Arthritis of knee
Table of Contents
What is arthritis of the knee?
Knee arthritis is inflammation & deterioration of knee joint cartilage. Cartilage is the slippery coating at the ends of bones that serves as a cushion & allows the knee to smoothly bend and straighten. Knee cartilage coats the end of the thighbone (femur), the top of the shinbone (tibia), & the backside of the kneecap (patella). When the cartilage wears away, the space between the bones decreases. In advanced arthritis, bone rubs on bone, & bone spurs might form.
Pain, swelling, & stiffness are the primary symptoms of arthritis. Any joint in the body might be affected by the disease, but it is particularly common in the knee.
Knee arthritis can make it difficult to do many daily activities, such as walking or climbing stairs. It is a major cause of lost work time and a serious disability for many patients.
The most usual types of arthritis are osteoarthritis & rheumatoid arthritis, but there are more than 100 different forms. While arthritis is mainly an adult condition, some types affect children also.
Everyone’s joints go through a normal cycle of damage & repair during their lifetime, but sometimes the body’s process to repair our joints can cause changes in their shape or structure. When these changes happen in one or more of the joints, it’s known as osteoarthritis.
Damage to the joint cartilage over time might result in the development or worsening of deformities of the knee, including knock knees & bowleg.
Cartilage loss can occur between the thighbone & the shinbone in the medial portion (inner side), lateral portion (outer side), & under the kneecap.
Thinning of the cartilage under the kneecap is called patellofemoral arthritis (kneecap arthritis). Some patients have cartilage loss in one, two, or all of these sites. When all three sites are affected, this is called tricompartmental arthritis.
Osteoarthritis can affect anyone at any age, but it’s more usual in women over 50.
Injuries or other joint complications, such as gout, can make people more likely to get osteoarthritis. The genes someone inherits from their parents can also increase the risk of the disease developing.
Being overweight is also linked to osteoarthritis, as this leads to extra strain on weight-bearing joints, such as knees.
Although there is no cure for arthritis, there are many treatment options available to help manage pain & keep patients staying active.
What is the anatomy of the knee?
The knee is the most strong & large joint in the body. It is made up of the lower end of the femur, the upper end of the tibia (shinbone), & the patella (kneecap). The ends of the three bones that form the knee joint are covered with articular cartilage, a smooth, slippery substance that protects & cushions the bones as you bend and straighten the knee.
2 wedge-shaped pieces of cartilage called meniscus act as “shock absorbers” between the thighbone & the shinbone. They are tough & rubbery to help cushion the joint & keep it stable.
The knee joint is surrounded by a thin lining known as the synovial membrane. This membrane releases a fluid that lubricates the cartilage & decreases friction.
Three bones get combined to make the knee joint. They include the
- Thighbone (femur).
- Shinbone (tibia).
- Kneecap (patella).
A smooth substance called cartilage covers the ends of every bone. It’s a cushion between the bones that keeps them from rubbing each other. The synovial membrane is a type of tissue that surrounds the joint and lubricates the cartilage.
What are the causes of arthritis of the knee?
Osteoarthritis takes place when the cartilage that cushions the ends of bones in the joints gradually deteriorates. Cartilage is a firm, slippery tissue-like structure that enables nearly frictionless joint movement.
Eventually, if the cartilage wears down completely, the bone will rub against the bone.
Osteoarthritis has frequently been referred to as a wear & tear condition. But besides the damage to cartilage, osteoarthritis affects the whole joint. It causes changes in the bone & deterioration of the connective tissues that hold the joint together & attach muscle to bone. That leads to inflammation of the joint lining.
Experts have identified some genes that may cause arthritis, including arthritis of the knee. Experts predict that there are more genes not yet discovered. Patients could have a gene linked to arthritis without knowing it & a virus or injury could trigger arthritis of the knee.
Though the cause is unknown, some risk factors elevate the possibility of arthritis of the knee.
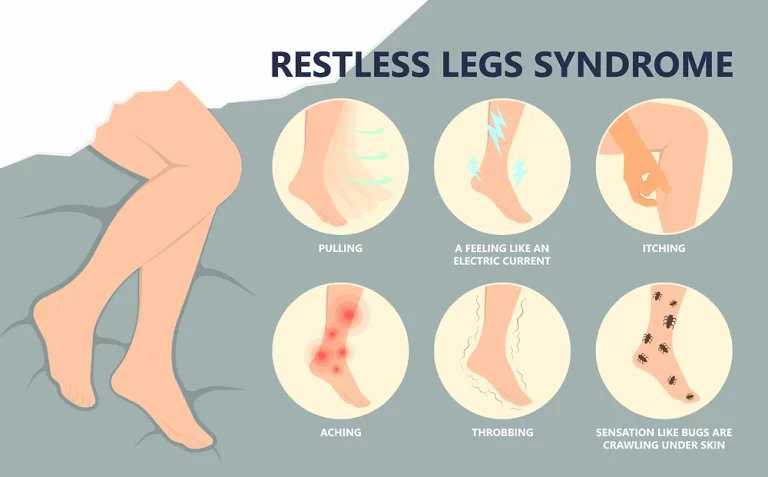
What are the symptoms of arthritis of the knee?
Gradual increase in pain, arthritis pain generally starts slowly, although it can appear suddenly in some cases.
At first, you might notice pain in the morning or after you’ve been inactive for a while. Your knees might hurt when you:
- climb stairs
- stand up from a sitting position
- walk on a flat surface
- sit down for a while
- Knee pain that wakes you up from sleep can be a feature of OA.
For patients with Rheumatoid arthritis, the symptoms frequently start in the smaller joints. They are also more prone to be symmetrical, affecting both sides of the body. The joint might be warm & red.
