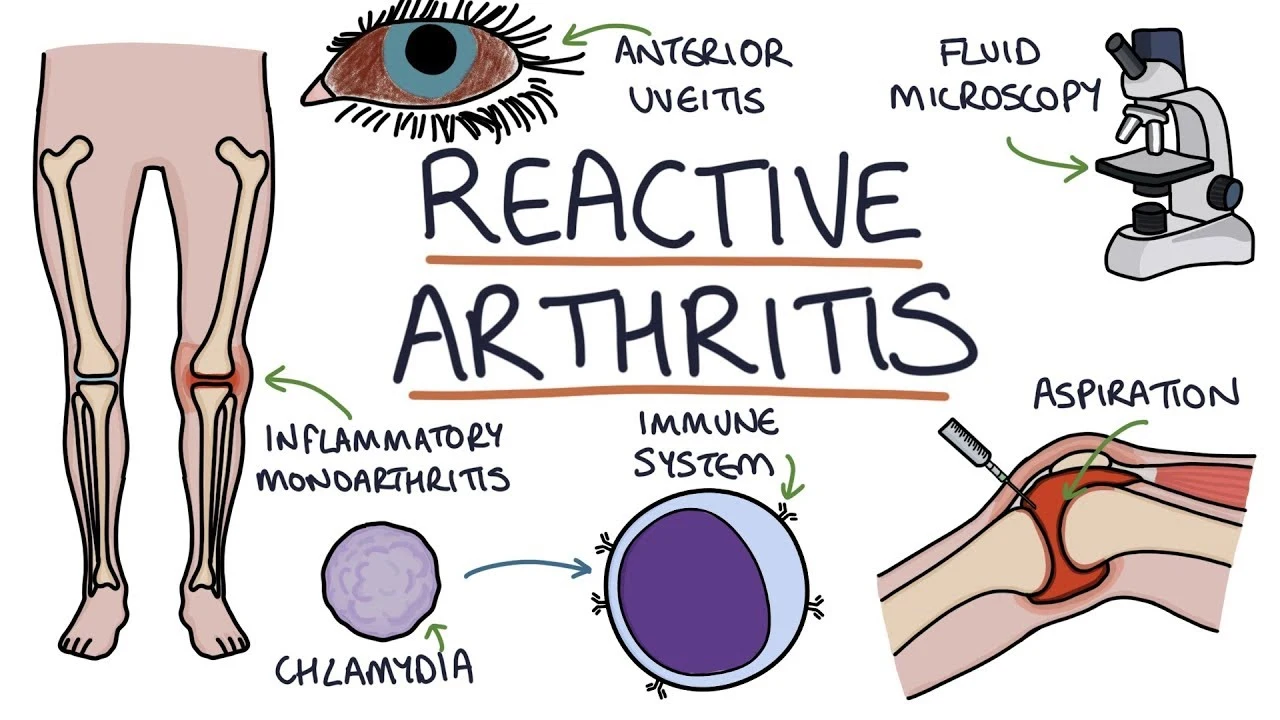
Reactive arthritis
Table of Contents
What is reactive arthritis?
Reactive arthritis, also known as Reiter’s syndrome, is a form of inflammatory arthritis that occurs in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria & develop an infection can trigger the disease. By the time the patient presents with symptoms, frequently the “trigger” infection has been cured or is in remission in chronic cases, thus making a determination of the initial cause difficult.
Arthritis frequently is coupled with other characteristic symptoms; this has been called Reiter’s syndrome, Reiter’s disease, or Reiter’s arthritis. The term “reactive arthritis” is increasingly utilized as a substitute for this designation because of Hans Reiter’s war crimes with the Nazi Party.
The manifestations of reactive arthritis involve the following triad of symptoms: inflammatory arthritis of large joints, inflammation of the eyes in the type of conjunctivitis or uveitis, & urethritis in men or cervicitis in women. Arthritis occurring alone after sexual exposure or enteric infection is also known as reactive arthritis. Patients can also present with mucocutaneous lesions, as well as psoriasis-like skin lesions such as circinate balanitis, & keratoderma blennorrhagicum. Enthesitis can involve the Achilles tendon outcome in heel pain. Not all affected patients have all the manifestations.
The clinical pattern of reactive arthritis usually consists of an inflammation of fewer than five joints which frequently includes the knee or sacroiliac joint. Arthritis might be “additive” (more joints become inflamed in addition to the primarily affected one) or “migratory” (new joints become inflamed after the starting inflamed site has already improved).
