Intersection syndrome of the wrist
Table of Contents
What is Intersection syndrome of the wrist?
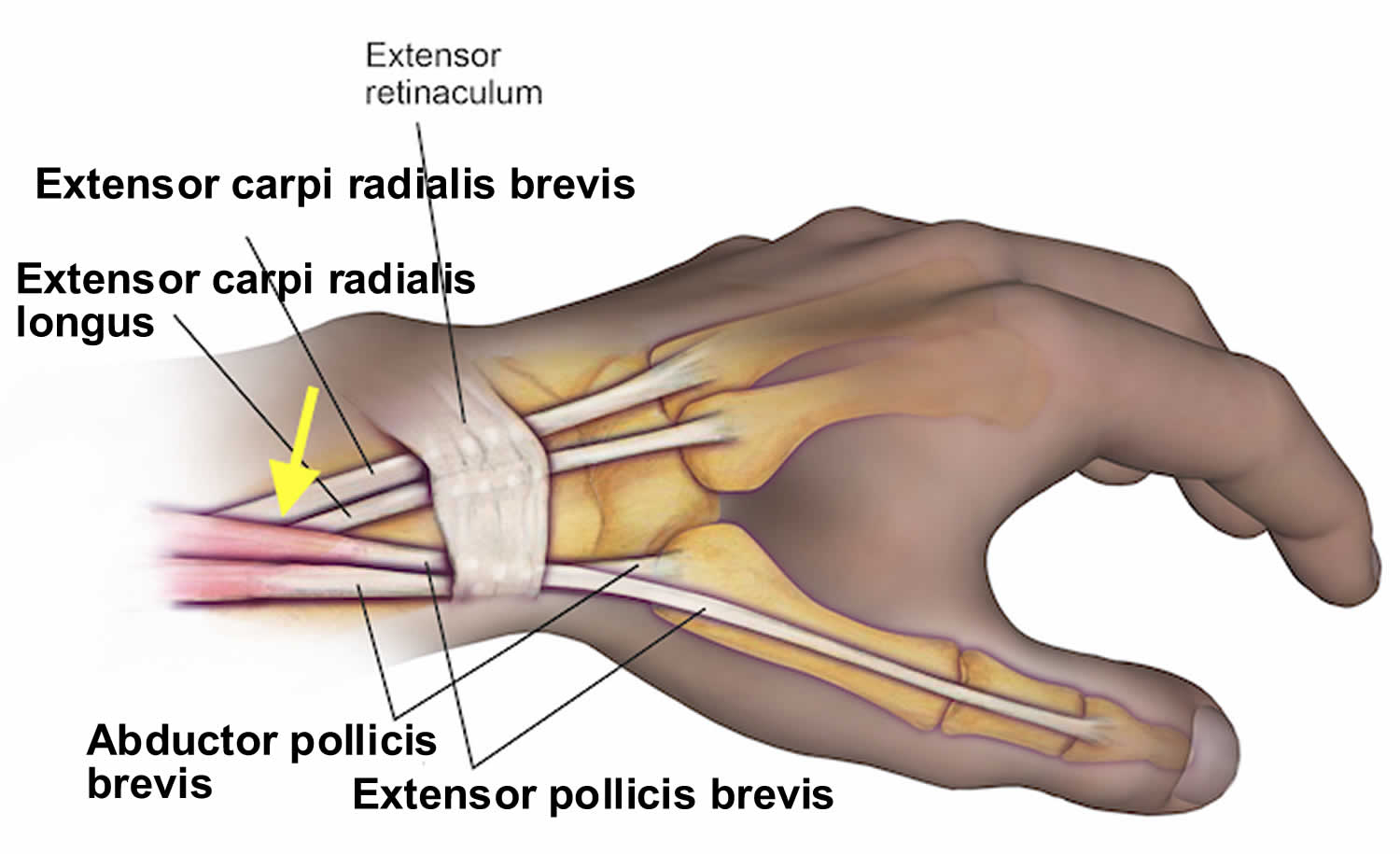
Intersection syndrome of the wrist is the condition that affects the first as well as second compartments of the dorsal wrist extensors. A condition is thought to happen as a result of repetitive friction at a junction in which the tendons of the first dorsal compartment cross over the second, creating the tenosynovitis. This is typically noted as the pain just proximal as well as dorsal to the radial styloid, or even also noted anatomically by 4 cm to 6 cm proximal to Lister’s tubercle.
The term “intersection syndrome” refers to an intersection (at the angle of around 60°) of the musculotendinous junctions of the first as well as second extensor compartment tendons. An intersection syndrome is a relatively uncommon disorder that is often misdiagnosed with other conditions, namely ‘De Quervain’s tenosynovitis.
In this condition, on the lateral side of a forearm when inflammation happens at the intersection of the muscle bellies of the abductor pollicis longus as well as extensor pollicis brevis cross over the extensor carpi radialis longus as well as the extensor carpi radialis brevis. This syndrome is the type of tenosynovitis resulting in pain in the lower forearm, usually a few inches from the wrist. The two muscles which control a thumb originate in a forearm, intersecting two wrist tendons before connecting to a thumb. Tendons are thick, rope-like structures that connect muscle to the bone. Each tendon is covered by the smooth, slippery tenosynovium which allows the tendons to glide freely over the surrounding tissues. Activities that involve frequent wrist motions may lead to inflammation of the tenosynovial lining known as tenosynovitis.
Anatomy of the wrist
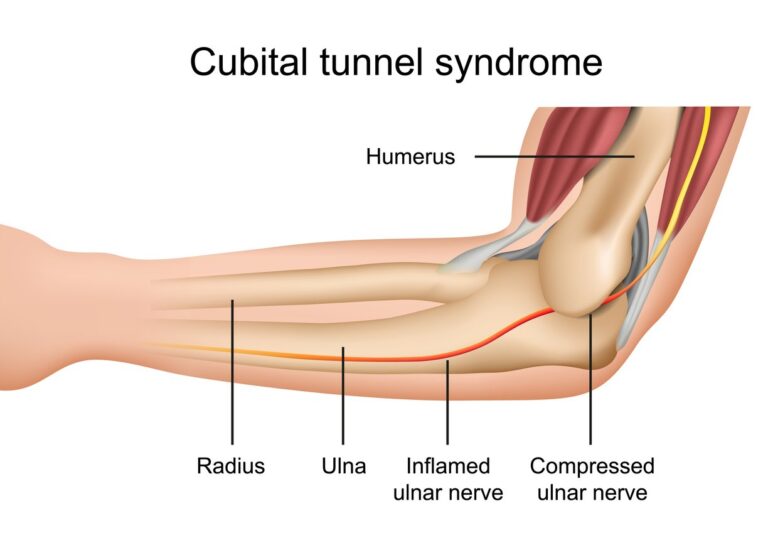
The wrist joint is a complex joint that bridges a hand to a forearm. It is the collection of multiple bones as well as joints. The bones comprising a wrist include the distal ends of the radius bone and ulna bone, 8 carpal bones, as well as the proximal portions of the 5 metacarpal bones.