With osteoarthritis, symptoms might progress rapidly or they might develop over several years, depending on the individual. Symptoms can worsen & then remain stable for a long time, and they can vary from day to day.
Factors that might cause worsening of symptoms include:
- cold weather
- stress
- excessive activity
With Rheumatoid arthritis, symptoms usually seem over several weeks, but they can develop or worsen in a few days. A flare can happen when condition activity increases. Triggers vary & can involve changes in medication.
- Swelling or tenderness
- Arthritis of the knee can occasionally cause inflammation.
With osteoarthritis, this can be:
hard swelling, because of the formation of bone spurs (osteophytes)
soft swelling, as inflammation leads extra fluid to collect around the joint
Swelling might be more noticeable after a long period of inactivity, like when you first wake up in the morning.
Joint swelling is usual with Rheumatoid arthritis, as it’s an inflammatory disease.
People with Rheumatoid arthritis might also have other symptoms, such as fever, tiredness, and a general feeling of being unwell, Other body organs that can be affected by inflammatory changes involve the eyes, heart, and lungs.
This is because Rheumatoid arthritis is a systemic disease, which means it affects the whole body. osteoarthritis, meanwhile, only has a straight impact on the affected joint.
Buckling & locking-
Over time, damage to the joint can cause the knee parts to become unstable. This can lead to it giving way or buckling.
Rheumatoid arthritis can cause damage to the tendons, which join the muscles to the bones. This damage can lead to the knee’s instability.
Bone spurs can also develop as the cartilage erodes & the bones rub together. These make a bumpy surface that can cause the joint to stick or lock up, making it hard to bend or straighten out.
Cracking or popping sounds-
When you bend or straighten your knee, you might feel a grinding sensation or hear cracking or popping sounds. Doctors call this crepitus.
These symptoms can occur when patients have lost some of the cartilage that helps with a smooth range of motion. Both conditions OA & Rheumatoid arthritis can result in cartilage damage.
When cartilage is damaged, rough surfaces & bone spurs develop. As the patient moves her joints, these irregular areas rub against each other.
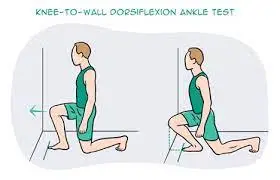
Poor range of motion-
The bone & cartilage changes that occur with osteoarthritis of the knee or after a knee injury can make it hard for your knee joints to move smoothly. It can become hard to move the knee to walk, stand up, & carry out other everyday movements.
People with Rheumatoid arthritis might find it hard to bend & flex their knee or to walk, due to pain & swelling. Damage to the knee joint can also affect mobility. In time, you might need a cane or walker to help you stay balanced and mobile.
Loss of joint space-Some of the effects on the knee is not obvious. Diagnostic tools, such as a knee X-ray, can help find internal damage.
Cartilage usually occupies a space around the bones, where it cushions the joint. An X-ray image of the knees can find the results of cartilage damage
Deformities of the knee-
The appearance of the knee can change during a flare & as damage progresses.
In Rheumatoid arthritis, swelling & redness are common during a flare. In the long term, persistent inflammation can result in permanent damage to the cartilage & the tendons. This can affect the shape & appearance of the knee joint.
With osteoarthritis, the muscles around the knee can weaken, resulting in a sunken appearance. The knees can starts pointing toward each other or bending outward.
Knee deformities range from hardly noticeable to severe & debilitating.

What are the stages of arthritis of the knee?
There are five stages of osteoarthritis, the most common type of arthritis that affects the knees:
- Stage 0 (Normal). If you’re at stage 0, the knees are healthy. The patient doesn’t have arthritis in the knee.
- Stage 1 (Minor). Stage 1 means that the patient has got some wear and tear in the knee joint. You probably won’t notice pain.
- Stage 2 (Mild). The mild stage is when a patient might start to feel pain and stiffness, but there’s still enough cartilage to keep the bones from actually touching.
- Stage 3 (Moderate). If the patient is at the moderate stage, they’ll have more pain, especially when running, walking, squatting, & kneeling. they’ll likely notice it after long periods of rest (like first thing in the morning). You’re probably in a great deal of pain because the cartilage has narrowed even further & there are many bone spurs.
- Stage 4 (Severe). Severe osteoarthritis means that the cartilage is almost gone away. the knee is stiff, painful, & possibly immobile. The patient might need surgery.
What are the types of arthritis of the knee?
Osteoarthritis
Osteoarthritis is indicated by cartilage degeneration & bony protrusions called osteophytes. In the knee, the most common areas of osteoarthritis include the tibia (shin bone), femur (thigh bone), & patella (kneecap).
The most usual type of arthritis affecting the knee is osteoarthritis. Osteoarthritis occurs when joint articular cartilage breaks down. In the knee, articular cartilage covers the top of the tibia (shin bone), the bottom of the femur (thigh bone), and the back of the patella (knee cap).
Not everyone with knee osteoarthritis will have knee pain. Pain might occur if the loss of healthy cartilage:
This causes the bones of the joint to rub against one another.
Compromises the joint’s biomechanics in some way.
It is a degenerative, “wear-and-tear” type of arthritis that occurs most frequently in patients 50 years of age & older, although it might occur in younger people, too.
In the early stages of knee osteoarthritis, the pain might be felt when doing specific activities, such as jogging. As osteoarthritis progresses, the pain might be felt during daily activities.
Post-traumatic knee arthritis
Post-traumatic arthritis is a type of osteoarthritis. It occurs after a meniscus tear, ligament injury, or other trauma. The injury might heal but wear and tear on the articular cartilage can accelerate. Post-traumatic arthritis might not become symptomatic until years after the injury.