Reactive arthritis is an RF-seronegative, HLA-B27-linked arthritis frequently precipitated by genitourinary or gastrointestinal infections. The most usual triggers are intestinal infections with Salmonella, Shigella, or Campylobacter & sexually transmitted infections (with Chlamydia trachomatis); Nevertheless, it also can happen after group A streptococcal infections.
It most commonly strikes individuals aged 20–40 years of age, is more common in men than in women, & is more common in white than black people. This is due to the high frequency of the HLA-B27 gene in the white population. It can occur in epidemic form. Patients with HIV have an increased risk of occurring reactive arthritis as well.
Numerous cases during World Wars I and II focused attention on the triad of arthritis, urethritis, & conjunctivitis (often with additional mucocutaneous lesions), which at that time was also referred to as Fiessenger-Leroy-Reiter syndrome.
What are the causes of reactive arthritis?
Reactive arthritis occurs in reaction to an infection in the patient’s body, frequently in the intestines, genitals, or urinary tract. The patient might not be aware of the triggering infection if it causes mild features or none at all.
Reactive arthritis is known to be attacked by a bacterial infection, particularly of the genitourinary Chlamydia trachomatis, Neisseria gonorrhea, Mycoplasma hominis, & Ureaplasma urealyticum or gastrointestinal (GI) tract Salmonella enteritidis, Shigella flexneri, & S. disenteriae, Yersinia enterocolitica, Campylobacter jejuni, Clostridium difficile. The incidence is about 2% to 4% after a urogenital infection, mainly with Chlamydia trachomatis, & varies from 0% to 15% after gastrointestinal infections with Salmonella, Shigella, Campylobacter, or Yersinia. This may be affected by the epidemiological, and environmental factors, the pathogenicity of the bacteria, & differences in the study programs. The enteric ReA develops commonly following enteric infections. Nevertheless, chlamydia-associated Reactive Arthritis is endemic, especially in developed countries.
Rare conditions have been reported after carrying out the Bacillus Calmette Guerin vaccine (BCG) treatment for bladder cancer.
The most general causes of reactive arthritis are:
- stomach upsets
- diarrhea
- other infections in the gut
- a throat infection – usually caused by streptococcus bacteria.
- slapped cheek syndrome
- glandular fever.
The infection that causes reactive arthritis can be so mild that you might not feel unwell until you’re aware of the pain in the joints.
We don’t yet know why some persons get reactive arthritis, but we do know that it’s linked to a gene that some people inherit, called HLA-B27. These people appear to be more likely to develop reactive arthritis & to get it more than once in their life.
What are the symptoms of reactive arthritis?
Keratoderma blennorrhagicum because of reactive arthritis. Because common systems involved the eye, the urinary system, & the hands and feet, one clinical mnemonic in Reactive arthritis is explained with”Can’t see, can’t pee,& can’t climb a tree.”
The classic triad consists of:
- Conjunctivitis
- Nongonococcal urethritis
- Asymmetric oligoarthritis
Symptoms generally seem within 1–3 weeks but can range from 4 to 35 days from the onset of the inciting episode of the disease.
The classical presentation of the syndrome starts with urinary symptoms such as burning pain during urination (dysuria) or an increased frequency of urination. Other urogenital problems might arise such as prostatitis in men & cervicitis, salpingitis & vulvovaginitis in women.
Patients significantly present with acute onset oligo-arthritis, mainly involving the lower extremities, sacroiliac joint, & lumbar spine. Not more than 6 large joints are affected at a time, & the knee and ankle are the most commonly affected. Joint pain is classically nocturnal with early morning stiffness. Involvement is asymmetric & affects the weight-bearing joint. The joints are often warm, painful, & swollen. Tendinitis is a usual feature of the disease. About 30% of patients suffer from related enthesitis in the form of plantar fasciitis or Achilles tendinitis.
It presents with monoarthritis affecting the large joints such as the knees & sacroiliac spine causing pain and swelling. Asymmetrical inflammatory arthritis of interphalangeal joints might be present but with relative sparing of small joints such as the wrist & hand.
Patients can have enthesitis presenting as heel pain, Achilles tendinitis, or plantar fasciitis, along with balanitis circinata (circinate balanitis), which involves penile lesions present in roughly 20 to 40 percent of men with the disease.
A small percentage of men & women develop small hard nodules called keratoderma blennorrhagicum on the soles of the feet & less commonly, on the palms of the hands or elsewhere. The existence of keratoderma blennorrhagica is diagnostic of reactive arthritis in the nonattendance of the classical triad. Subcutaneous nodules are also a sign of this disease.