Ligaments of the wrist
- Ligaments of the wrist are fibrous bands of tissue that connect one bone of the wrist to another. A wrist contains a network of ligaments, including:
- Extrinsic ligaments connect the wrist bones to the long bones of a forearm as well as the bones of the hand. Extrinsic ligaments mainly include several volar radiocarpal ligaments, volar ulnocarpal ligaments, as well as dorsal ligaments.
- Intrinsic ligaments connect the wrist bones to each other. Intrinsic ligaments include several proximal row ligaments, the distal row ligaments, and palmar midcarpal ligaments.
- Collateral ligaments: Strong ligaments on either side of the finger as well as thumb joints, which prevent sideways movement of the joint
- Volar plate: A ligament that connects a proximal phalanx to the middle phalanx on the palm side of the joint. As a joint in the finger is straightened, this ligament tightens to keep the proximal interphalangeal joint from bending backward.
- Radial and ulnar collateral ligaments: A pair of ligaments that bind the bones of a wrist as well as provide stability.
- Volar radiocarpal ligaments: The complex web of ligaments that supports the palm side of the wrist.
- Dorsal radiocarpal ligaments: These ligaments support the back of the wrist.
Wrist capsule
- The radiocarpal joint, where a forearm’s radius bone, as well as the first row of a wrist’s carpal bones, meet, is surrounded by a wrist capsule. The outer layer of this capsule is fibrous as well as contains some extrinsic ligaments.
- The capsule’s inner layer is made up of very thin tissue called a synovial membrane.
- The synovial membrane produces as well as holds in the special fluid, called synovial fluid. This fluid assists keep the joint lubricated.
Tendons of the wrist
- The movements of a hand, as well as wrist, are powered by tendons, which connect muscles to bones. The tendons which control a wrist originate from forearm muscles as well as inserted into hand bones. No tendons insert into the carpal bones themselves.
- Wrist tendons mainly include the:
- Tendons are involved in wrist flexion or even the action of bending the wrist forward/inward. These tendons also assist in rotating a wrist.
- Tendons are involved in wrist extension or even the action of bending the wrist backward. These tendons also assist move the wrist toward the thumb or even the little finger.
- Tendons are involved in finger flexion as well as extension, which passes by the wrist on their way to the fingers.
Muscles involved in the intersection of wrist syndromes

- Abductor pollicis longus
Origination: Posterior surface of the proximal half of radius bone, ulna as well as interosseous membrane
Insertion: Base of the metacarpal bone 1, (trapezium bone)
Action: At radiocarpal joint: Hand extension; Carpometacarpal joint of the thumb: Thumb abduction as well as extension
Innervation: Posterior interosseous nerve (C7, C8)
Blood supply: Anterior interosseous artery, posterior interosseous artery of the hand. - Extensor pollicis brevis
Origination: Posterior surface of the distal third of radius bone as well as interosseous membrane.
Insertion: Posterior aspect of the base of proximal phalanx of the thumb
Action: Carpometacarpal as well as metacarpophalangeal joint: Thumb extension
Innervation: Posterior interosseous nerve (C7, C8)
Blood supply: Posterior interosseous artery and anterior interosseous artery - Extensor carpi radialis longus
Origination: Lateral supracondylar ridge of the humerus bone, the lateral intermuscular septum of the arm.
Insertion: Posterior aspect of the base of metacarpal bone 2nd.
Actions: Wrist joints: Hand extension and hand abduction (radial deviation) as well.
Innervation: Radial nerve (C5-C8)
Blood supply: Radial recurrent artery, radial collateral artery, and radial artery as well. - Extensor carpi radialis brevis.
Origination: Lateral epicondyle of the humerus (common extensor tendon)
Insertion: Posterior aspect of the base of metacarpal bone 3rd.
Action: Wrist joints: Hand extension and hand abduction (radial deviation)
Innervation: Radial nerve (C5- C6)
Blood supply: Radial recurrent artery, radial artery as well as the deep brachial artery
Epidemiology
This syndrome occurs typically as the result of repetitive extension as well as flexion exercises or even activities. This is commonly seen in sporting activities, namely rowing or canoeing, skiing, racquet sports, as well as horseback riding. There is no significant difference in injury patterns found in men and women.
Pathophysiology
The repetitive extension and flexion result in the friction injury at the crossover junction of the first dorsal compartment (abductor pollicis longus as well as extensor pollicis brevis) and the second dorsal compartment (extensor carpi radialis brevis/extensor carpi radialis longus) tendons leading to the inflammatory response and subsequently the tenosynovitis as well.
This intersection is at the angle of approximately 60°, approximately 4 cm proximal to Lister’s tubercle (the bony protuberance on a dorsal surface of the distal radius). The presentation is typically one in which a patient complains of pain or even tenderness over a dorsal aspect of a wrist proximal to a radial styloid. There can also be swelling as well as crepitus that is palpable on the exam with wrist and/or thumb extension.
What causes Intersection Syndrome of the wrist?
- Tennis, skiing, rowing as well as weight lifting are all common culprits. In fact, any activity that requires a wrist to repeatedly move downward toward a thumb may lead to Intersection Syndrome. This movement causes the muscles as well as tendons in the wrist to rub against one another producing irritation and swelling as well. As the inflammation progresses, the tendons may no longer glide easily.
Signs and symptoms of Intersection syndrome of the wrist
- The symptoms of intersection syndrome are very predictable. Patients with the complaint almost always have the same symptoms. These symptoms typically develop a day or even two after the repetitive activity, namely sports or even gardening activity. Often this condition develops in competitive rowers a day or two after a particularly challenging workout session. Typical signs of intersection syndrome include:
- Pain as well as tenderness of the wrist tendons,
- Swelling of the tendons,
- The grinding sensation (crepitus) with the motion of the fingers,
- In rare circumstances where a diagnosis is unclear, an injection of the local anesthetic into the area may be helpful in making the definitive diagnosis. Individuals who have immediate relief of symptoms following injection directly at an intersection of these tendons will have the diagnosis confirmed.
How to Diagnose the Intersection syndrome of the wrist?
- Intersection syndrome is the clinical diagnosis, even though the musculoskeletal ultrasound may easily confirm it. The initial steps for diagnosis include the focused physical exam of an elbow, wrist, and hand.
