The Radial Nerve
Table of Contents
What is Radial Nerve?
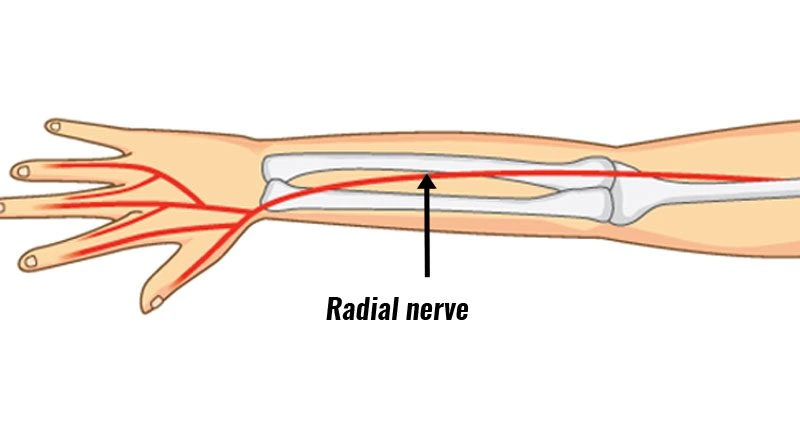
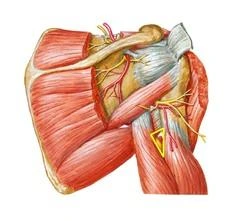
The Radial nerve is one in all the terminal branches of the posterior cord. within the axilla, it lies behind the axillary and upper brachial arteries and passes anterior to the tendons of the teres muscle, latissimus dorsi, and subscapularis. It arrives in the posterior compartment of the arm transient via a triangular space, formed by the lateral humerus, long head of triceps, and teres.
However this space, the nerve arrives at the spiral groove of the humerus. It descends obliquely between the lateral and medial heads of the triceps where it reaches the lateral border of the humerus within the distal third of the arm. The nerve arrives at the anterior compartment by penetrating through the lateral intermuscular division where it continues between brachialis and brachioradialis. Anterior to the epicondyle the nerve divides into its terminal superficial and deep branches.
The posterior cutaneous nerve of the arm arises within the axilla, piercing the deep fascia near the posterior axillary fold. The lower lateral cutaneous nerve of the arm arises before the nervus, pierces the intermuscular septum, and becomes cutaneous below the deltoid.
The nervus’s superior branch continues from the nervus anterior to the epicondyle. It moves with the anterolateral side of the forearm. Its sole function is sensory. within the distal third of the forearm, the nerve rises posteriorly from below the tendon of brachioradialis and pierces the deep fascia to become superior. It again divides into the digital nerves.
The deep branch of the musculospiral nerve or posterior interosseous nerve is entirely motor. It begins anterior to the epicondyle of the humerus and enters the posterior compartment of the forearm through the 2 heads of the supinator where it curves around the lateral and posterior surfaces of the radius. It descends between the deep and superficial extensor muscles and lies on the interosseous membrane and ends in an exceedingly flattened expansion.
Roots of Radial nerve
C5, C6, C7, C8, T1
Anatomical Course of Radial nerve
The nervus radialis is the terminal continuation of the posterior cord of the plexus brachialis. It includes fibers from nerve roots C5 – T1.
The nerve rises during the axilla region, where it’s located posteriorly to the arteria axillaris. It issues the axilla inferiorly (via the triangular interval), and supplies branches to the long and lateral heads of the triceps muscle.
The musculospiral nerve then descends down the arm, traveling during a shallow depression within the surface of the humerus, called the radial groove.
As it descends, the nervus wraps around the humerus laterally and supplies a branch to the medial head of the musculus triceps brachii. During much of its course within the arm, it’s in the course of the deep branch of the arterial blood vessel.
To enter the forearm, the nervus radialis runs anterior to the epicondyle of the humerus, via the cubital fossa. The nerve terminates by splitting into two branches:
Deep branch (motor) – stimulates the muscles in the posterior compartment of the forearm.
The superficial branch (sensory) –provides the cutaneous innervation of the dorsal hand and fingers.
Branches of Radial nerve
Muscular twigs within the arm: triceps, anconeus, brachioradialis, extensor carpi radialis longus muscles.