Ocular involvement (mild bilateral conjunctivitis) occurs in about 50 % of men with urogenital reactive arthritis syndrome & about 75 % of men with enteric reactive arthritis syndrome. Conjunctivitis & uveitis can involve redness of the eyes, eye pain & irritation, or blurred vision. Eye involvement typically occurs early in the course of reactive arthritis, and symptoms might come and go.
Dactylitis, or “sausage digit”, a diffuse swelling of a solitary finger or toe, is a distinctive feature of reactive arthritis & other peripheral spondylarthritides but can also be seen in polyarticular gout & sarcoidosis
Mucocutaneous lesions can be present. Common findings involve oral ulcers that come and go. In some cases, these ulcers are painless & go unnoticed. In the oral cavity, the patients might experience recurrent aphthous stomatitis, geographic tongue & migratory stomatitis is more prevalent than in the general population.
Some patients experience serious gastrointestinal problems same to those of Crohn’s disease.
About 10 % of people with reactive arthritis, especially those with a prolonged course of the disease, will develop cardiac manifestations, involving aortic regurgitation & pericarditis. Reactive arthritis has been explained as a precursor of other joint conditions, involving ankylosing spondylitis.
Men:
- Increased urine
- Burning sensation during urination
- Discharge from penis
- Inflamed prostate gland (prostatitis)
Women:
- Inflamed cervix
- Inflamed urethra. This leads to a burning sensation during urination.
- Inflamed fallopian tubes (salpingitis)
- Inflamed vulva and vagina (vulvovaginitis)
- Eye Symptoms
- Red eyes
- Painful & irritated eyes
- Blurry vision
- The inflamed mucous membrane that covers the eyeball and eyelid (conjunctivitis)
- Inflammation of the inner eye (uveitis)
What are the Risk factors of reactive arthritis?
Certain factors increase a patient’s risk of reactive arthritis:
- Age. Reactive arthritis occurs most often in adults between the ages of 20 & 40.
- Sex. Women & men are equally likely to develop reactive arthritis in response to foodborne infections. Nevertheless, men are more likely than women to occur reactive arthritis in response to sexually transmitted bacteria.
- Hereditary factors. A specific genetic marker has been linked to reactive arthritis. But most populations who have this marker never develop the condition.
- Having an infection from sexual contact
- Having illness from contaminated food
Some patients with reactive arthritis have a gene called HLA-B27. Patients who test positive for HLA-B27 frequently have a more sudden & severe onset of symptoms. They also are more prone to have chronic symptoms. Yet, patients who are HLA-B27 negative can still get reactive arthritis after exposure to an organism that causes it.
How to prevent reactive arthritis?
Genetic factors seem to play a role in whether you’re likely to develop reactive arthritis. Though you can’t change your genetic makeup, you can decrease your exposure to the bacteria that might lead to reactive arthritis.
Store your food at proper temperatures & cook it properly. Doing these things help you avoid the many foodborne bacteria that can cause reactive arthritis, including salmonella, shigella, yersinia & campylobacter. Some sexually transmitted infections can attack reactive arthritis. Use condoms to help lower the risk of infection from sexual contact.
What is the differential diagnosis of reactive arthritis?
The physician should be able to rule out conditions that appear with similar clinical findings. The most common differential diagnosis should involve:
- Gonococcal arthritis
- Gouty arthritis
- Still disease
- Septic arthritis
- Rheumatic fever
- Psoriatic arthritis
- Ankylosing spondylitis
- Rheumatoid arthritis
- Immunotherapy or immunization–related arthropathy
- Secondary syphilis
- Tubercular arthritis
What is the diagnostic procedure for reactive arthritis?
Reactive Arthritis falls within the subcategory of seronegative spondyloarthropathies that affect the axial skeleton. Other participants in that group are Ankylosing spondylitis & Psoriatic arthritis. Joint involvement is oligoarticular & asymmetrical.
American College of Rheumatology came up with diagnostic criteria for Reactive arthritis in 1999. The criteria were classified into
- MAJOR
Asymmetric oligo or monoarthritis involving lower extremities
Either enteritis or urethritis symptoms preceding the onset of arthritis with a time interval of 3 days to 6 weeks - MINOR
existence of a triggering infection as evidenced by culture positivity
Presence of persistent synovial involvement
A combination of genitourinary symptoms, metatarsophalangeal joint involvement, elevated C reactive protein, & positive HLA- B27 renders a 69% sensitivity & 93.5% specificity to the diagnosis of reactive arthritis.