- As with all musculoskeletal exams, the therapist must have a structured approach that includes inspection, the range of motion, palpation, muscle testing, as well as other special tests. Each joint above as well as below an injury should be tested in all movement. Look for swelling over a distal forearm as there may be some cases that present with the palpable finding on exam 4 cm to 6 cm proximal to Lister’s tubercle. Crepitus is a very common finding on an exam over the site of irritation. This is the finding that is specific to intersection syndrome. As the two dorsal compartments cross the motions of pronation as well as supination, create friction resulting in the exam finding of crepitus. Pronation is typically found more uncomfortable as compared to supination.
- When developing or even working through the differential diagnosis, resisted pronation which leads to the recreation of a patient’s pain, as well as the palpable finding of crepitus about 2 cm to 3 cm proximal to a radial styloid, may assist differentiate from tenosynovitis of De Quervain Syndrome. De Quervain Syndrome is the condition that also involves the first dorsal compartment of the wrist extensors, and it is condition is noted below the radial styloid as well as can be classically tested via the Finkelstein maneuver.
- Plain film imaging, as well as CT scan, will not be useful in a diagnosis of Intersection syndrome. MRI would give an excellent soft-tissue picture as well as diagnosis, even though MRI would not be the cost- or even time-effective choice.
- Ultrasound technology has pushed musculoskeletal medicine forward in both diagnoses as well as treatment provided by physicians. There have been some that say it may be as specific as MRI in the hands of a skilled person. Remember that as in most musculoskeletal conditions, anatomy is mostly superficial. Hence, the linear ultrasound probe is utilized.
- When observing Intersection syndrome under ultrasound, an ideal image is in the transverse plane on a short axis. The findings that would correlate to a diagnosis would be the hypoechoic area in between the two dorsal compartments as they are on top of each other. It represents swelling/edema as caused by friction. There can be a thickening of the tendon sheaths.
- Ultrasound can show peritendinous edema as well as fluid within the tendon sheaths at the intersection point between the 2nd as well as 3rd dorsal extensor tendon compartments.
- MRI typically shows features of peritendinous edema (peritendinitis) around the 2nd as well as 3rd extensor compartment tendons and extending proximally from the crossover point of the extensors pollicis brevis in the dorsal wrist.
Differential Diagnosis
De Quervain tenosynovitis (first extensor compartment involvement only, and located more distal at a radial styloid),
Extensors muscle strain,
Entrapment of a dorsal radial sensory nerve as it emerges beneath the brachioradialis (Wartenberg’s syndrome)
Thumb carpometacarpal arthritis
Extensor pollicis longus (EPL) tendinitis.
Treatment of Intersection syndrome of the wrist
Once symptoms have reduced, athletes may gradually return to action to ensure the problem is completely resolved. Even if there is no pain during performing the activity, too early the return can cause inflammation that is not apparent for several days. Hence, those early workouts when the athlete is returning from treatment are critically important. Having the athletic trainer or even a well-versed coach supervise this return to sport may assist to prevent the recurrence of the symptoms.
In some persistent situations, more aggressive management may be considered. Occasionally the cortisone injection is used to assist with management. In some situations, surgery to clean up the inflammation can be considered, but most patients will recover with 1-2 weeks of simple treatment. In very rare circumstances, surgical debridement (clean-up) of the tendons may be performed. During surgery, the abnormally tight tissue, called fascia, would be released from around the tendons to prevent the issue from coming back. The good news is that almost all patients may recover without having to undergo a surgical procedure for this problem.
Medical treatment
- Corticosteroid injection has shown significant improvement as well as is a known next best step if little or even no improvement has been made with other conservative treatments.
- Anti-inflammatory medications are can be helpful for acute injury as well as pain relief.
- Common medications are ibuprofen, naproxen, meloxicam or even diclofenac. Acetaminophen may be utilized for pain relief.
Physical therapy of Intersection syndrome of the wrist
Electrotherapy
- Ultrasound: Ultrasound therapy is used to decrease pain as well as swelling
- (TENS)Transcutaneous electrical nerve stimulation: TENS modality is used for the reduction of pain as well as inflammation.
- Deep therapy: Use to reduce pain.
Massage Techniques
- Massage therapy is an age-old therapy that uses both stretching as well as pressure in the rhythmic flow. Massage therapy assists in decreasing tension in specific muscles that have built up owing to injury or stress. Massage therapy assists a person to get blood flowing which speeds up the recovery process at any level.
- Some benefits of massage:-
Decreasing stress and improving relaxation.
Reducing pain and muscle soreness as well as tension.
Increasing circulation, energy, and alertness.
Lowering heart rate as well as blood pressure.
Increasing the immune function of a body.

- Effleurage (Stroking) technique
The hands are passed rhythmically and continuously over a patient’s affected part, in one direction as well as straight only, with the goal of improving blood flow in that direction, stretching tissues, relaxing a patient, and aiding the dispersal of waste products. This technique involves the stroking movements of the hands sliding over the skin of a wrist as well as is always the first and last technique applied in the massage session. Effleurage may be used with varying tempo and pressure according to the stage of the situation as well as whatever the desired effect of a massage is. - Petrissage (Kneading) technique
The affected skin is lifted, pressed down and squeezed, pinched, as well as roll. Alternate squeezing as well as relaxation of the tissues stimulates the local circulation as well as may have a pain-relief effect with some muscular disorders. The basic movement is to compress, pick up, as well as after that release the soft tissues. This is generally used when a deeper effect as compared to effleurage is wanted, more interestingly it is techniques include: - Squeezing
To begin with, tell a patient to take a comfortable position, supine or even sitting. After that, a physical therapist applies the squeezing technique, and the circular hand stroke is used for the entire wrist the technique uses the circular motion. A physical therapist will bring the tissue between a patient’s two hands lifting it up and away from the body. - Picking up
To start with, the therapist gives a command to a patient that takes a comfortable position, that pick-up technique applying equal pressure on the sides of the tissue and lifting it away from a body. The hands of a physical therapist are parallel to a limb being treated to avoid hyperextension of an outer wrist. - Shaking
A vibration or even shaking massage technique is the fine, gentle, trembling movement performed with hands or even fingers. Shaking may be used to stimulate soft tissues in the body. Vibration motions may assist to stimulate nerves, relieving muscular tension as well as reducing stress. This technique is mainly performed by hands, a clinician should put one hand on the other hand as well as place it on the affected side while stroking give vibrations. - Rolling
A skin rolling technique is performed using a thumb and fingers to pull the skin away from the tissue. This is then rolled forwards in constant motion to assist separate it from being stuck in muscle. Skin rolling may be used around areas of scar tissues to assist in breaking them down. - Wringing
A wringing technique consists of lifting and squeezing the muscle forwards as well as backward movement. Wringing is used to treat tight muscles, for relaxation, and as part of the post-event massage. The benefits of wringing are relief of tight muscles, decreased DOMS as well as improved recovery. - Myofascial Release
A myofascial release technique is manual for stretching a fascia aiming to reduce fascia restrictions. Fascia is situated between the skin as well as the underlying structure of muscle and bone and connects the muscles, organs, as well as other skeletal structures in the body. Fascia may become restricted through injuries, stress, trauma, or poor posture. Three strokes have been provided to a tight muscle. A physical therapist should place one hand on the other as well as apply stroking on the affected part to release tightness. - Trigger Point Therapy
Trigger point therapy involves an application of pressure to tender muscle tissue to decrease pain as well as dysfunction in other parts of the body. Trigger points are active centers of muscular hyperactivity, which often cross over with acupuncture points in the body. - Deep Transverse Frictions
These are transverse connective tissue therapy applied directly by a physical therapist’s fingers. Oscillating pressure is provided across the direction of the tissue fibers. Mainly used on a tendon or ligament injuries to help break down thickened, pain-producing scar tissue. - Compression Massage
In this helpful technique, rhythmic compression into muscles is used to originate deep hyperemia and softening effects in the tissues. This technique is often used for sports massage as the warm-up for deeper, more specific massage work. - Cross-Fibre Massage
Cross-fiber friction massage techniques are applied in a general manner to create the stretching and broadening effect in large muscle groups of a wrist or on site-specific muscle and connective tissue, deep transverse friction is applied to reduce adhesions and to help in creating strong, flexible repair while the healing process. - Palm Massage
Target the muscles in the hand to decrease sore wrists. Open an affected hand. Place a thumb of the unaffected hand into the base of an affected thumb as well as wrap the fingers around the back of the affected hand. Gently move a thumb in circles as a patient feel that release tension in the large thumb pad. - Tennis Ball Roll
Hold onto the tennis ball between both hands with the palms open. Vigorously roll a ball between the hands to reduce muscle tension as well as wrist pain. If a patient cannot find the ball, use the smooth rock, the frozen water bottle, or a patient’s car’s gear shift to rub out tense hand muscles.