The superficial branch of the radial nerve: supplies haptic sensation to the dorsal aspect of the hand, the dorsal aspect of the primary to 3rd digits, and therefore the dorsal lateral aspect of the fourth finger (sparing the fingertips).
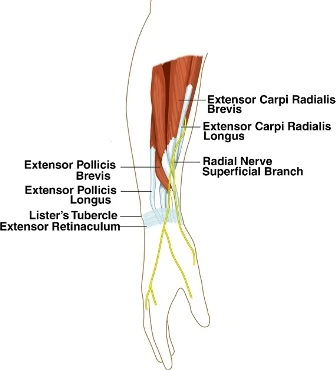
Deep branch of the radial nerve: direct stimulation to the extensor carpi radialis brevis and supinator muscles.
Continues because the posterior interosseous nerve provides the deep extensors of the dorsal arm (extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, extensor indices, extensor pollicis longus, extensor pollicis brevis, abductor pollicis longus).
Articular twigs to the elbow and wrist joints.
Structure and Innervations
Structure
The nervus is made as a continuation of the posterior cord of the nerve plexus and arises from the C5-T1 nerve fibers. It routes from the axilla to the posterior compartment of the arm, then into the anterior compartment of the arm, and keeps into the posterior compartment of the forearm.
Arm
The nerve derives from the posterior cord of the plexus brachialis and exits the axilla posteriorly to the arteria. It moves with the deep artery brachialis and gives two motor branches and one sensory branch before crossing the triangular interval. These motor branches stimulate the medial and long heads of the triceps. This sensory branch is termed the posterior cutaneous nerve of the arm which supplies cutaneous sensory innervation to a little of the distal posterior arm. After passing through the triangular interval, the nervus descends the radial groove before laterally wrapping around the humerus. The nerve provides a motor branch to the lateral head of the triceps follow by two sensory branches: the inferior lateral cutaneous nerve of the arm which penetrates via the posterior cutaneous and the lateral head of the triceps nerve of the forearm.
Forearm
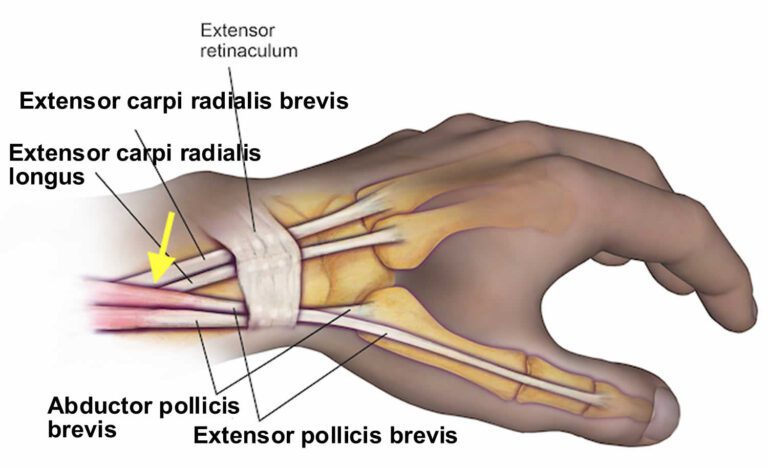
The posterior cutaneous nerve of the antebrachium also penetrates via the lateral head of the triceps but keeps stimulating a posterior strip of the forearm. After providing these two sensory branches, the radial artery travels via the lateral intermuscular septum to penetrate the anterior compartment of the forearm among the brachialis and brachioradialis muscles. The radial nerve then crosses over the lateral epicondyle into the cubital fossa and forearm. The radial nerve is divided into deep and superficial branches. The deep branch is a motor branch that crosses among the heads of the supinator muscle and becomes the posterior interosseous nerve to stimulate the muscles of the posterior compartment of the forearm. The superficial branch follows the radial artery inferiorly to the anterolateral part of the radius, deep to the brachioradialis muscle. The superficial branch then courses dorsally over the distal radius over the anatomical snuffbox to stimulate the posterior lateral three and a half digits (3/2) (the thumb, index, middle, and lateral half of the ring fingers) and the connected hand area.