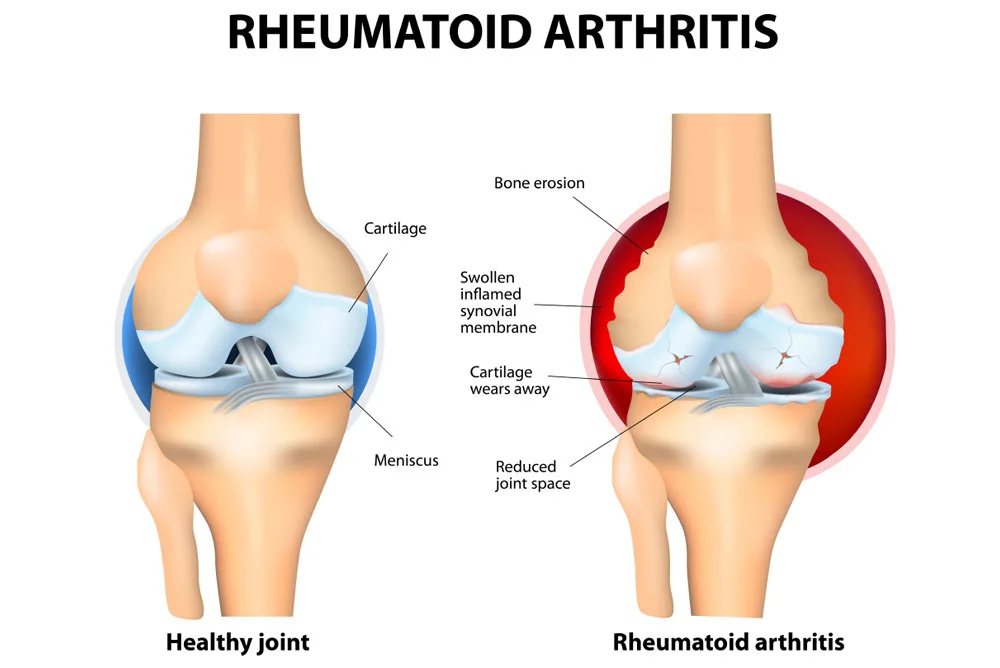
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune condition that targets the synovial membrane surrounding many joints of the body. Some of the most common areas affected involve the wrists, knees, & ankles.
Knee pain can be caused by an autoimmune condition called rheumatoid arthritis. Rheumatoid arthritis causes joint inflammation that can be made the knee feel swollen, stiff, warm, & painful. Over time, untreated Rheumatoid arthritis can cause permanent knee joint damage.
Rheumatoid arthritis frequently affects joints symmetrically, so if one knee is affected the other is also prone to be affected. Symptoms are also usual in the hands & wrists. Episodes of Rheumatoid arthritis might come and go and can be accompanied by other symptoms, such as fatigue.
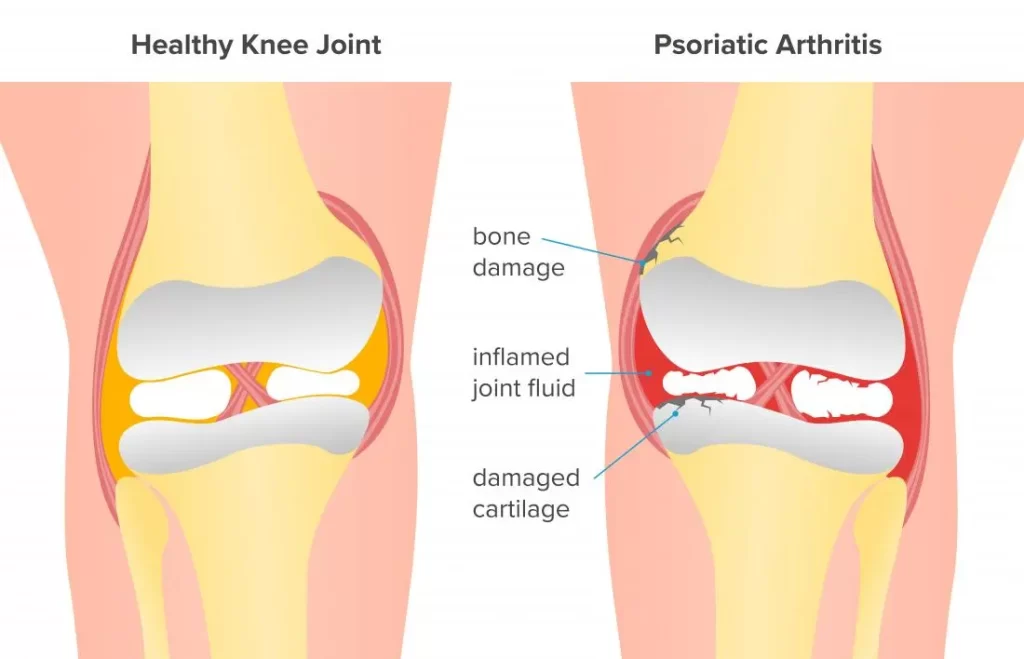
Psoriatic arthritis is an autoimmune disease associated with psoriasis, a skin disease. Psoriasis frequently appears as an itchy red spot on the elbows, knees, or scalp; & psoriatic arthritis can manifest in the joints of the extremities, hips, knees, & spine.
As Rheumatoid arthritis, psoriatic arthritis is also an autoimmune disease. When the knee is affected by psoriatic arthritis, the knee might feel painful, stiff, swollen, & tender. Other joints are frequently affected, particularly joints in the fingers & toes. Other common symptoms involve fatigue & eye pain.
Psoriasis is a skin condition. While estimates vary, recent research suggests about 20% of patients with psoriasis also have psoriatic arthritis. Many patients have had psoriasis for years before experiencing joint pain related to psoriatic arthritis.