Exercises for Intersection syndrome of the wrist
Stretching exercises
Stretching exercise may increase the performance in physical tasks, reduce the risk of injuries, assist the joints to move through their full range of motion, increase muscle blood flow, Enable the muscles to work most effectively, as well as increase the ability to do daily tasks.
- Praying position stretching
Tell a patient to take the standing position, as well as place the palms together in the praying position. Have the elbows touch each other. The patient hands should be in front of the face. The patient’s arms should be touching each other from the tips of the fingers to the elbows. With the palms pressed together, slowly spread the elbows apart. Do this exercise during lowering the hands of a patient to waist height. Give a command to a patient to Stop when the hands are in front of a belly button or a patient feels a stretch. Hold the stretch for thirty seconds, after that repeat three times in one session. Do three sessions in one day.

- Wrist extensors stretching
Give the commands to a patient to extend an affected arm in front of a patient at shoulder height, as well as keep the palm down, facing the floor. Relax a wrist so that the fingers point downward. With a free hand, gently grasp the fingers as well as pull them back toward the body. Hold for thirty seconds in one repetition. Do three times in one set per session. Three sessions in a day. - Clenched fists
Tell a patient to take the sitting position, as well as place the open hands on the thighs with palms up. Close the hands slowly into fists, but do not clench the fingers too tightly. With the forearms touching the legs, raise the fists off of a patient’s legs and back toward a patient’s body, bending at a wrist. Hold for thirty seconds. Lower the fists and slowly open the fingers wide. Repeat three times in one session. Do three sessions in one day. - Hooked stretching exercise
To begin with, to do this stretching exercise, hook one elbow under another and pull both arms towards the center of the torso. A patient should feel the stretch in the shoulders as well as wrap one arm around the other arm so that the palms are touching each other. Hold the position for thirty seconds. Do three repetitions in one session. Do three sessions in one day. - Finger stretching exercise
To embark with, to do this stretching exercise, bring a pinky finger and ring fingers together. Separate a middle finger as well as index fingers from the ring finger. Hold for thirty seconds per repetition. Do three repetitions in one session. Repeat three sessions in one day.

- Fist-opener
First of all, Make the fist as well as hold it for thirty seconds in front of a therapist. Stretch the fingers until a hand is flat and open, with the fingers together. Repeat this action three times in one session. Do three sessions in one day. Hold for thirty seconds. - Thumb pull
To do the stretching exercise, grab a thumb with the other hand. Gently, pull a thumb backward, mild away from a hand. Hold the stretching position for thirty seconds during one repetition. Do three repetitions per session. Do three sessions in one day. Repeat it on the other thumb also. - Alternate finger stretch
To do the stretching exercise, bring the middle finger and ring fingers together. Separate a pinky finger and index fingers from them. Repeat the stretching three times in one session. Do three sessions in a day. - Wrist Extensor Stretch with extended arm
To start with, by extending both of the arms in front of a patient’s face. Make two fists, like a patient is punching the air. Move the fists downward, while keeping the arms straight. Hold for thirty seconds and do three repetitions per session. Repeat three sessions per day. - Wrist Flexor Stretching exercise
First of all, the physical therapist tells a patient to put the arms in front of the patient himself/herself as well as make a fist with the hands. Open both of the hands, as if a patient was pushing on the wall in front of himself/herself. Take the right hand and pull the fingers back on a patient’s left hand as well as hold for thirty seconds. Repeat on the other hand also. Repeat three times per session. Do three sessions in one day. - Side to Side Stretching
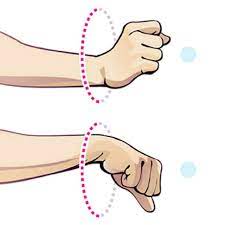
To start with, the therapist tells a patient to take a tabletop position with the knees and hands on the ground. Move the fingers outwards, they should be facing away from each other hands. Move from side to side, as well as hold for thirty seconds. Do it three times in one session. Do three sessions in a day. - Wrist Circle stretching exercise
First of all, the therapist tells a patient to take the sitting position with the hands-on table. Let the wrists hang off an edge. Make a circle with a wrist going clockwise. Then make the circle go anticlockwise. Hold at the end for thirty seconds. Repeat three times in one session. Do three sessions in one day. - Wrist Circle stretching exercise
To start with, tell a patient to take the sitting position with the hands-on table. Let the wrists hang off an edge. Make a circle with the wrist going clockwise. Then make the circle go anticlockwise. Hold at the end for thirty seconds. Repeat three times in one session. Do three sessions in a day. - Seated Clenched Fists
To begin with, the physiotherapist tells a patient to take the sitting down position and put the hands on the thighs. The palms should be facing up. Slowly, make a fist with both hands. After that, bend the wrist slightly so that it is facing toward a patient. A patient should make sure to keep the arms on the thighs. Hold for thirty seconds. Gradually open the fists. Do it three times in a session. Do three sessions in a day. - Palm Pulses stretching exercise
To start with, the physical therapist tells a patient to take a tabletop position with the knees and hands on the ground. Spread the fingers wide. Live the palms off the ground while keeping the fingers on the floor. Move or pulse the palms down to up ten times. - Thumb and upper wrist stretching exercise
Give a command to a patient to put the right arm out and make a fist around a thumb. Bend a fist down toward the ground. A patient will feel the stretch in the top of the wrist and a thumb. Hold for thirty seconds and repeat on the other hand. Do three repetitions in one session. Do three sessions in a day. - Figure Eight
First of all, the therapist tells a patient to interlace the hands with the elbows at the sides. Make the figure eights with the patient’s hands and hold for thirty seconds. Do three repetitions in a session. Do three sessions in a day. - Palm to ceiling wrist stretching exercise
To begin with, give a command to a patient that extends one arm in front of a patient’s face as well as palm facing toward the ceiling. Bend a wrist so that the fingertips point toward the floor. Using the other hand, gradually, pull the fingers toward the body till a patient feels the stretch in the underside of the wrist. Hold for thirty seconds. Repeat the exercise. Do it three times in a session. Do three sessions in a day. - Finger tendon glide stretch
First of all, the fingers extended straight out in front of a patient. Make the hook fist first, as well as return to the straight hand. Make the full fist, then return to the straight hand. Make the straight fist, after that return to the straight hand. Repeat this action ten times per session. Do three sessions in a day. - Thumb stretching exercise
To begin with, the physical therapist tells a patient to hold the hand out in front of the patient’s face, as if a patient is saying stop. Start with the thumb positioned outward. Move a thumb across the palm as well as after that back to the embarking position. - Wrist extensors stretching with the use of a table