Function of Radial nerve
The following may be a list of the motor and cutaneous sensory functions of the nervus radialis.
Sensory
Anterior aspect:
The inferior lateral cutaneous nerve of the arm – gives the impression of the anterior lateral quality of the mid-arm.
Posterior aspect:
The posterior cutaneous nerve of the arm – impression to the posterior distal arm.
The posterior cutaneous nerve of the forearm – impression to a peel posterior aspect of the forearm
Superficial branch – sensation to the posterior aspect of the thumb, index, middle, and lateral half of the ring fingers also because of the associated dorsal hand area.
Motor
The nerve branches off to the Deep Branch after it passes through the cubital fossa and so continues because the Posterior Interosseous Nerve after it passes between the supinator muscle heads.
Radial Nerve
Triceps brachii (medial and lateral heads) – gives the extension of the forearm.
Extensor carpi radialis longus – gives for the extension of the wrist.
Brachioradialis – gives flexion of the elbow as well as pronation and supination, depending on the position of the forearm.
Anconeus – gives for elbow extension.
Deep Branch of the Radial Nerve
Supinator – supinates the forearm.
Extensor carpi radialis brevis – extends and abducts the wrist.
Posterior interosseous nerve:
Abduct the thumb at the wrist – Abductor pollicis longus
Extends and adducts the wrist – Extensor carpi ulnaris
Extends the medial four digits of the hand – Extensor digitorum
Extends the index finger and to some extent wrist extension – Extensor indices
Extends the terminal phalanx of the thumb – Extensor pollicis longus
Extends the wrist and small finger – Extensor digiti minimi
Extends and abducts the thumb at the carpometacarpal and metacarpophalangeal joints – Extensor pollicis brevis
Embryology
The nerve could be a peripheral nerve that arises from the bilaterally paired neural crest which are strips of cells arising from the ectoderm at the margins of the exoderm during embryonic development. The migration of the neural crest cells eventually forms what becomes nervous during a fully developed body.
Blood Supply and Lymphatics
The nerve exits the axilla with the arterial blood vessel and follows it posteriorly with the artery. It then continues with the deep arteria brachialis into the posterior compartment via the triangular interval. The nerve follows the radial collateral artery till it covers anteriorly over the cubital fossa. Now the nervus radialis branches into the superficial branch of the nerve which passes with the artery, the deep branch of the arteria radialis, and also the posterior interosseous artery.
Nerves
The radial nerve forms as a continuation of the posterior cord of the brachial plexus with fibers of the nerve from the C5-T1 nerve roots.
The Radial Nerve branches
Sensory
The inferior lateral cutaneous nerve of the arm
The posterior cutaneous nerve of the arm
The posterior cutaneous nerve of the forearm
The superficial branch of the radial nerve
Motor
Deep branch of the radial nerve
Posterior interosseous nerve
Muscles
The nervus radialis and its branches provide innervation for the subsequent muscles (See Structure and performance for specific nerve branch innervations and muscle actions):
- Abductor pollicis longus
- Anconeus
- Brachioradialis
- Extensor carpi radialis brevis
- Extensor carpi radialis longus
- Extensor carpi ulnaris
- Extensor digiti minimi
- Extensor digitorum
- Extensor pollicis brevis
- Extensor indices
- Extensor pollicis longus
- Triceps brachii (medial and lateral heads)
- Supinator
Variation
The deep branch of the musculospiral nerve normally passes between the heads of the supinator muscle because it becomes the posterior interosseous nerve to innervate the muscles of the posterior compartment of the forearm. A variant can occur where the deep branch of the nerve passes through the Arcade of Frohse (Supinator Arch) which might increase the likelihood of impingement.
Surgical Considerations
Any surgery near the nervous holds a possible risk for an injury that is able to cause adverse downstream effects.
The nerve plexus injury with nervus involvement can occur with the utilization of sternal retraction after sternotomy, particularly with internal mammary dissection during cardiac surgery.
Damage to the superficial nerves may be a potential complication to surgery for de Quervain tendinopathy.
There is a theoretical risk of nerve injury with hyperextension of the elbow and therefore the forearm should be placed in a very slightly flexed position during anesthesia.