Gout is an inflammatory arthritis condition that can cause a build-up of uric acid crystals in the knee joint. These needle-like, microscopic crystals collect in the soft tissue of the knee joint and lead to pain that can be excruciating, as well as swelling, redness, & warmth.
About half of all gout cases affect the big toe joint, but other cases affect the knee or another joint.
Pseudogout: Calcium Pyrophosphate Deposition (CPPD)
Pseudogout is a type of inflammatory arthritis that comes from the buildup of calcium pyrophosphate crystals in the joints of the body. While less usual than gout, pseudogout is more likely to affect the knee.
Like gout, pseudogout is caused by a build-up of microscopic crystals in a joint & can lead to sudden, severe knee pain, swelling, warmth, & redness. Pseudogout is less usual than gout but more likely to affect the knee joint.
The microscopic crystals that cause pseudogout are known as calcium pyrophosphate crystals. Doctors frequently refer to pseudogout as calcium pyrophosphate deposition (CPPD).
Reactive arthritis can result in inflammatory joint pain, most usually in the knee, fingers, or low back. Other possible features include problems involving the urinary tract, skin, & eyes.
Reactive arthritis usually affects the knee, though it can affect any joint in the body. Arthritis inflammation can lead to a knee being achy, swollen, & red.
Reactive arthritis happens as a reaction to an infection, such as a stomach bug or a sexually transmitted disease (STD). Days, weeks, or even months after the infection has resolved, a person might develop pain in one or more joints, inflamed eyes, & other symptoms.
The above conditions are usual causes of arthritic knee pain. There are more than 100 types of arthritis that might include knee symptoms. Patient with chronic knee pain is advised to consult with their doctors for an accurate diagnosis.
What are the risk factors for arthritis of the knee?
- Age. Osteoarthritis is a degenerative, “wear & tear” disease. The older patients are, the more likely they are to have worn-down knee joint cartilage.
- Heredity. Slight joint defects or double-jointedness (laxity) & genetic defects might contribute to osteoarthritis in the knee.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, & the more you weigh, the greater patient’s risk. Increased weight adds stress to weight-bearing joints, such as hips & knees. Also, fat tissue produces proteins that can cause harmful inflammation in & around the joints.
- Injury. Severe injury or repeated injury to the knee can cause osteoarthritis years later.
- Overuse. Jobs & sports that require physically repetitive motions that place stress on the knee can increase the risk of developing osteoarthritis.
- Gout. Gout, also a type of inflammatory arthritis, might cause osteoarthritis.
- Gender. Postmenopausal women are more prone to osteoarthritis than men.
- Autoimmune triggers. While the cause of rheumatoid arthritis remains unknown, the triggers of autoimmune diseases are still an area of active investigation.
- Developmental abnormalities. Deformities such as knocked knee & bowleg place higher than normal stress on certain parts of the knee joint and can wear away the cartilage in those areas.
- Other health conditions. Patients with diabetes, high cholesterol, hemochromatosis (high levels of iron in the blood), & vitamin D deficiency are more likely to have osteoarthritis.
What are the complications of arthritis of the knee?
Osteoarthritis is a degenerative condition that worsens over time, frequently resulting in chronic pain. Joint pain & stiffness can become severe enough to make daily tasks difficult.
Depression & sleep disturbances can come from the pain & disability of osteoarthritis.
Osteoarthritis can develop over just a year or two, but more frequently it’s a slow process over many years that only causes fairly small changes in just part of the knee.
But in some cases, the cartilage can become so narrow that it no longer covers the ends of the bones. This causes them to rub against each other & eventually wear away.
The loss of cartilage, the wearing of the bones, & the bony spurs can change the shape of the joint. This forces the bones out of their normal positions, making the knee feel unstable & painful.
Some patients with osteoarthritis find a lump that seems at the back of their knee. This is known as Baker’s cyst or popliteal cyst.
A Baker’s cyst is fluid-filled swelling at the back of the knee that occurs when part of the joint lining bulges through a small tear in the joint capsule. This can then lead joint fluid to be trapped in the bulge.
It can happen on its own but is more prone in a knee that’s already affected by arthritis. A Baker’s cyst doesn’t always cause pain, but sometimes it can burst so the fluid leaks down into your calf, causing sharp pain, swelling, & redness in the calf.
Osteoarthritis in the knee may change the way a patient walks or carry their weight, and this could cause them to develop the condition in other joints, such as their hips.
What is the diagnostic procedure for arthritis of the knee?
During an appointment, the doctor will talk with the patient about symptoms & medical history, conduct a physical examination, & possibly order diagnostic tests, such as x-rays or blood tests.
What questions might a healthcare give ask to diagnose arthritis of the knee?
the healthcare provider will interview the patient when the patient report symptoms. Some questions may include:
- Does anyone in the family have arthritis of the knee?
- Does the knee swell up?
- Is the skin often red?
- Is the skin often warm?
- Do patients have symptoms in one knee or both?
- How long has the patient had these symptoms?
- What medications does the patient take?
- How severe is the patient’s pain?
- Do patients struggle to walk?
- Do the symptoms interfere with daily activities?
The healthcare provider will probably order X-rays of the patient’s knees to check for arthritis. The X-rays should reveal:
- The type of arthritis.
- Any changes in the bones.
- Bone spurs.
- How narrow the space is between the bones. The less cartilage, the narrower the space. The lesser the space, the greater the pain.
Magnetic resonance imaging (MRI). An MRI uses radio waves & a strong magnetic field to produce detailed images of bone & soft tissues, including cartilage. An MRI isn’t commonly required to diagnose osteoarthritis but can help provide more information in complex cases.
computerized tomography (CT) scan might be required to determine the condition of the bone & soft tissues of the knee.