To begin with, the physical therapist tells a patient to stand at the table with the palms down, fingers flat, as well as elbows straight. Lean the bodyweight forward. Hold it for thirty seconds. Repeat three times per session. Do three sessions in a day. - Basic Wrist Stretching exercise
The basic wrist stretching exercise is an excellent way to alleviate stiff joints in a wrist, especially after long days of typing as well as writing. To start with, hold the right hand out in front of a patient’s face with a palm facing upwards. Grip all four fingers with the opposing hand. Slowly, pull the fingers down towards the floor. Hold the stretch for 30 seconds, after that release the hand back to a starting position. Repeat with the other hand, holding for 30 seconds. Repeat it three times in a session. Do three sessions in a day. - Wrist stretching exercise using a table
To begin with, the physical therapist gives the command to the patient to place both the palms face down on the edge of the table. Fingers point away from a patient’s body. Keep the elbows straight, as well as gradually lean the bodyweight slightly forward. Then, reverse it! Place both of the palms face down on the edge of the table with fingers pointing toward the body. Keep the elbows straight, as well as gently lean the bodyweight back away from a table. - Reverse Prayer Stretching exercise
Place the backs of the hands together in front of a patient’s body and press the elbows toward the ground without letting the backs of the hands come apart until the stretch is felt in the forearms. - Loosen-up stretching exercise
This exercise is a simple stretching exercise to loosen up the fingers and hands before a patient begins exercising. It is also a good break to relax the wrists as well as hands if a patient is doing repetitive hand movements. Sit comfortably and after that bend an arm at the elbow at the right angle. Make the fist first, and then gradually open it spreading and stretching the fingers apart. Repeat three times in a session. Do three sessions in a day. In every repetition hold for thirty seconds. - Backward facing wrist stretch exercise
Place the hands out in front of a patient, rotating the wrists around so that a patient’s fingers are facing the knees. Start with the fingers closer to a patient’s knees. Keeping the palms flat on the ground, shift the body back toward the heels, and after that forward toward the hands. Do three repetitions in one session. Hold for thirty seconds in a single repetition. Do three sessions per day. - Forward-facing wrist stretching exercise
To start with, the hands are flat on the floor in front of a patient with fingers facing forward. Make sure that the elbow pits are facing forward and pulse forward for three repetitions. Holding for thirty seconds in one repetition per session. Do three sessions in a day.
Active-assisted range of motion exercise
- Active-assisted wrist flexion
First of all, the physical therapist tells a patient to take a comfortable position, such as sitting on a chair and affected hand relaxed on the edge of a table with full pronation. After that, place a rolled towel under the affected hand. Next, a physical therapist takes his/her position opposite the patient. A clinician gives commands to a patient to try to move the wrist down, when a patient is unable to move his/her hand during that time the physiotherapist provides the help to a patient to reach the entire range. Perform it ten times per session. Do three sessions per day. - Active-assisted wrist extension
To start with, tell a patient to take a comfortable position, namely sitting on the chair, and the affected hand should be relaxed on the edge of a table with full pronation. After that, place the rolled towel under the affected hand. Next, a physical therapist takes his/her position opposite the patient. Then, a therapist gives a command to a patient to try to move the wrist upward, when a patient is not able to reach the end range during that time a physical therapist provides assistance to reach the entire range. Do the motion ten times per session. Do three sessions per day. - Active-assisted wrist ulnar deviation
Tell the patient to take a comfortable position, namely sitting on the chair, and the affected hand should be in mid-supination. After that, place the rolled towel under the affected hand. Next, a physical therapist takes his/her position opposite a patient. Then, a physical therapist gives the command to a patient to try to move the wrist down, and when a patient is stopped while performing the motion, then a clinician helps a patient to reach the end range. Do this action ten times in one session. Do three sessions per day.

- Active-assisted wrist radial deviation
First of all, tell a patient to take a comfortable position, namely sitting on the chair, and an affected hand should be in a mid-supination position. Next, place a rolled towel under the affected hand. After that, a physical therapist takes the position opposite a patient. Then, a physical therapist gives a command to a patient to try to move the wrist up, as well as when a patient is stopped while acting, then a clinician helps a patient to reach the end range. Do it ten times in one session. Do three sessions per day. - Active-assisted supination
To start with, tell the patient to take a comfortable position, such as sitting on the chair with the affected hand should be in full pronation position, meaning the front of the hand will be facing the floor. After that, place the rolled towel under the affected hand. Next, a physical therapist takes the position opposite a patient. Then, a clinician gives a command to a patient that tries to rotate the wrist as well as when a patient stops the movement, a physical therapist provides outside force to reach the entire range of supination. do this action ten times in a session. Do three sessions per day. - Active-assisted pronation
To embark with, tell a patient to take a comfortable position, namely sitting on a chair with the affected hand should be in the full supination, meaning the palm will be facing the ceiling. After that, place the rolled towel under the affected hand. Next, a physiotherapist takes the position opposite the patient. the clinician gives a command to the patient to try to rotate the wrist and when a patient is unable to reach the end range and stops at any point, a physiotherapist helps the patient to perform the entire range. Do it ten times per session. Do three sessions in a day. - Active-assisted finger flexion
To start with, place the hand with the affected finger flat on a table, with palm up. Then, a physical therapist gives the command to a patient to bend the fingers inward, but when the patient cannot able to do full finger flexion due to pain or stiffness, the clinician helps the patient to reach full range. Then, straighten the fingers. Repeat it ten times per session. Do three sessions in a day. - Active-assisted finger extension
To begin with, place the hand with the affected finger flat on a table, with a palm up. Next, a physical therapist will give the command to the patient to straighten the fingers, but when a patient cannot do full finger extension because of pain then the therapist helps the patient to complete the finger extension. After that, relaxed the fingers. Repeat it ten times per session. Do three sessions per day. - Active-assisted thumb flexion
First of all, ask a patient to take a comfortable position, namely, sitting on a chair as well as a hand should be in mid-pronation. After that, the rolled towel is placed under the affected hand. Next, the clinician gives a command to a patient to bend the thumb down so that a gentle stretch is felt. The finger will cross a palm. Repeat it ten times per session. Do three sessions in a day.