Although reactive arthritis is a clinical diagnosis, laboratory tests to find the offending pathogens to confirm concomitant or preceding infections are commonly done to support the diagnosis. Nucleic acid amplification tests from an early morning urine sample or urogenital swab are used to detect Chlamydia trachomatis & Neisseria gonorrhea. A nucleic acid amplification test for Mycoplasma genitalium is also available nowadays & is relevant in men with urethritis.
Positive evidence of Chlamydia by polymerase chain reaction (PCR) in the joint is probably majorly diagnostic, but the current methods used for the finding of chlamydia in the urine are not validated for diagnostic aims for synovial samples. Serological testing for Chlamydia trachomatis is of limited importance because of serological cross-reactivity between Chlamydia trachomatis & Chlamydia pneumonia, inability to differentiate past & present infection by the endless of antibodies, lower or absent antibody feedback in lower urinary tract infections. Serological testing is available for Salmonella, Yersinia, & Campylobacter but is not useful in clinical practice. There are also gastrointestinal infections, for example, Shigella, in which no reliable serological methods are present. A stool culture might be helpful to detect enteric pathogens.
Certain complications, like uveitis, are important to identify. The slit-lamp exam is useful to diagnose cells in the anterior chamber in acute iritis. Therefore, the presence of ocular symptoms in a suspected patient should create a prompt referral to an ophthalmologist. The usual presentation of uveitis will involve acute pain, photophobia, visual impairment, scleral injection, & hypopyon.
Acute phase reactants such as the erythrocyte sedimentation rate (ESR) or C-reactive protein might be raised. Joint aspiration must be done when possible to rule out other arthritis. Aspiration of the joint is frequently done to rule out septic arthritis & crystalline arthritis. The findings in synovial fluid are nonspecific & are characteristic of inflammatory arthritis, with raised leukocyte counts (typically 2000 to 4000 WBC per ml), with neutrophil predominance.
HLA B 27 can be measured as it correlates with the severity of the condition but is not diagnostic. It is also key in the localization of arthritis. Sacroiliitis occurs more usually in HLA B 27-positive patients.
In a patient from an endemic population, the tuberculin skin test should be done.
Plain radiographs might show nonspecific inflammatory joint findings in the acute phase. Ultrasonography or magnetic resonance imaging (MRI) can be performed to diagnose peripheral synovitis, enthesitis, or sacroiliitis. Scintigraphy can show the early stages of enthesitis.
What is the treatment plan for reactive arthritis?
There are three ways patients with reactive arthritis can be treated:
Medical treatment for reactive arthritis:
Treating the infection:
If the patient is still showing signs of infection, the doctor will prescribe antibiotics. This will not treat the inflammation in the joint but should get rid of the bacteria that caused the infection in the first place.
If a patient had a stomach upset, or bowel or genital tract infection, they’ll probably be given oral antibiotics. Conjunctivitis is frequently treated with eye drops or ointment. More severe inflammatory eye conditions, such as iritis or uveitis, might require steroid eye drops.
Antibiotic treatment shouldn’t last more than four weeks.
Treating the inflammation:
If a patient has mild to moderate pain and inflammation, your doctor might prescribe non-steroidal anti-inflammatory drugs (NSAIDs). These include ibuprofen or naproxen.
Before prescribing NSAIDs, the doctor will consider your medical & lifestyle history for other risks, such as:
- smoking
- circulation problems
- high blood pressure
- high cholesterol
- diabetes.
A patient will generally be given the lowest effective dose of NSAID for as short a time as possible.
If the patient has a history of stomach problems, the doctor might prescribe a proton pump inhibitor (PPI) with the NSAID. This will stop a patient from getting stomach upsets, indigestion, or damage to the lining of the stomach.
A major part of reactive arthritis is fatigue or extreme tiredness it causes. It’s important to recognize when you’re tired & need to rest, but it’s also important to keep up some level of activity. Bed rest can do much more harm than good.
When a patient’s symptoms are at their worst, they should try to get plenty of rest & avoid putting too much strain on the affected joint. If a patient can gently move it, this should stop it from becoming too stiff. the doctor might refer you to an occupational therapist or a physiotherapist.