Laboratory Tests
the doctor might also recommend blood tests to determine which type of arthritis patients have. With some types of arthritis, including rheumatoid arthritis, blood tests will be used for a proper diagnosis.
Joint aspiration: drawing out & testing the synovial fluid inside the knee joint
Cartilage cannot be seen on X-ray, but the narrowing of the joint space between the bones indicates lost cartilage. X-rays show bone spurs & cysts, which can be led by osteoarthritis.
What is the treatment plan for arthritis of the knee?
Being overweight elevates the strain on the joints, especially the knees. It makes it more likely that the patient will develop
osteoarthritis & arthritis will get worse over time.
Losing weight if patients are overweight could reduce pain & other symptoms of osteoarthritis of the knee. The force put
through the knees when you walk, run or go up & down stairs can be two or three times your body weight, so losing even a
a little amount of weight can make a big difference to the strain on the knees.
There’s no special diet that will help with osteoarthritis, but if the patient needs to lose some weight they should follow a balanced, reduced-calorie diet combined with regular exercise. the doctor should be able to give the patient advice on diets & exercise that will help.
- Reducing the strain on the knees
- Apart from keeping an eye on weight, there are a number of other ways patients can decrease the strain on the knees.
- Pace patient activities – don’t tackle all your physical jobs at once. Break the harder jobs up into chunks & do anything gentler
- in between. Keep using the knee even if it’s slightly uncomfortable, but rest it before it becomes too painful.
- Wear shoes with thick soles & enough room for toes. Wearing the right shoes can reduce the shock through the knees
- as you walk & prevent any changes to the feet.
- If you require extra support for feet or knees when you walk, speak to your physiotherapist, occupational therapist, or doctor
- about getting insoles made for patients’ shoes.
- Use a walking stick if required to reduce the weight & stress on a painful knee. An occupational therapist can recommend on the
- correct length & the best way to use the stick.
- Use a handrail for support when going up or down the stairs. Go upstairs one at a time with the patient’s good leg first.
- Think about making changes to your home, car, or workplace to decrease unnecessary strain. An occupational therapist can advise
- patient on special equipment that will make things they do every day easier.
- Using a heat pack or something same on a painful knee may help to relieve the pain & stiffness of osteoarthritis. An ice pack can also help but be careful not to put ice or heat packs or hot water bottles directly on the skin wrap them with a tea towel or cover.
Some patients find that knee braces help. Patients can buy knee braces from sports shops & chemists, but they should speak to a doctor or physiotherapist first, as they might be able to provide braces or recommend the best one for them.
Coping with low mood & sleep problems. The patient might find that osteoarthritis of the knee makes him feel depressed or anxious. Speak to a doctor if you’re feeling low as they might be able to recommend psychological therapies to help you, such as cognitive behavioral therapy (CBT) & stress-relieving techniques.
If a patient’s sleep is disturbed because of osteoarthritis of the knee, this could make the pain feel worse. nevertheless, there are things the patient can do for themselves that might help, such as:
- Keep a sleep diary to work out if there are any patterns to sleep problems
- Sleep at regular times to get the body into a routine
- Avoid phones & other screens in the bedroom to help you wind down before bed.
- If the patient is still having problems, speak to a doctor or an occupational therapist who can give you other tips & techniques to try, known as sleep hygiene.
Other remedies. Applying heat or ice, or wearing elastic bandages to give support to the knee might provide some relief from pain.
Medical treatment for arthritis of the knee:
Medications. Several types of drugs are useful in managing arthritis of the knee. Because patients respond differently to medications, the doctor will work closely with the patient to determine the medications & dosages that are safe & effective for you.
Over-the-counter, non-narcotic pain relievers & anti-inflammatory medicines are usually the first choices of therapy for arthritis of the knee. Acetaminophen is a simple, over-the-counter pain reliever that can be effective in decreasing arthritis pain.
Like all medications, over-the-counter pain relievers can cause side effects & interact with other medications patients are taking. Be sure to discuss potential side effects with the doctor.
Another kind of pain reliever is a nonsteroidal anti-inflammatory drug, or NSAID (pronounced “en-said”). NSAIDs, such as ibuprofen & naproxen, are available both over the counter & by prescription & in oral and topical (gel) forms. Oral NSAIDs are recommended to improve pain & function in people with knee osteoarthritis. Topical NSAIDs can help improve function & quality of life for patients with knee osteoarthritis. Nevertheless, NSAIDs should be used with caution, or avoided, in patients with certain health conditions, such as coronary artery disease, congestive heart failure, & chronic kidney disease. Talk to a doctor about whether NSAIDs are right for you.
A COX-2 inhibitor is a special type of NSAID that might cause fewer gastrointestinal side effects. Common brand names of COX-2 inhibitors involve Celebrex (celecoxib) & Mobic (meloxicam, which is a partial COX-2 inhibitor). A COX-2 inhibitor decreases pain & inflammation so that you can function better. If patients are taking a COX-2 inhibitor, the patient should not use a traditional NSAID (prescription or over-the-counter). Be sure to tell the doctor if you have had a heart attack, stroke, angina, blood clot, or hypertension, or if patients are sensitive to aspirin, sulfa drugs, or other NSAIDs.
Corticosteroids are powerful anti-inflammatory drugs that can be injected directly into the joint. These injections give pain relief & reduce inflammation; nevertheless, the effects do not last indefinitely. the doctor might recommend limiting the number of injections to three or four per year, per joint, because of possible side effects. In some cases, pain & swelling might “flare” immediately after the injection, & the potential exists for long-term joint damage or infection. With often repeated injections or injections over an extended period of time, joint damage can actually increase rather than decrease.