- Active-assisted finger extension
To begin with, place the hand with the affected finger flat on a table, with the palm up. After that, a therapist will give a command to a patient to straighten the fingers, but when the patient cannot do full finger extension due to pain then a physical therapist assists a patient to complete the finger extension. Relaxed the fingers. Repeat it ten times in one session. Do three sessions in a day. - Active-assisted thumb flexion
To embark with, ask the patient to take a relaxed position, such as sitting on the chair and the hand should be in mid-pronation. Next, a rolled towel is placed under the affected hand. Then, a physical therapist gives the command to the patient to bend the thumb down so that the gentle stretch is felt. The finger will cross the palm. Repeat it ten times in a session. Do three sessions per day. - Active-assisted thumb extension
To start with, tell the patient to take a relaxed position, such as sitting on the chair and a hand should be in mid supination position. A rolled towel is placed under the affected hand. Then, a clinician gives a command to a patient to stretch the thumb outside meaning slightly posteriorly to a palm, but when a patient is unable to reach the full range, a physical therapist gives the assistance to do a full thumb extension. Repeat it ten times in a session. Do three sessions per day. - Active-assisted thumb abduction
First of all, the clinician tells the patient to take a comfortable position, such as sitting in the chair with a rolled towel under the affected hand, but a hand should be in a mid pronation position. After that, tell the patient to stretch the thumb out from the palm as if a patient is opening it up to hold the large jar, but remember that stretch at a big thumb knuckle, is not at the tip. Repeat it ten times in one session. Do three sessions per day. - Active-assisted thumb opposition
To start with, tell a patient to take a comfortable position, namely sitting on the chair. Next, touch a thumb to the tip of each finger. When a patient can do this exercise effortlessly, then touch further down on each finger till a patient is able to touch the base of each finger. Repeat it ten times per session. Do three sessions in one day.
Active range of motion exercise
Increase movement at a wrist joint, increase the function of the wrist joint as well as the whole limb, increase movement efficiency, improve the independence of the fine moments, decrease pain at the wrist, and improve and maintain joint integrity.
- Active wrist supination
Tell a patient to take a comfortable position means to stand or even sit with an arm at the side with the elbow bent to 90 degrees, with the hand in a mid-range over the edge of a table. Tell a patient to move their hand upward facing the roof without holding it at the endpoint. Do it ten times per session. Do three sessions in a day. - Active wrist pronation
A physical therapist should give a command to a patient to take a comfortable position means to stand or even sit with the arm at the side with the elbow flexed to 90 degrees, with a hand in the mid pronation over the edge of a table. Tell a patient to move their hand downward facing the ground without holding it at the endpoint. Do it ten times per session. Do three sessions per day. - Active wrist extension range of motion exercise
To start with, place the forearm on a table on a rolled-up towel for padding with the hand hanging off the edge of a stable surface, such as the table with palm down. A physical therapist should give a command to move the hand upward until a patient feel the gentle stretch. Next, return to the embarking position. Do it ten times per session. Do three sessions in a day. - Active wrist flexion range of motion exercise
First of all, tell a patient to place a forearm on the table on a rolled-up towel for padding with the hand hanging off to the edge of a stable surface, such as the table with the wrist, is in full pronation. After that, a clinician should give a command to move the hand downward until a patient feel a mild stretch. Next, return to the starting position. Do it ten times in a session. Do three sessions per day. - Wrist circles to increase range of motion
To begin with, a clinician should give a command to a patient to take a comfortable position, such as sitting on a chair. After that, bring the hands up with the elbows close to the body, making fists. Next, rotate the wrists in a circular motion. Then, try to keep the palms facing down to maximize the range of motion. Do 15 circles in each direction per session. Do it in opposite direction also (anticlockwise). Do three sessions in a day.
- Wrists Shakes
To start with, tell a patient to take a namaste position of a hand. Next, simply shake the wrists out ten times in a session. Do three sessions in a day. - Shake It Out
Shaking out the wrist and hands after staying in the same position for a while is a great mode to reintroduce blood flow as well as relieve the stiffness of the joints. To start with, the hands are out in front of a patient as well as palms facing the floor. Slowly shake the hands by letting the wrist go limp. Continue for 15 to 20 times. Repeat up to three times in a set. One set in a session is enough. Do three sessions in a day. - Fist to Fan
To start with, the hands in front of a patient as well as palms facing downwards. Make a fist with both hands. Open a fist halfway so that the finger is bent at the knuckles. Hold for 10 seconds. Open the hands fully so all five fingers are straight and spread wide apart. Hold for ten seconds per repetition. Do five times in a session along with three sessions in a day. Re-make a fist, as well as repeat the routine. - Thumb Touches
This exercise assists to increase coordination in the thumb and forefingers, and aids to reintroduce blood flow back to the affected area: Hold the hands outwards with the palms facing the ceiling. With the affected hand, slowly bring a thumb to touch the tip of every finger. Repeat on the other hand as well. Next, return to the starting position. Repeat five times with both hands per session. Do two sessions in a day. - Wrist flexion in supination
To start with, tell a patient to place the forearm on the table on a rolled-up towel for padding with the hand hanging off the edge of the stable surface, namely a table with palm down. A physical therapist should give a command to move the hand upward until a patient feel a mild stretch. Then, return to the starting position. Do it ten times per session. Do three sessions in a day. - Wrist extension in supination
First of all, the clinician gives a command to a patient to place the forearm on the edge of the table on the rolled-up towel for padding with a hand, which is in full supination position. Next, a physical therapist should give a command to move the hand down till a patient feels the gentle stretch. Then, return to the beginning position. Do ten repetitions in a session. Do three sessions per day. - Active wrist ulnar deviation
To begin with, it is the responsibility of a therapist to give a command to a patient to take a comfortable position with the support of the forearm on a table on the rolled-up towel for padding or on the knee, along with a thumb upward in position. Move the wrist down through a full range of motion. Do it ten times per session. Do three sessions in a day. - Active wrist radial deviation
To start with, a physical therapist gives a command to a patient to take a comfortable position with the forearm supported on a table on the rolled-up towel for padding or on the knee, with a thumb upward in position. After that, move the wrist up through the entire range of motion. Do exercise ten in a session. Do three sessions in a day. - Active thumb flexion
First of all, a physical therapist gives a command to the patient to take a comfortable position with the forearm supported on the table on a rolled-up towel for padding or on the knee. A thumb is positioned outward. Move a thumb across the palm as well as back to the starting position. Do it ten times in a session. Do three sessions in a day. - Active thumb extension
To start with, a physical therapist should give a command to a patient to take a comfortable position with the forearm supported on a table on a rolled-up towel for padding or on the knees. The thumb is positioned outward direction. After moving a thumb across a palm then come back to the embarking position as well as move slightly backward but not in abduction. Do ten repetitions in a session. Do three sessions per day.
