Atlantoaxial Joint
Table of Contents
What is an atlantoaxial joint?
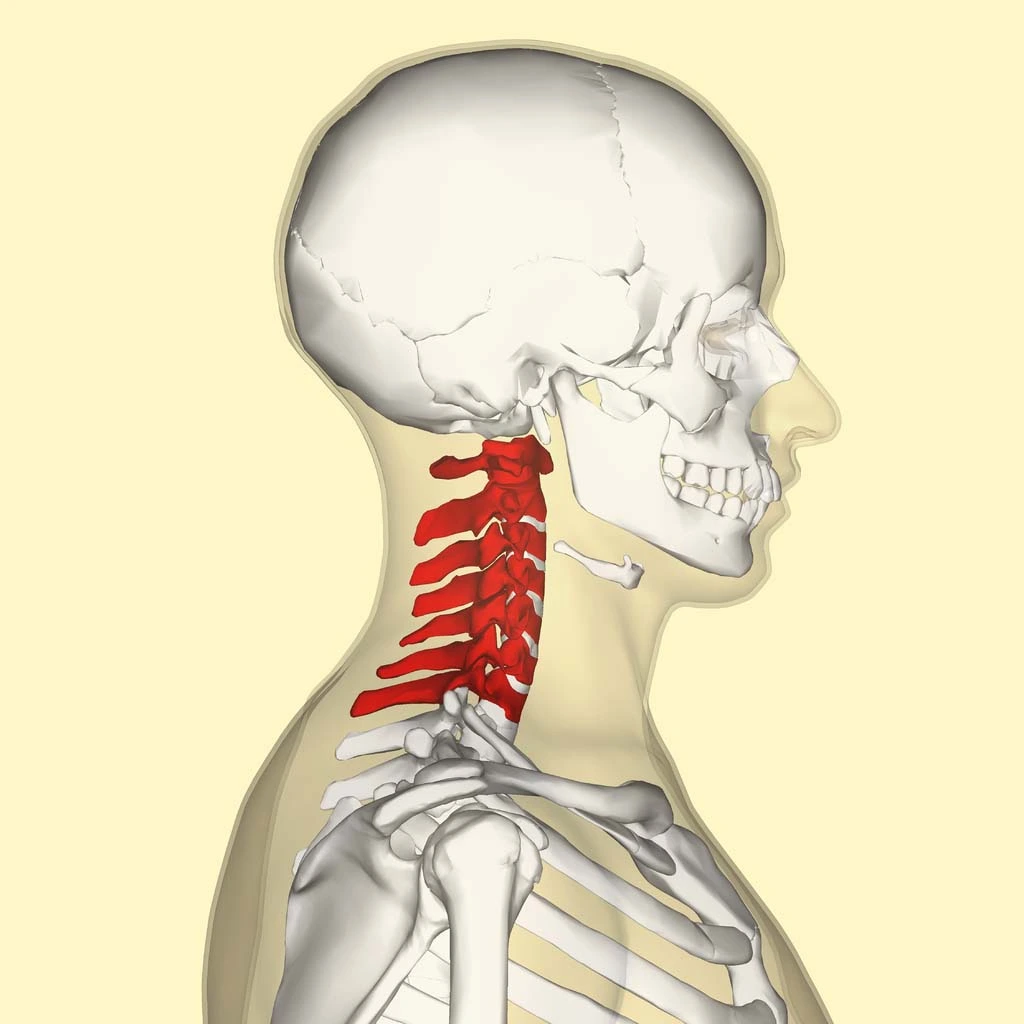
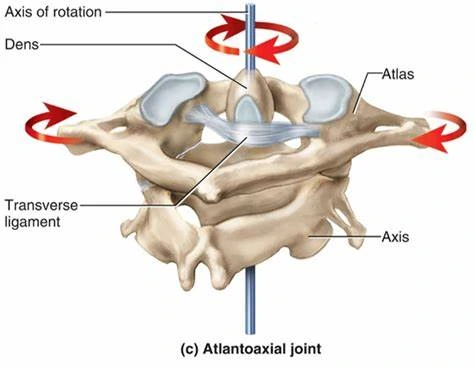
The atlantoaxial joint is a synovial type of joint that is categorized as a biaxial, pivot joint. The joint locates in the upper part of the neck between the 1st and 2nd cervical vertebrae. It is also known as the atlas and axis. The pivot joint classification indicates that it permits rotation only and is formed by a central pivoting, bony structure that rotates around craniovertebral ligaments.