Disease-modifying anti-rheumatic drugs (DMARDs) are utilized to slow the progression of rheumatoid arthritis. Drugs like methotrexate, sulfasalazine, & hydroxychloroquine are commonly prescribed. In addition, biological DMARDs like etanercept (Enbrel) & adalimumab (Humira) might decrease the body’s overactive immune response. Because there are many different drugs today for rheumatoid arthritis, a rheumatology specialist is frequently required to effectively manage medications.
Glucosamine & chondroitin sulfate, substances found naturally in joint cartilage, can be taken as dietary supplements. Although patient reports indicate that these supplements might relieve pain, there is no evidence to support the use of glucosamine & chondroitin sulfate to decrease or reverse the progression of arthritis. In addition, the U.S. Food & Drug Administration does not test dietary supplements before they are sold to consumers. These
compounds might cause side effects, as well as negative interactions with other medications. Always consult a doctor before
taking dietary supplements.
Surgical treatment for arthritis of the knee:
the doctor might recommend surgery if the patient’s pain from arthritis causes disability & is not relieved with nonsurgical treatment. As with all surgeries, there are some risks & possible complications with different knee processes. the doctor will discuss the possible complications with the patient before your operation.
Arthroscopy. During arthroscopy, doctors use small incisions & thin instruments to diagnose & treat joint problems.
Arthroscopic surgery is not frequently utilized to treat arthritis of the knee. In cases where osteoarthritis is accompanied by a degenerative meniscal tear, arthroscopic surgery might be recommended to treat the torn meniscus.
Cartilage grafting. Normal, healthy cartilage tissue might be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small sites of cartilage damage.
Synovectomy. The joint lining damaged by rheumatoid arthritis is removed to decrease pain & swelling.
Osteotomy. In a knee osteotomy, either the tibia (shinbone) or femur (thighbone) is cut & then reshaped to relieve pressure on the knee joint. Knee osteotomy is utilized when patients have early-stage osteoarthritis that has damaged just one side of the knee joint. By shifting the patient’s weight off the damaged side of the joint, an osteotomy can relieve pain & significantly improve function in the arthritic knee.
Total or partial knee replacement (arthroplasty). the doctor will remove the damaged cartilage & bone, & then position new metal or plastic joint surfaces to restore the function of the knee.
The most usual type of surgery for osteoarthritis of the knee is a knee replacement. Many knee replacements are performed each year, & the operation can give a lot of pain relief & improve movement in the knee.
Surgical techniques are improving all the time & research has shown that up to 8 in 10 knee replacements could last as long as 25 years. Nevertheless, as with all surgery, there are some risks & your surgeon will want to make sure you’re in the best health possible before the operation.
Sometimes keyhole surgery techniques might be used to wash out loose fragments of bone & other tissue from the knee. This is called arthroscopic lavage or debridement, but it won’t be recommended for patients unless the knee locks.
Recovery
After any kind of surgery for arthritis of the knee, there is a period of recovery. Recovery time & rehabilitation depends on the type of surgery performed.
the doctor might recommend physical therapy to help you regain strength in the knee & to restore your range of motion. Depending upon your procedure, a patient might need to wear a knee brace or use crutches or a cane for a time.
In most cases, surgery relieves pain &makes it possible to perform daily activities more easily.
To assist doctors in the nonsurgical management of knee osteoarthritis, the American Academy of Orthopaedic Surgeons has conducted research to give some useful guidelines. These are recommendations only & might not apply to every case.
Physiotherapy treatment for arthritis of the knee:
Physiotherapy should be started with all patients with a diagnosis of knee arthritis.
Pain is a common symptom that occurs at different intensities depending on the individual, it is not necessarily related to the severity of arthritis progression.
Exercise has been proven to be effective in pain management & also improves physical functioning in the short term. Exercises have to take place under the supervision of a physiotherapist initially & when properly instructed these exercises can be performed at home, though research has shown that group exercise combined with home exercise is more beneficial.
Role of Physiotherapy:
- Education
- Understanding what arthritis is
- Explaining pain
- Explain the long-term management of arthritis
- Educate regarding activity modification
- Role of weight loss
- Promote an active, healthy lifestyle
- Exercise
- Reduces knee pain & inflammation.
- Normalises knee joint range of motion.
- Strengthens lower kinetic chain
- Reduces risk of cardiovascular disease
- Improves proprioception, agility, & balance.
- Promotes physical function
Land-based exercises are ideal for most patients & are strongly recommended. Aquatic exercise, stationary cycling, & walking are safe & effective activities that do not cause undue stress on the knee joint.
Exercise has also been found to be beneficial for other co-morbidities & overall health. Walking, resistance training, cycling, yoga, & Tai Chi are examples of such exercises. An individualized exercise program should be set by a physiotherapist initially, taking into account the patient’s goals & hobbies to ensure long-term exercise compliance.
Range of movement exercises
These are good for posture & help to keep joints flexible. These exercises can be something as simple as stretching, making sure the joint moves through a range of positions that comfortably stretch its reach and flexibility slightly further each time.
Movement or physical activity is the best medicine for patients suffering from knee osteoarthritis. Performing physical activity might not only improve a patient’s joint mobility, but it can also improve their overall quality of life & can help reduce depression. Individuals with knee arthritis commonly engage in strengthening their knee muscles, neglecting however hip muscle strengthening. On assessing patients with knee arthritis they would usually be presented with hip muscle weakness & are more prone to an increase in medial compartment loading on the knee joint. Research has proven that patients with knee pain will benefit from hip-strengthening exercises. Potential benefits include quick pain relief & better hip strength. It is important to strengthen the hip in knee arthritis because hip strengthening exercises tend to improve the mechanics of the lower limb & reduce stress on the knee.