Treating arthritis:
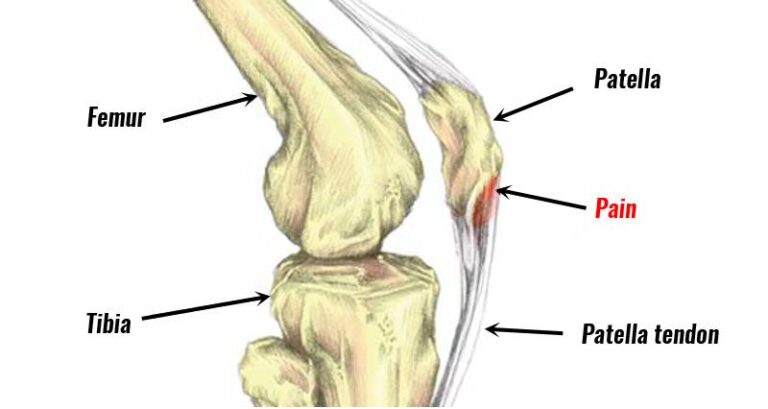
If symptoms are really bad & other treatments haven’t helped, the doctor might recommend an injection to remove the fluid that is causing the swelling in your joint. This is called aspiration.
Once the inflammation has gone down, the patient might be given a steroid injection into the joint. This is frequently used to help with knee pain.
If reactive arthritis is bad, the patient might need a steroid injected into a muscle. This will help the steroid spread through the body. Alternatively, patients might be given low-dose steroid tablets, which frequently work very well in the short term.
If these treatments haven’t helped after a few weeks and symptoms are still bad, a patient might be prescribed disease-modifying anti-rheumatic drugs (DMARDs), such as sulfasalazine&, occasionally, methotrexate, or azathioprine.
DMARDs work on the underlying condition, rather than managing symptoms. They’re not painkillers, but they’ll decrease pain, swelling, & stiffness over weeks or months by slowing down the condition & its effects on the joints.
There are two kinds of patients who might be prescribed for reactive arthritis: conventional DMARDs & biological therapies. They can take between 6 weeks & 6 months to work. They can be prescribed on their own or with steroids or NSAIDs.DMARDs can cause changes in the blood or liver, so it’s important to have regular blood tests while taking them.
Immunosuppressive medicines such as methotrexate control inflammation. Strong biological immunosuppressants gave as a shot. Methotrexate & sulfasalazine can sometimes make them feel sick, have diarrhea, headaches or lose their appetite, at first. These are usual side effects & should clear up, once your body gets used to the drug.
Speak to a doctor if your medication isn’t working, or you’re worried about side effects. If conventional DMARDs don’t work for you, the patient might be prescribed injections of biological therapy. These are also called biologics.
Biologics are a newer kind of drug that is prescribed when conventional DMARDs haven’t worked. DMARDs & biological therapies can lower the body’s ability to fight infections, so patients should try to neglect people who have bacterial illnesses such as tummy bugs, colds, or sore throats.
Rest to ease pain & inflammation
Tell a doctor right away if you develop any signs of infection, such as:
- a sore throat or fever
- any unexplained bruising or bleeding
- breathlessness
- jaundice when the eyes & skin seem yellow.
Patients should also see a doctor if they come into contact with anyone who has chickenpox or shingles, or if they develop chickenpox or shingles themselves.
- Tips to decrease your risk of infection
- Try to avoid close contact with patients who have an infection.
- Wash hands regularly & carries around a small bottle of antibacterial hand gel.
- Keep your mouth clean by brushing your teeth in a routine.
- Stop smoking if you’re a smoker.
- Make sure the food is stored & made properly.
- Try to keep your house clean & hygienic, especially the kitchen, bathrooms, & toilets.
- If a patient is prescribed a drug you might find more information about it here.
When a patient’s joints are inflamed & painful, you can feel tired & generally unwell. Fatigue plays an important role in reactive arthritis & can have a huge impact on all aspects of your life. It’s important that you and the people around you recognize this.
It’s equally as important to keep moving. You could try:
swimming in a heated pool – this allows you to exercise while the water supports a weight
stretching exercises, keep the muscles & tendons that support the joint strong and supple
talking to their line manager about working shorter hours
asking whether the patient can avoid any activities that are too demanding
making their workstation better suited to their condition.
The doctor can refer you to a physiotherapist or occupational therapist for specific advice.
Getting a good night’s sleep & recognizing when you need to relax is really important to your recovery. If you’re finding it difficult to wind down relaxation techniques, such as breathing exercises, mindfulness, or meditation, might help.