Structure and Function of Atlantoaxial Joint
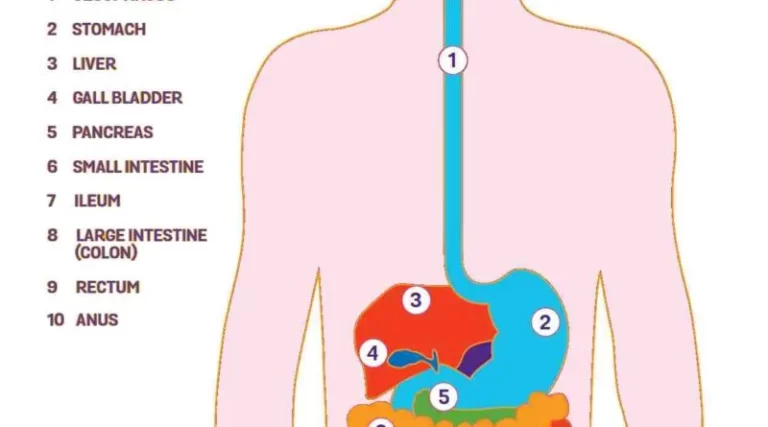
The atlantoaxial joint is a specific joint with multiple distinct structural parts donating to its crucial function for cervical stability & mobilization. It consists of 3 distinct, synovial joints: one medial joint & two lateral atlantoaxial joints. The median atlantoaxial joint’s structure is developed by the dens of C1 vertebrae & two ligamentous structures anteriorly & posteriorly.
These structures are the osteoligamentous rings of the atlas & the transverse ligament. The 2 bilateral atlantoaxial joints located laterally are classified as gliding joints. The upper-most regions of the cervical spine that make up the atlantoaxial joint are the atlas (C1) & the axis (C2). As they reside in the craniovertebral conjunction at the junction of the skull and the cervical spine, these two vertebrae are special among the rest of the cervical spine due to their distinct anatomical structure. This joint is special among the rest of the cervical spine due to its deficiency of an intervertebral disk.
The atlantoaxial joint is important in practical applications, permitting the rotate the head & turn to the right or left. Without the atlantoaxial joint, the kinematic capacity of the head & neck would not permit the nearly 600 moves/hour that we make as humans. In general, it stabilizes the head and helps the weight in a neutral position. This cervical unit also facilitated a defensive part of the spinal cord from external compression. It also permits blood supply to the brain via the passage of the vertebral artery. In addition to the protection and stabilization of the head, neck, and internal structures, the atlantoaxial joint also facilitates head and neck activities along with the neck muscles. This joint is also wrapped by an articular capsule, which performs to bind the margins of the atlas at the lateral masses with the posterior aspects of the axis.
Atlas (C1)
An atlas is a circular form that corresponds with the cranium above it with the zygapophyseal joints, and lateral masses. Below, the atlas articulates with the axis via its bilateral condyles. The atlas lacks a spinous procedure or vertebral body, which determines its structure from the rest of the cervical vertebrae. The atlas involves the transverse ligament between 2 superior articular facets, i.e. a posterior arch & an anterior arch, which works as a groove for the vertebral artery.
Axis (C2)
This vertebra is known as the C2 vertebra & carries a characteristic feature called the dens/ odontoid process. This structure is on the vertebrae’s anterior part and extends superiorly, articulating with the axis. Any other features of the axis are the bilateral transverse foramina, superior articular facets, & bifid spinous process.
Embryology
During pregnancy and the first two weeks that follow fertilization, many cellular divisions occur that cause blastocyst formation. At the end of the 2nd week, the blastocyte undergoes a process called gastrulation, which includes formation into a stratified structure composed of the ectoderm, mesoderm, & endoderm. In the formation of the cervical spine & atlantoaxial joint, mesodermal forms called somites start to migrate into their mature, functional form as vertebrae.
As the notochord involutes & somites develop into their mature forms as vertebrae at primary ossification centers. The normal effect of the cervical spine in embryogenesis involves the following steps: gastrulation & somatic mesodermal formation, ossification of the vertebrae, segmentation of somites, condensation of mesoderm into somites, dermomyotome & sclerotome reorganization, chondrification. The axis includes one ossification center for the vertebral body, 2 for both neural arches, and 1 for the dens.
These ossification compromises of the dens are particularly important since they can be confused as fractures in pediatric patients since the connection between the dens and the body of the axis does not complete fusion until about 6 years of age.