Strengthening exercise
- Grip strengthening
Grippers come in several types of tensions. A patient can start with the one that is only a little difficult to move. When a low weight becomes easy, improve the gripper tension. Grippers range begins from light to ones requiring 365 pounds of pressure to close(move).
Tell a patient to sit comfortably with an arm bent at 90 degrees, with palm facing in, holding the gripper in one hand. Next, squeeze slowly, as well as release it without holding at the endpoint. Repeat 10 to 20 times in a session, and do three sessions in a day. Only a hand should be moving, not the whole arm. Switch the hand as well as repeat. When a patient can comfortably do three to four sets, try the gripper with more tension.

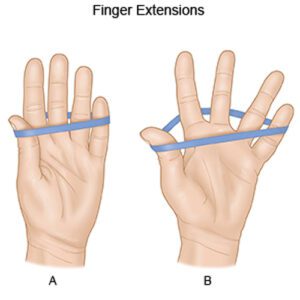
- Rubber band strengthener
The rubber band strengthening exercise is simple, but, it works the smaller hand muscles. It is also one a patient can do sitting at the desk or even anywhere else. Tell a patient to take an ordinary rubber band available at home and stretch it around the tops of the fingers and the thumb. After that, slowly open a hand to stretch against a rubber band, and after that slowly close a hand. Keep the motion-controlled. Repeat 10 times in a session. Do three sessions in a day.
- Fist to jazz hand
To begin with, tell a patient to rest one arm on a table like a patient is about to arm-wrestle someone. Next, make the fist. Next, slowly open a fist and stretch the fingers out as wide as a patient can comfortably go (do a jazz hand). Repeat 10 times per session. Do three sessions in a day. - Finger spread-apart with theraband
To embark with, wrap the theraband around each of the fingers. After that, push against the resistance from a band, and then spread fingers as far apart as possible. Hold for ten seconds, after that release it. Continuously do ten times, then switch a theraband to the other hand as well as repeat. Do it ten times in a session. Do three sessions in a day. - Dumbbell Windshield Wipers
To start with, place the forearm on a stable as well as a flat surface like a table or even a chair. After that, hold one end of the lightweight dumbbell (around two to five pounds) in the affected hand. Rotating a wrist from right to left, lift and lower the dumbbell in the windshield wiper motion. Do continuously for ten repetitions per session. Do three sessions in a day. - Ball Squeeze
First of all, telling a patient to grasp the ball in one hand means the affected hand can be squeezed, namely the stress ball, tennis ball, or racquetball. Squeeze a ball with all the affected fingers for ten seconds and then relax. Repeat ten times in a session. Do three sessions in a day. After 5 to 6 days increase repetitions from 10 to 20, according to a patient’s ability.

- Wrist extensors strengthening with the dumbbell in pronation
To start with, on the affected wrist strengthening exercise, tell a patient to sit in the chair with the forearm resting on the table. After that, hang the wrist as well as hand over the edge of the table. Hold the 2 or 3-pound dumbbell on the affected hand. Then, with a palm facing down, slowly lift a hand, so the back of the hand moves towards the ceiling. A patient’s forearm should remain on a table. Next, a physical therapist should give a command to move the hand in the upward direction as far as he/she can and then come back to the normal position. Do it ten times in a session. Do three sessions in a day. After 5 to 6 days, a clinician must apply hold at the endpoint for ten seconds in one repetition. - Dumbbell wrist flexors strengthening in pronation
To embark with, tell a patient to sit on the chair with the forearm resting on the table. Next, hang the wrist and hand over the edge of the table. Hold the 2 or 3-pound dumbbell in the affected hand. After that, with the palm facing down, slowly flex a wrist down so that the palm moves down the ground. Without holding at the endpoint tell a patient to perform ten repetitions per session and then release. Do three sessions in a day. After 5 days, a physical therapist must give a command to a patient to hold for ten seconds in one repetition, for strengthening the muscles. - Wrist extensors strengthening with a dumbbell in supination
To start this wrist strengthening exercise in the full supination, tell a patient to take the sitting position on the chair with a forearm resting on the table. Next, hang the wrist and hand over the edge of a table. Hold the 2 or 3-pound dumbbell in the affected hand. Then, with a palm facing up, slowly move a hand down, so the back of the hand moves towards the floor. A patient’s forearm must remain on a table. Then, a clinician should give a command to move their hand in the downward direction as far as he/she can and then come back to the normal position. Do it ten times per session. Do three sessions per day. After 5 days, a clinician must give the command to a patient to hold at the endpoint for ten seconds in a repetition. Do two sessions in a day. - Wrist flexors strengthening with a dumbbell in supination
To start this wrist strengthening exercise, first of all, tell a patient to sit on the chair with the forearm resting on a table. Next, hang the wrist and hand over the edge of the table. Hold the 2 or 3-pound dumbbell in the affected hand. After that, with a palm facing up, slowly lift a hand, so the back of the hand moves towards the floor. A patient’s forearm must remain on a table. Then, a clinician should give a command to move their hand in the upward direction as far as he/she can and then come back to the normal position. Do it ten times in a session. Do three sessions in a day. After 5 to 6 days, a physiotherapist must give a command to a patient to hold at the endpoint for ten seconds in one repetition. - Wrist supination with dumbbell
To perform the exercise, tell a patient to take the sitting position on the chair with a forearm resting on the table. Make sure that a wrist, as well as a hand, is over the edge of a table. After that, hold the end of the small 1- to 3-pound dumbbell in a hand, like a patient would hold the hammer. Then, slowly allow a hand as well as wrist to rotate over so the palm is facing up towards the ceiling, then slowly rotate the hand back up, therefore the dumbbell is straight up again. Do ten repetitions in one session, but without hold at the endpoint. Do three sessions in a day. After 5 to 6 days of the exercise, tell a patient to take hold at the endpoint for ten seconds per repetition. - Wrist pronation with dumbbell
To strengthen the wrist pronators, tell a patient to sit on the chair with the forearm supported on the table as well as the wrist and hand over the edge. Hold a dumbbell with the weight pointing up towards the roof. Next, slowly rotate the hand, so the wrist, as well as palm, are facing down towards the floor, then slowly turn the hand back to the starting position with the weight pointing up towards the ceiling. Do it ten times per session. Do three sessions in a day. - Rotation
Sit with the arms bent to 90 degrees and forearms out in front of a patient with palms facing down. Hold the light resistance band or even dumbbells, or go weight-free as well as pretend a patient is holding something. After that, slowly rotate the hands so the palms are facing up. Next, slowly rotate the palms back to the starting position. Repeat it ten times per session. Do around two sessions per day. - Wrist curl