Exercises:

- Hamstring Stretch:
Stretching keeps the patient flexible & improves their range of motion, or how far they can move their joints in certain directions. It also helps patients lower their odds of pain & injuries.
Always warm up with a 5-minute walk, in starting. Lie down when a patient is ready to stretch her hamstring. Loop a bed sheet around the right foot. Use the sheet to assist pull the straight leg up. Hold for 20 seconds, then lower down the leg. Repeat twice. Then, switch the legs.

- Calf Stretch:
Hold onto a chair for balance. Bend the patient’s right leg. Step back with your left leg, & slowly straighten it behind you. Press your left heel toward the floor. You should feel the stretch in the calf of your backward leg. Hold for 20 seconds. Repeat twice, then switch legs.
For more of a stretch, lean forward & bend the right knee deeper but don’t let it go beyond your toes.

- Straight Leg Raise:
Build muscle strength to help support weak muscle joints.
Lie on the floor, upper body supported by the elbows. Bend left knee, foot on the floor. Keep the right leg straight, toes pointed upward. Tighten thigh muscles & raise right leg.
Pause, as shown, for 3 seconds. Keep your thigh muscles tight & slowly lower the leg to the ground. Touch & raise again. Do two sets of 10 repetitions. Switch legs after each set.

- Quad Set:
If the straight leg raise is too tough Do quad sets instead. With these, the patient doesn’t raise their leg. Simply tighten the thigh muscles, also known as the quadriceps, of one leg at a time.
Start by lying on the floor. Keep both legs on the ground, relaxed. Flex & hold left leg tense for 5 seconds. Relax. Do two sets of 10 repetitions. Switch legs after each set.

- Seated Hip March:
Strengthen hips & thigh muscles. It can assist with daily activities like walking or standing up.
Sit up straight in a chair. Kick the left foot back slightly, but keep the toes on the floor. Lift your right foot off to the floor, knee bent. Hold the right leg in the above for 3 seconds. Slowly lower the foot to the ground. Do two sets of 10 repetitions. Switch legs after each set.
If it is too hard Use your hands to help lift your leg.

- Pillow Squeeze:
This move helps strengthen the inside of the legs to help support the knees. Lie on your back, both knees bent. Place a pillow between the knees.
Squeeze the knees together, squishing the pillow between them. Hold for 5 seconds. Relax. Do two sets of 10 repetitions. Switch legs after each set.
If it is too tough You can also do this exercise while seated.

- Heel Raise:
Stand tall & hold the back of a chair for balance support. Lift heels off the ground & rise up on the toes of both feet. Hold for 3 seconds. Slowly lower both heels to the ground. Do two sets of 10 repetitions.
If it is too tricky Do the same exercise while sitting in a chair.

- Side Leg Raise:
Stand & hold the back of a chair for balance support. Place your weight on your left leg. Stand tall & lift the right leg out to the side keeping the right leg straight and the outer leg muscles tensed. Hold for 3 seconds, then slowly lower the leg down. Do two sets of 10 repetitions. Switch legs after each set.
If it is too hard Increase leg height over time. After a few workouts, the patient will be able to raise it higher.

- Sit to Stand:
Practice this exercise to make standing easier. Place two pillows on a chair. Sit near the edge, with your back straight, & feet flat on the floor. Use leg muscles slowly & smoothly to stand up tall. Then lower again to sit. Be sure bent knees don’t move ahead of the toes. Try with the arms crossed or loose at the sides.
If it is too tough to do Add pillows. Or use a chair with armrests & help push up with your arms.

- One Leg Balance:
This move helps patients bend over or get in & out of cars.
Stand behind the kitchen counter without holding on, & slowly lift one foot off the floor. The aim is to stay balanced for 20 seconds without grabbing the counter. Do this exercise twice, then switch sides.
If it is too easy Balance for a longer time. Or try it with the patient’s eyes closed.

- Step Ups:
Do this to strengthen the legs for climbing steps.
Stand in front of the stairs, & hold onto the banister for balance. Then place the left foot on a step. Tighten your left thigh muscle & step up, touching your right foot onto the step. Keep muscles tight as the patient slowly lowers her right foot. Touch the floor & lift again. Do two sets of 10 repetitions. Switch legs after each set.
- Walking:
Even if you have stiff or sore knees, walking might be a great exercise. Start slow, stand tall, & keep at it. You can ease joint pain, strengthen leg muscles, improve posture, & improve flexibility. It’s also good for the heart.
If the patient is not active now, check in with a doctor before you start a new exercise program.
- Low-Impact Activities:
Other exercises that are easy on the knees involve biking, swimming, & water aerobics. Water exercise reduces the weight of painful joints. Many community & hospital wellness centers, gyms, & pools offer classes for patients with arthritis.
Being active might also help you lose weight, which takes the pressure off your joints. For favorite activities, like golf, ask the doctor or physical therapist how to safely make painful moves hurt less.
- Aerobic exercise:
Aerobic exercise is any exercise that increases a patient’s pulse rate & makes you a bit short of breath. Regular aerobic exercise can help them in many ways. It’s good for their general health & well-being and can decrease pain by stimulating the release of pain-relieving hormones called endorphins. It can also help patients sleep well.
Different kinds of aerobic exercises include cycling, swimming, & walking. the patient should work hard enough to get out of breath but still be able to have a conversation.
You should try to do 2 hours & 30 minutes of aerobic exercise each week. the patient can spread this out over the week & doesn’t need to do it all in one go.
How much exercise should do?
Thirty minutes a day is a good aim. Initiate small, like with 10 minutes every other day. If the patient doesn’t have pain, exercise more to meet the goal.
Some mild muscle soreness is normal at starting. It’s OK to work through it. Check with the doctor if you want to try over-the-counter pain relievers like acetaminophen, ibuprofen, or naproxen to ease the soreness. Ice can also help. Don’t ignore the pain in your joints, though. Let the doctor know if the patient has any difficulty.