Blood Supply and Lymphatics
The vertebral arteries are by far the most significant in the contextual situation of the head & neck. This joint as an entirety receives blood collection from surrounding branches of the deep cervical, occipital, & vertebral arteries. About the atlantoaxial joint, the vertebral arteries leave the axis transverse foramen, then run slightly laterally to the transverse foramen of the atlas as they penetrate the cranium.
The collateral branches of the vertebral arteries provide the vertebral bodies of the cervical spine & the cervical radicular arteries. Surfacing from the subclavian arteries, the vertebral arteries cross the cephalad bilaterally: they join together to form a single structure called the basilar artery, which directly provides the brainstem.
Nerves
The innervation of this joint is the branch of the 2nd cervical spinal nerve. In general, each cervical vertebra has 2 nerve roots that originate from the spinal cord & extend out from both sides. The ventral part of the vertebrae includes the ventral root, & the dorsal segment of the vertebrae includes the dorsal root. As the nerve roots join together in the spinal foramen, they are termed spinal nerves. Although there are 7 cervical vertebrae, 8 pairs of spinal nerves exist. Generally, the spinal nerves exit above individually corresponding vertebrae. However, the C8 nerve root leaves below the C7 vertebrae.
Muscles
The movable part of the cervical spine is the atlantoaxial joint, & the primary stabilization are the 2 major surrounding & stabilizing ligaments:
- Transverse ligament
- Alar ligament.
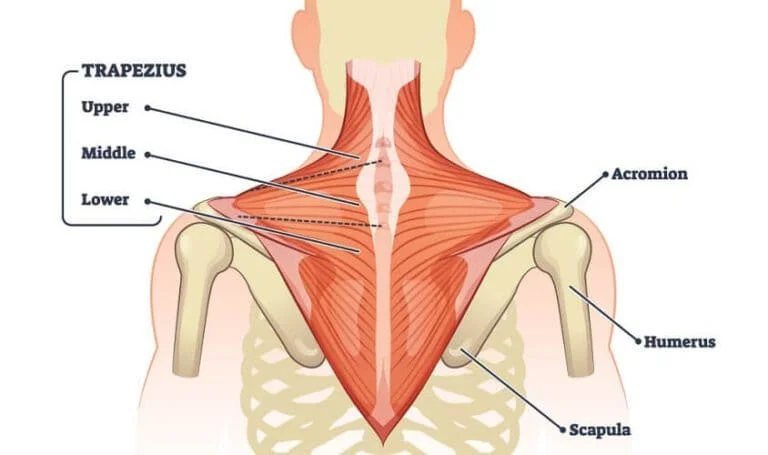
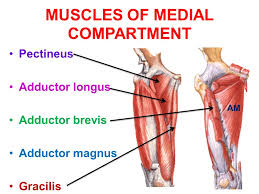
Considerable muscles in the posterior neck & suboccipital triangle accomplishment to stabilize the cervical vertebrae & joints as they enable rotatory, extension, flexion, and side-flexing. The suboccipital muscle group, which involves the posterior occipital triangle muscles, acts as attachments, & craniocervical motion initiators and postural stabilizers. They also include the posterior action of the occiput on C1. These 4 muscles involve the obliquus capitis superior & inferior and the rectus capitis posterior major & minor.
The craniovertebral ligaments that play an important role in the stability of the atlantoaxial joint are the following:
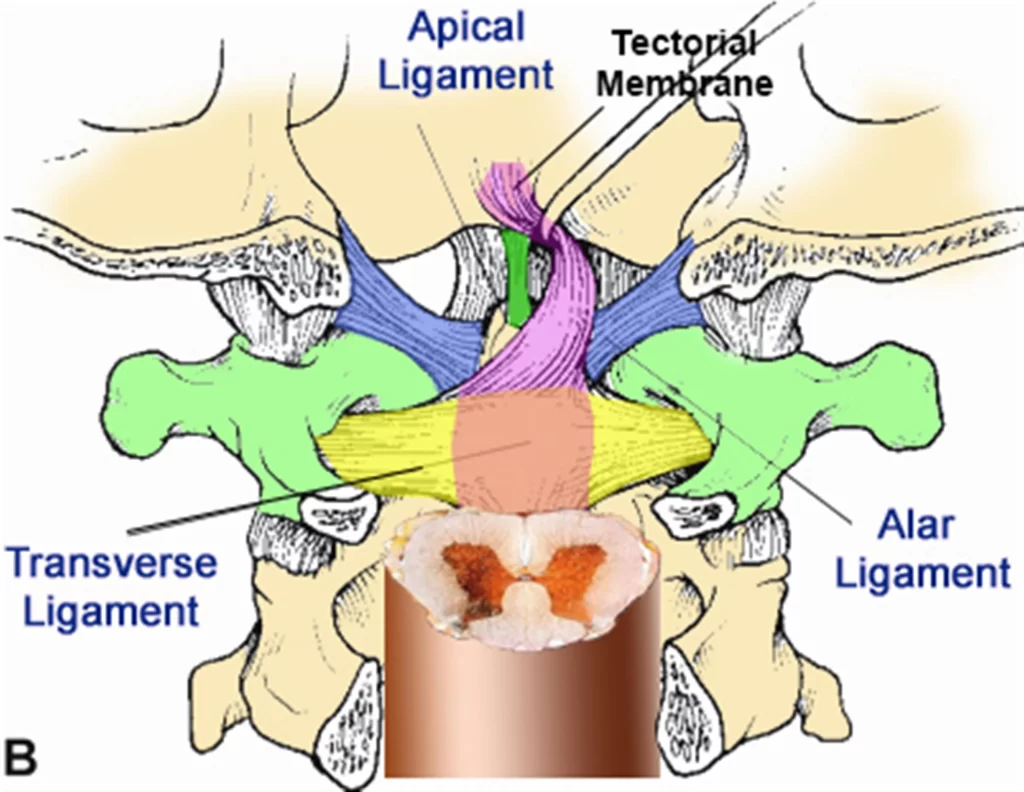
- Cruciform ligament (transverse ligament of the atlas)
- Tectorial membrane
- Alar ligaments
- Apical ligament of dens
Physiologic Variants
In general, in between cervical vertebrae, there fibs an intervertebral disc that is not present between C1 & C2 of the atlantoaxial joint. Further, a bifid spinous procedure is only consistently seen in C2 to C4. The literature accounts for approximately 0.3% of the population having a bifid spinous approach as low as C7. These are instances of normal physiologic variation. However, the odontoid process & even the transverse ligament can potentially undergo insufficient formation leading to an anatomical variant and potentially dangerous predisposition to instability & injury.