A good bedtime routine can also make them feel better. Try to get an early night & give yourself an hour before to have a warm bath and relax, try to avoid using your computer, phone or TV in that hour, as they can disrupt your sleep.
Complementary & alternative treatments
Complementary & alternative treatments, such as acupuncture, massage, & supplements, might help your symptoms.
There can be risks associated with some complementary & alternative treatments. Patients should let their doctor know about any complementary therapies they’re considering, as some can react with prescribed medications.
Physiotherapy treatment for reactive arthritis:
Physiotherapy will help with reactive arthritis in various ways. Your treatment program will be tailored to specifically manage symptoms & help you return to your normal activities of daily living. Physiotherapy might help in the following ways:
- Reduce inflammation
- Reduce pain
- Improve range of movement
- Increase cardiovascular levels
- Help return to activities of daily living & sports
- Increase energy levels
Physical Therapy Management
Physical Therapy is helpful during the recovery phase of the disease after the exacerbation of symptoms has ceased. Physical Therapy should follow a program same to that given to a patient with arthritis.
Patient education – this is necessary to promote joint protection & proper body mechanics when performing daily activities to maintain joint integrity.
An exercise regimen – that involves regular aerobic activity, as well as exercises that promote the joint range of motion & muscle strengthening should be utilized.
- Aerobic exercise should include low-impact activities, such as swimming, walking, or a recumbent bike, depending on the patient’s cardiovascular level.
- Strengthening should target muscles surrounding the affected joints with the purpose of improving their support system.
for acute joint inflammation, give the advice to avoid overuse.
If enthesitis is present, heel support & orthosis can be considered to decrease pain & thus improve mobility. Patients might choose to recommend a short period of non-weight bearing, to decrease the inflammation & limit the pressure of the body on the inflamed joints.
Stretching & ROM exercises should be completed to prevent muscle atrophy, especially if several joints are involved. The objective of physiotherapy is to avoid stiffness & deformities and to promote mobility & strength.
- Hydrotherapy
- Cryotherapy (ice therapy)
- Transcutaneous electrical nerve stimulation (TENS)
When recovery takes place, patients must be instructed not to overload their joints too soon, to avoid minor traumas which can cause a relapse.
Immobilization & inactivity are discouraged as they can lead to decreased range of motion, contractures, joint stiffness, decreased muscle strength, & decreased flexibility, as well as overall decreased cardiovascular fitness, which can lead to a cascade effect on other body systems. The goals of treatment should include pain relief, improved activities of daily living, reduce joint swelling, and prevention of joint damage & disability.
What are the complications of reactive arthritis?
Complications include:
- Recurrent arthritis (15 to 50%)
- Chronic arthritis or sacroiliitis
- Ankylosing spondylitis
- Urethral stricture
- Aortic root necrosis
- Cataracts
- Cystoid macular edema
What is the prognosis of reactive arthritis?
Reactive arthritis might be self-limiting, frequently recurring, chronic, or progressive. 15 to 50 % of cases include recurrent bouts of arthritis. Chronic arthritis or sacroiliitis occurs in 15–30 % of cases. Repeated attacks over many years are common, & patients sometimes end up with chronic & disabling arthritis, heart disease, amyloid deposits, ankylosing spondylitis, immunoglobulin A nephropathy, cardiac conduction abnormalities, or aortitis with aortic regurgitation. Nevertheless, most people with reactive arthritis can expect to live normal life spans & maintain a near-normal lifestyle with modest adaptations to protect the involved organs.
Patients who are HLA-B27 positive have much more risk of recurrence of reactive arthritis. 15-30% of patients with reactive arthritis can develop long-term arthritis or other joint abnormalities. The presence of hip involvement, unresponsiveness to NSAIDs, & ESR greater than 30 portend a worse outcome.
FAQ (frequently asked questions)
Reactive arthritis is a type of inflammatory arthritis. Unlike other types of inflammatory arthritis, for many people, reactive arthritis lasts a relatively amount of time commonly around three months to a year. Nevertheless, some people find it lasts longer & can have random flare-ups years after they first get it.
There’s no cure for reactive arthritis, but the disease is usually temporary & treatment can help to relieve symptoms. Most patients will make a full recovery in about six months, although around one in five cases lasts a year or more, & a small number of patients experience long-term joint problems.
Reactive arthritis is joint pain & swelling triggered by an infection in another part of the body most frequently the intestines, genitals, or urinary tract.
In patients with rheumatoid arthritis, the body releases less of the anti-inflammatory chemical cortisol at night, increasing inflammation-related pain.