To embark with, tell a patient to take the sitting position as well as hold the arm at 90 degrees, with a palm facing up. The arm may rest on the leg, a bench, or the table. Curl a wrist up. Return wrist to the starting position. Repeat ten times in a session. - Pronated wrist curl
To start with, to do this exercise, then a patient should sit as well as hold the arm at 90 degrees, with the palm facing down. Next, curl a wrist up. Return wrist to the beginning position. Repeat ten times per session. Do three sessions in a day. - Wrist ulnar deviators strengthening with dumbbell
To start this wrist strengthening exercise, the therapist tells a patient to sit in the chair with the forearm resting on a table. Next, give the command to a patient to put the hand in mid-range of supination as well as pronation over the edge of a table. Hold the 2 or 3-pound dumbbell in the affected hand. Next, with the palm facing a side, slowly move the hand down. A patient’s forearm must remain on the table. Then, a clinician should give a command to move a hand in the downward direction as far as he/she can and then come back to the starting position. Do it ten times in a session. Do three sessions in a day. After 5 to 6 days, a therapist must give a command to a patient to hold at the endpoint for ten seconds in one repetition. - Wrist extensors strengthen with the use of a theraband in supinated hand
First of all, ask a patient to take a comfortable position, such as sitting on a stable surface(chair or table) with the hand hanging on a rolled towel at the edge of the table, a palm should be facing the ceiling. After that, wrap the one end of the band on a patient’s hand, and the second end on a physical therapist’s strong hand. Tell a patient to move their hand in the downward direction agaist a theraband. Do it ten times in one session. Nearly three sessions would be done by a patient per day. - Supinators strengthen with the use of the band
To begin with, give a command to a patient to take a comfortable position, such as sitting on a stable surface(chair) with the hand neutral on a rolled towel at the edge of the table. After that, wrap the one end of a theraband in a patient’s hand, whilst the second end in a physical therapist’s strong hand. Give a command to a patient to rotate their hand against the theraband, a palm will face the ceiling. Then, do this strengthening exercise ten times per session. Around three sessions must be done by a patient per day. - Pronators strengthen with the use of the band
To embark with, the therapist tells a patient to take a comfortable position, namely sitting on the stable surface(chair) with the hand in the normal position as well as should be on a rolled towel at the edge of the table. Next, wrap the one end of the band in a patient’s hand, whereas the second end is in a clinician’s strong hand. Give a command to a patient to rotate their hand against the band, so the hand must be facing the floor. Do this strengthening exercise ten times in one session. Around three sessions would be done by a patient in a day. - Wrist ulnar deviators strengthening with theraband
To embark with, telling a patient to take a relaxed position means sitting on a chair with the hand in mid-pronation position at an edge of the table as well as hand should be put over a rolled towel. After that, wrap one end of the theraband in the patient’s hand, as well as the second end in the clinician’s hand. Ask a patient to move their hand in the downward direction agaist a theraband. Do it ten times in one session. Around three sessions should be done by a patient per day. After 5 days held at the end position for ten seconds in one repetition. Slowly return to the neutral position. When the patient is adapted to the light-weighted band after upgrading the color of the band for strengthening. - Wrist radial deviators strengthening with the theraband
To start with, tell a patient to take a comfortable position, such as sitting on a chair with the hand in a mid-supination position at the edge of the table as well as the hand should be placed over the rolled towel. Next, wrap the one end of the band on a patient’s hand, and the second end on a physical therapist’s hand. Ask a patient to move their hand in the upward direction agaist a theraband. Do it ten times in a session. Around two sessions would be done by a patient per day. After 5 to 6 days hold the position at the endpoint for ten seconds per repetition. Slowly come back to the neutral position. - Wrist extensors strengthen with the use of the theraband in pronated hand
To begin with, tell a patient to take a comfortable position, which means sitting on a stable surface(chair) with the hand hanging on a rolled pillow at the edge of the table, the palm should be facing the ground. After that, wrap the one end of the theraband on a patient’s hand, whereas the second end is on a clinician’s strong hand. Give a command to a patient to move their hand in the upward direction against the band. Next, do it ten times per session. Around three sessions would be done by a patient in one day. - Wrist flexors strengthen with the use of the theraband with a pronated hand
To start with, the therapist gives a command to a patient to take a comfortable position, such as sitting on a stable surface(chair or table) with the hand hanging on a rolled towel at the edge of a table, and the palm should be facing the floor. Wrap the one end of the theraband in a patient’s hand, while the second end is in a physical therapist’s strong hand. Tell a patient to move their hand in the downward direction against a theraband. Next, do this strengthening exercise ten times per session. Nearly three sessions should be done by a patient per day.
Surgical treatment of Intersection syndrome of the wrist
- On the occasion that conservative treatments fail surgery must be indicated to provide relief from symptoms. The minimal invasive tendon release operation may usually be done on an outpatient basis. A procedure starts the small incision over the intersection site to expose the involved muscles as well as tendons. Once the inflamed tendons are identified the surgeon carefully removes an irritated tenosynovium and releases the tendon sheath as well. The skin is then sutured together and the surgical dressing in place.
Home care
- Rest: Most individuals benefit from the use of the wrist brace to fully rest the tendons for at least five days. The optimal position of the splinted wrist joint is at about 15 degrees of extension. Activities that cause the aggravation of the symptoms must be avoided. Often changing techniques may assist to reduce the stress on the involved tendons.
- Ice: Ice must assist to relieve the symptoms of inflammation. The application of ice can be of significant benefit given the superficial location of the inflammation in people with intersection syndrome. Compared to other conditions that are deeper within the body as well as icing is of questionable benefit, this is the scenario where ice must have significant effects.






One Comment