Os odontoideum – a controversial congenital or traumatic divagation of the dens where the superior margin of a hypoplastic den includes an ossific density. It is generally seen in the early evolution of the spine as in children and can be categorized as orthotopic/dystopic.
Persistent ossiculum terminal –this congenital malformation directs to the secondary ossification centers that fail to connect on the superior edge of the dens. This malformation is stable most of the time but it can be discovered incidentally. Ossification variation represents any arrest or partial interruption of bony ossification that may pose an obstacle to the anatomical structure & physiologic functional abilities of the atlantoaxial joint. These disorders can cause important cervical vertebrae abnormalities due to growth plate dysfunction.
Surgical Considerations
External Reduction Fixation
Surgical restoration of the odontoid process, or dens, fractures is usually an immediate necessity. Type I fractures are excessively rare & are generally stable, not requiring any surgical fixation. Type II fractures, however, are unstable & need stabilization either by external fixation and immobilization or internal fixation. Without stabilization, the a potential danger of nonunion with non-surgical intervention. There are specific nonunion risk aspects to consider before opting out of surgery. These involve but are not restricted to age greater than 50 years old at the time of injury, removal of the dens greater than 6 mm, & if moderate fracture comminution is present. It is shown that with an anterior process of fixation, there is a higher success ratio of surgical rehabilitation.
Halo Immobilization
This non-surgical procedure carries a lesser chance of nonunion if the patient is younger than 50 years of age at injury, has minimal dens removal, and has no comminution. This procedure can be achieved using a halo vest immobilizer (HVI), which works to provide extremely severe external support for the immobilization of the upper cervical spine, involving the atlantoaxial joint. It limits C1-C2 joint flexion by 75%.
Clinical Significance
Atlantoaxial Dislocation or Subluxation
Most of the time, atlantoaxial dislocation (AOD) occurs due to high-energy trauma such as motor vehicle accidents. These damages are affiliated with high mortality rates due to immediacy to the brainstem & potential vascular structures. There are 3 types of AOD, and all three are considered to all share the same mechanism of injury of severe hyperextension followed by lateral flexion. It is significant to note that the process for detecting an AOD on imaging is to look for the basion-dens distance. This is highly an atlantoaxial dissociation if greater than 10 mm.