Clinical Significance
Radial nerve injuries are related to the trail it travels near the humerus. Mechanisms of injury are often humerus fracture, an instantaneous blow, or sustained pressure (i.e. from the incorrect use of a crutch). Motor function of the triceps is usually preserved as they’re innervated superiorly whereas wrist and digit extensors are often paralyzed resulting in the dropped wrist deformity.
A loss of synergic action among wrist and extensors leads to excessive and unnecessary wrist flexion. this will be observed in an exceedingly simple gripping task or asking the individual to create a fist. Both tasks are going to be difficult to finish as movement is going to be ineffective. Interphalangeal joints will be extended by the lumbricals and interossei thanks to their attachments at the dorsal digital expansion.
Due to overlapping cutaneous nerves, there’s only a tiny low patch exclusive to the nervus radialis on the dorsum of the thumb web.
Radial Tunnel Syndrome
Radial Tunnel Syndrome shows symptoms involving fatigue or dull, aching pain at the proximal part of the forearm while using it. Unusually, these symptoms can happen at the dorsal aspect of the wrist or hand. Radial Tunnel Syndrome generally happens secondary to overuse or repetitive motions from pushing, pulling, gripping, pinching, or bending at the wrist generally from employment or playing sports. Muscle overuse may cause compression of the musculospiral nerve anywhere along its path, but most ordinarily occurs over the elbow because it passes through the radial tunnel. Treatment for radial tunnel syndrome will be conservative or surgical if non-operative therapy fails.
Radial Nerve Palsy
Radial neuropathies occur from injury to the nervous because of compression, ischemia, fractures to the arm, or penetrating wounds. Wrist drop is the commonest presentation. The severity of the neuropathy depends on the extent of the injury. Surgical procedures like stabilization of an acute humeral fracture with humeral nailing also can cause radial neuropathies. Palsy of the nerve is additionally referred to as crutch palsy, Saturday night palsy, and honeymooner’s palsy, conditions which can occur after placing one’s arm over a chair (or crutches) for an extended period causing a pressure injury to the nerve.
Injury to the nerve may be broadly categorized into four groups – looking at where the damage has occurred (and thus which components of the nerve are affected).
In the Axilla
The nervus radialis is damaged within the axilla region by a dislocation at the ball-and-socket joint, or a fracture of the proximal humerus. Occasionally, it’s injured via excessive pressure on the nerve within the axilla (e.g. a badly fitting crutch).
Motor functions – the musculus triceps brachii and muscles in the posterior compartment are affected. The patient is unable to increase at the forearm, wrist, and fingers. Unopposed flexion of the wrist occurs, referred to as wrist drop.
Sensory functions – all four cutaneous branches of the nervus radialis are affected. there’ll be a loss of sensation over the lateral and posterior arm, posterior forearm, and dorsal surface of the lateral three and a half digits.
In the Radial Groove
The nervous is tightly bound within the spiral groove of the humerus. Thus, it’s most liable to damage with a fracture of the humeral shaft.
Motor functions
The triceps could also be weakened but aren’t paralyzed (branches to the long and lateral heads of the triceps arise proximal to the radial groove).
Muscles of the posterior forearm are affected. The patient is unable to increase at the wrist and fingers. Unopposed flexion of the wrist occurs, referred to as wrist drop.
Sensory functions – the cutaneous branches to the arm and forearm have already risen. The superficial branch of the nerves is going to be injured, cause to sensory loss to the dorsal surface of the lateral three and a half digits and also the connected area on the dorsum of the hand.
In the Forearm
There are two terminal branches of the radial nerve situated within the forearm. The typical mechanism of injury and impact of their injury vary:
| Superficial branches | Deep branches | |
| Mechanism | Stabbing or laceration of the forearm | Fracture of the radial head or posterior dislocation of radius |
| Motor functions | None | The majority of the muscles in the posterior forearm are affected. wrist-drop does not occur, as the extensor carpi radialis longus is unaffected, and maintains some extension at the wrist |
| Sensory functions | Sensory loss affects the lateral three and a half digits, and associated ara on the dorsum of the hand | None |
Radial Nerve Entrapment
Radial nerve injury or compression can occur anywhere along the nerve’s path which might cause extensor or supinator muscle denervation. this could lead to pain, weakness, dysfunction, or paresthesias and numbness along the sensory distribution of the nervus radialis. The proximal forearm is the most typical area of compression where the posterior interosseous branch of the musculospiral nerve passes between the supinator heads. Other, less common, sites of compression can occur because of fractures of the humerus about the center and proximal thirds of the shaft. The radial aspect of the wrist is another site of possible compression of the nerve. Treatment for musculospiral nerve entrapment depends on the pathology and should be treated conservatively or surgically if conservative measures fail.
