution of a portable weight to avoid this rotator cuff exercise.
- This routine specifically mainly focuses on wrist supinators.
- Bend your elbow to a 90-degree angle and place a yoga block or rolled towel between your body and elbow to ensure proper form.
- Holding the handle of a kettle with your thumb for 10-15 seconds is similar to holding the handle of a cup.
Stretching exercises:
- gentle stretching exercises to improve muscle flexibility and relieve muscle tension in the forearm and wrist area.
Manual therapy:
- Manual techniques from a physical therapist can help reduce pain, improve joint mobility, and release muscle tension.
- Manual therapy techniques that may be used for supinator syndrome include:
Soft tissue mobilization:
Massage, myofascial release, or trigger point therapy to relax tense muscles and improve circulation.
Joint Mobilization:
Gentle, passive movements of the forearm and wrist joints to improve joint mobility and reduce stiffness.
Nerve gliding exercises:
- These exercises aim to improve the mobility and function of the intervertebral nerve by lengthening and gently gliding the nerve along its course.
- Nerve exercises are performed under the guidance of a physical therapist and can help reduce nerve irritation and improve symptoms.
Modality:
A physical therapist can use a variety of modalities to relieve pain and promote tissue healing. These may include:
Heat or cold therapy:
Applying hot or cold packs to the affected area can help relieve pain and reduce inflammation.
Transcutaneous Electrical Nerve Stimulation (TENS):
TENS devices deliver mild electrical impulses to the affected area to help reduce pain and promote blood flow.
Education and self-management:
- A physical therapist teaches proper body mechanics, ergonomics, and activity modification to prevent the worsening of symptoms.
- They can also advise on self-management strategies such as home exercises, ice cream techniques and pain management techniques.
- It is important to note that specific physical therapy procedures are tailored to the individual’s needs and the severity of symptoms.
- The treatment plan is prepared based on the general assessment of the physiotherapist.
- Regular follow-up visits with a physical therapist and adherence to the prescribed exercises and treatment plan are essential for optimal recovery.
- It is always recommended to consult a qualified physical therapist who can perform a thorough evaluation and develop a personalized treatment plan for supinator syndrome.
Post-operative rehabilitation
- Start active movement at 3-5. during the day
- Include extensor stretching
- Start strengthening after 3-4 weeks
- Patients can return to light work 2 to 3 weeks after surgery while returning to major activities can take 6 to 12 weeks.
FAQ
Near the supinator arch, the radial nerve divides into a superficial and posterior interosseous branch. The radial nerve supplies most of the extensor muscles of the forearm and hand. Injury to this branch of the radial nerve outcome in posterior interosseous nerve syndrome.
Posterior interosseous nerve syndrome is likewise named supinator syndrome since its source is the result of entanglement of the profound branch of the radial nerve at the grade of the supinator muscle.
Supinator. This muscle originates at the back of the forearm and is innervated by the deep branch of the radial nerve (arising from the posterior cord, nerve roots C5-T1), which becomes the posterior interosseous nerve.
Supinator. This muscle originates at the back of the forearm and is innervated by the deep branch of the radial nerve (arising from the posterior cord, nerve roots C5-T1), which becomes the posterior interosseous nerve.
Wartenberg syndrome is defined as an entanglement of the superficial branch of the radial nerve with just sensory manifestations and no motor disturbances. In this situation, the patient says distal radial forearm pain is associated with dorsal radial arm paresthesia.