A new systematic review published in the journal Rheumatology Advances in Practice aiming to assess factors related to fatigue in individuals with hip & or knee arthritis found that there is strong or moderate evidence that high numbers of co-morbidities or illness burden & modifiable factors, such as high depressive symptoms, low levels of self-reported physical function, high pain & low physical activity levels, are associated with greater fatigue, making these factors possible targets for fatigue reduction in hip & knee arthritis populations. The review showed there was moderate evidence of no association between socio-demographic factors (age, education, race, living situation or circumstances), BMI, radiographic arthritis severity, and fatigue; & conflicting evidence for the association between poor performance-based physical function, high anxiety, high joint stiffness, poor sleep & low social support with higher fatigue.
Other Interventions
There are various forms of therapeutic interventions that might or might not be helpful for patients with various degrees of evidence to support them:
- Hydrotherapy – this might be particularly helpful if the pain is very high & analgesia is not tolerated. It can be helpful to build up strength & decrease the stiffness around the knee joint in a non-weight-bearing position.
- Taping – works to offload the joint same as bracing, this is useful in the short term. A systematic review shows elastic taping leads to no significant change in WOMAC score for improvement of pain in patients with primary knee osteoarthritis & alternative conservative treatments to elastic taping should be explored if arthritis knee pain persists for more than 21 days.
- Manual therapy – effective to improve ROM According to a systematic review, manual therapy mobilization with movement, passive joint mobilization, and patellar mobilization therapy & exercises effectively reduce knee pain & increase functionality. Nevertheless, further research is needed to determine the long-term effects of manual therapy on knee arthritis.
- Massage – might be useful to control pain in some subjects, but this has low evidence to show its effectiveness.
- Bracing -to support the joint.
- Electrotherapy -such as muscle stimulation to improve quadriceps strength & TENS as it has some evidence to show it can help with pain reduction.
Alternative treatment Option
Many alternative forms of therapy are unproven but might be helpful to try, provided the patient finds a qualified practitioner & keep the doctor informed of your decision. Alternative therapies to treat pain include the usage of acupuncture, magnetic pulse therapy, platelet-rich plasma, & stem cell injections.
Acupuncture uses fine needles to stimulate specific body sites to relieve pain or temporarily numb an area. Although it is used in many parts of the world & evidence suggests that it can help ease the pain of arthritis, there are few scientific studies of its effectiveness. Be sure the acupuncturist is certified, & do not hesitate to ask about his or her sterilization practices.
Magnetic pulse therapy is painless & works by applying a pulsed signal to the knee, which is situated in an electromagnetic field. Like many alternative therapies, magnetic pulse therapy has not been proven yet.
Treatments such as platelet-rich plasma (PRP) & stem cell injections involve taking cells from your own body & re-injecting them into a painful joint. platelet-rich plasma uses a component of the patient’s own blood, platelets, that have been separated from the blood, concentrated & injected into your knee. The platelets contain “growth factors” thought to be helpful in decreasing the symptoms of inflammation.
Stem cells are precursor cells that can also be taken from the patient’s own body & injected into the knee. Since they are basic cells, they might have the potential to grow into new tissue & thus heal damaged joint surfaces.
Glucosamine & chondroitin. A few have found benefits for patients with osteoarthritis, while most indicate that these supplements work no better than a placebo. Glucosamine & chondroitin can interact with blood thinners such as warfarin Jantoven, & cause bleeding problems.
Avocado-soybean unsaponifiable. This nutritional supplement — a mixture of avocado & soybean oils — is widely used in Europe to treat knee & hip osteoarthritis. It acts as an anti-inflammatory, & some studies have shown that it can slow or even prevent joint damage.
Omega-3 fatty acids. Omega-3s, found in fatty fish & fish oil supplements, might help relieve pain & improve function.
Talk to the doctor about the supplements you’re considering.
While both treatments show promise, clinical studies have yet to confirm their importance in managing osteoarthritis.
Summary
The features of knee arthritis will depend, to some extent, on the type of arthritis. Pain, swelling, & a loss of mobility are common with different types of arthritis.
There’s no cure for arthritis, but management can relieve symptoms, slow the progress of the disease, & decrease the risk of complications. In the case of rheumatoid arthritis, medication might help reduces the frequency & severity of flares.
Strategies, such as weight management & exercise, might help postpone or eliminate the requirement for surgery in the future. the doctor will help the patient make the best decisions for the type of knee arthritis they have.
FAQ (frequently asked questions)
Knee arthritis can make it hard to do many daily activities, such as walking or climbing stairs. It is a major cause of lost work time & a serious disability for many patients. The most common types of arthritis are osteoarthritis & rheumatoid arthritis, but there are more than 100 different forms of arthritis.
Untreated arthritis will add to the degradation of the structures in & around the joint leading to more & more pain and a loss of function. The progression of arthritis might lead to needing a total joint replacement.
5 signs patient may need knee replacement surgery
Persistent or reoccurring pain.
The pain prevents the patient from sleeping.
the patient has difficulty doing daily activities including walking or climbing stairs.
patient’s knees are stiff or swollen.
Knee deformity is bowing in or out of the knee.
Experts confirm that once arthritis starts, it might take years to reach a severe stage. Nevertheless, in extreme cases, arthritis progresses rapidly to complete the destruction of the cartilage within a few months. Some of the factors that determine the rate of arthritis progression include The severity of the patient’s symptoms at the time of diagnosis.
The age bracket of 50 to 70 years is the most usual age group for knee replacement patients. Older patients above the age of 70 might also benefit immensely from the mobility & comfort offered by a prosthesis.