Type I – Ventral Dislocation
- Most common
- Ventral dislocation of the occiput
Type II – Longitudinal Distraction
- Most unstable
Type II – Dorsal Dislocation
- Nontraumative Subluxation
Specific disease states have an increased incidence of atlantoaxial joint instability. This is mainly due to ligamentous laxity, which carries a higher chance for subluxation. Some of these situations involve, nasopharyngeal torticollis, also known as Grisel syndrome, spontaneous hyperemic dislocation, Morquio syndrome, and rheumatoid arthritis. Other genetic syndromes can lead to anatomical variants of the atlantoaxial joint, such as insufficient odontoid process formation or underdeveloped transverse ligament.
Traumatic Rotatory Subluxation
Age-related bony architecture plays an important role in tendencies for trauma. In geriatric populations, there is more prominent bony degeneration & decreased bone density, which also cause cartilaginous loss. This may account for a thinner joint space & predispose the patient to survive life-threatening harm if they sustain an atlantoaxial distraction or subluxation. Also, children tend to have a higher probability of having hypermobility in their joints & ligaments. Therefore, traumatic rotational subluxation due to hyperflexion & rotational forces may be seen more frequently in pediatric inhabitants.
Fractures of the Atlas with Successive Transverse Ligament Rupture
Jefferson fracture is the name provided to describe the atlas fracture. When the weakest part of the vertebral body is affected by severe axial loading, the anterior & posterior arches are generally affected. This type of fracture is usually seen when a patient has a record of diving headfirst into shallow water. Distinctive subtypes of the atlas due to high-intensity axial loading can be categorized into three subtypes:
- Posterior arch
- Burst
- Lateral mass injuries
Sometimes, the transverse & alar ligaments may be pulled without fracture to the atlas. These damages are best assessed by computed tomography & magnetic resonance imaging (MRI).
Dens Fractures
Type I – fracture of the odontoid tip at the alar ligament insertion site
Type II – a fracture at the base of the odontoid procedure
Type III – a fracture that expands into the axis body
Cervicogenic Headache
This is a subtype of chronic headache, which is likely a secondary headache originating from pathology in the upper cervical or the atlantooccipital joint. With ipsilateral, pericranial muscle pain existing as the major symptom of a cervicogenic headache, the C1-C3 nerve roots are considered to be a nociceptive origin for guided pain up to the occiput. It is necessary to distinguish a cervicogenic headache from other headache subtypes & more ominous pathology such as intracranial pathology, cervical artery dysfunction, & cervical myelopathy.
Occipital Neuralgia
The posterior cervical plexus, also known as Cruveilhier’s plexus, can be trapped by a collection of muscle fibers. As the nerve fibers from the posterior rami of C1-C3 exit, hypertonic suboccipital muscles & even the superficial muscles such as the trapezius & splenius capitis can compress & ensnare the surrounding nerve structures. Hypertonic muscles can subsequently inhibit the functions of the nerve fibers conducting to inflammation, injury, & severe piercing or throbbing-like sensations in the upper heck & occiput. This situation is known as occipital neuralgia.
FAQ
The median atlantoaxial joint is developed between the dens of the axis and an osteoligamentous ring of the atlas anteriorly & transverse ligament posteriorly. It is categorized as a pivot joint. The lateral atlantoaxial joints are bilateral joints developed between the lateral masses of the atlas & axis.
In addition to the primary ligaments, there are many accessory ligaments of the median atlantoaxial joint that attach the axis (C2) with the occipital bone. The tectorial membrane of the cervical vertebral column defines the superior continuation of the posterior longitudinal ligament.
The joint between the upper spine & the base of the skull is called the atlantoaxial joint. In individuals with Down syndrome, the ligaments that connect between muscles are “lax” or floppy. This can result in AAI where the bones are less stable & can harm the spinal cord.
Repetition radiographs (x-rays) will usually be repeated in 4 & 8 weeks to assess the restoration and recovery. The prognosis for atlantoaxial instability relies on the degree of spinal cord trauma & neurological deficits already present.
This joint is stabilized by a promontory of the axis named the dens, which fits into the atlas, and considerable ligaments between the 2 bones. There are two reasons for the instability, trauma & birth abnormalities. Traumatic instability happens after forceful flexion of the head.
Parents should watch their child for any dissimilarities in how they walk, use their hands, use their arms, how they tilt the head, complaints of pain in the neck, change in bowel or bladder function, change in known function, or new-onset weakness.
The best reason to determine them is generally that atlantoaxial instability patients can minister with a less interfering C1-C2 screw fixation while CCI patients may require more comprehensive surgery.
The lateral atlantodental interval is the horizontal space between the lateral cortex of the dens & the medial cortex of the lateral masses of the atlas. The normal value is 3.4 mm in either the right or left atlantodental interval. However, a normal asymmetry between the right & left atlantodental interval can differ up to 0.76 mm.