Cheiralgia Paresthetica (Wartenberg syndrome)
Cheiralgia paresthetica may be a hand neuropathy commonly caused by trauma or compression of the superficial branch of the musculospiral nerve. The dorsum of the hand near the bottom of the thumb (in the vicinity of the anatomical snuffbox) is often affected; however, it’s going to affect the dorsum of the thumb, index, and hand. Symptoms involve pain, numbness, tingling, and a burning sensation. there’s no motor involvement since the superficial branch is solely sensory. Its etiology is assumed to be caused by a constriction of the wrist like a watch band or bracelet. it’s connected to handcuff use and is in addition commonly remarked as handcuff neuropathy.
Neuro Examination
Conduct your standard neurological examination. Look out for these signs:
Weakness:
- Wrist extension
- Abduction of thumb
- Diminished sensation:
- Back of thumb, index, middle, and 1/2 annualry
- back of forearm
- Abnormal reflexes
- Triceps
- Brachioradialis
- Neurodynamics
- The upper limb neurodynamic test for the musculospiral nerve (ULNT2b) is performed with the patient supine. The joints are moved sequentially and to the tip of range or until symptoms are produced. Patients are to be instructed to report the onset of any sensation like a stretch, tingling, or pain anywhere within the arm or neck.
ULNT2b sequencing:
- Shoulder girdle depression
- Elbow extension
- Shoulder internal rotation
- Pronation
- Wrist flexion
- Shoulder abduction
- If a sensation is provoked, differences between neurogenic and non-neurogenic sources of pain should be acted upon. this can be achieved by the addition of sensitizing movements distant to the pain such as:
Ipsilateral and contralateral cervical lateral flexion
Wrist extension or flexion
Shoulder girdle elevation
It is good practice to perform the test on the unaffected arm first, to determine what’s ‘normal’ for the patient. A ULNT is taken into account positive if it reproduced the patient’s symptoms and a neurogenic source of pain is identified.
FAQ
Which are the three branches of the radial nerve?
Muscular branches of the radial nerve:
Triceps brachii.
Anconeus.
Brachioradialis.
Extensor carpi radialis longus.Where does the musculospiral nerve run on the humerus?
The deep branch of the nervus or posterior interosseous nerve is entirely motor. It begins anterior to the epicondyle of the humerus and enters the posterior compartment of the forearm through the 2 heads of the supinator where it curves around the lateral and posterior surfaces of the radius.
What is the function of the radial nerve?
The nerve provides motor (movement) and sensory functions to the arm. It Stimulates muscles so you’ll straighten and lift your elbows, wrists, hands, and fingers. Provides touch, pain, and temperature sensations to portions of the rear of the upper arm, forearm, and to the rear of the hand and fingers.
Where is the musculospiral nerve possibly to be damaged?
A nervous injury refers to a break of the nerve within the upper arm. This nerve controls the triceps muscle. It also helps extend the wrist and fingers and provides sensation partly to the hand. The nervus radialis is near the bone within the upper arm, so it’s prone to injury, especially if the arm breaks.
What fingers does the nervous control?
The nerve gives feeling to the skin on the surface of the thumb and on the rear of the hand and also on the index, finger, and 1/2 of the finger.
What is nerve pain?
When the nerve reaches your elbow, it passes through the radial tunnel, which could be a collection of muscles. Radial tunnel syndrome occurs when the nerve is pinched or compressed because it enters the radial tunnel. This creates unwanted pressure on your musculospiral nerve, often causing nagging pain.
Is musculospiral nerve damage permanent?
Knives and glass, for instance, can directly transect the nerve and cause disability. However, the superficial branches of the musculospiral nerve are the foremost liable to this kind of injury, and infrequently there’s no significant permanent damage.




12 Comments