Tietze’s Syndrome
- Tietze syndrome is a rarely seen inflammatory condition that causes chest pain and cartilage swelling near your upper ribs. Symptoms involve chest pain, swelling, and tenderness near your ribs. Tietze syndrome treatments involve rest, NSAIDs & corticosteroids.
Table of Contents
What is Tietze syndrome?
- Tietze syndrome is a painful inflammation in the cartilage located at the costochondral joint – where your ribs join to your breastbone (sternum). You might look at it referred to as Tietze’s syndrome or costochondral junction syndrome. These names all refer to a similar condition.
- Cartilage is a strong, flexible connective tissue that protects your joints & bones. It likes like a shock absorber throughout your body. The cartilage that connects your ribs to your breastbone is stiff and strong to assist your ribcage to protect organs such as your heart and lungs.
- Tietze syndrome occurs when the cartilage in the joint where your ribs connect to your breastbone — your costochondral joint — is irritated. This irritation conducts to inflammation around the joint and causes chest pain and swelling.
- Tietze syndrome is treated with rest & over-the-counter medicine. It usually takes certain weeks for the inflammation to go away and your symptoms to get better.
Tietze syndrome vs costochondritis
- Tietze syndrome is very same to costochondritis, another type of irritation in your costochondral joint.
- The biggest difference between them is swelling and which ribs they commonly affect.
- Tietze syndrome causes pain, tenderness, and swelling near harmed costochondral joints. It commonly affects ribs higher up on your ribcage, closer to your shoulders — usually your second or third ribs.
- If you have costochondritis, you will feel the pain that may start on the left side of your chest & spread (radiate) out to the rest of your chest. The symptoms are almost identical to Tietze syndrome, except costochondritis does not cause swelling that you can see or feel outside your body. It usually harms ribs lower down your ribcage — usually ribs two through five.
- Because Tietze syndrome and costochondritis are so similar, they are sometimes confused with each other. The good news is they are usually treated and diagnosed the same way. Talk to your healthcare provider (doctor) if you have any pain or swelling in or around your chest.
Whom does Tietze syndrome affect?
- Tietze syndrome can affect anyone, but it is more common in people under 40. People older than forty are more likely to experience costochondritis rather than Tietze syndrome.
You might be more likely to irritate your costochondral joint and develop Tietze syndrome if you have certain conditions, including:
- Psoriatic arthritis & rheumatoid arthritis.
- Other autoimmune diseases,
- Conditions that make you cough or sneeze a lot such as sinusitis or laryngitis.
How common is Tietze syndrome?
- Tietze syndrome is infrequent. Experts do not know exactly how many people each year develop Tietze syndrome because it is not recorded very often.
How does Tietze syndrome affect my body?
- The most obvious way Tietze syndrome will harm you is the pain in your chest.
- Depending on which ribs are harmed, it might harm more when you move or twist your upper body. It can harm sitting or lying down in certain positions.
- Coughing, sneezing & vomiting, while you have Tietze syndrome, will be painful.
What are the symptoms of Tietze syndrome?
Symptoms of Tietze syndrome involve:
- Chest pain,
- Tenderness on or near your ribs,
- Swelling,
- A feeling of warmth,
- Discoloration.
Your symptoms might look sudden or develop over time.
What causes Tietze syndrome?
- Experts are not sure what causes Tietze syndrome. Certain experts think activities that put small, repeated stress on your ribs over time (microtraumas) can conduct to Tietze syndrome.
Microtraumas can involve:
- Coughing,
- Vomiting,
- Infections.
- Getting hit in the chest sometimes during a sport or other physical activity.
- Studies have found that traumas such as car accidents, falls and sports injuries might cause Tietze syndrome.
How is Tietze syndrome diagnosed?
- Diagnosing Tietze syndrome is sometimes known as a diagnosis of elimination. This means your provider might do an exam and perform tests to rule out other, more serious conditions previously diagnosing Tietze syndrome as the cause of your pain.
- Your provider (doctor) will diagnose Tietze syndrome with a physical exam and imaging tests.
- They will feel your chest and ribs. They might press on your chest to sense how sensitive you are and to pinpoint where your pain is most intense (localized). They will examine your torso for other signs of injuries or conditions that might be causing your symptoms.
- You might require a blood test to check for infections or other issues.
Your provider may also need some imaging tests, involving:
- Chest X-ray,
- A CT scan,
- MRI,
- Ultrasound,
- Electrocardiogram (EKG).
How is Tietze syndrome treated?
- Tietze syndrome is commonly treated by resting your chest and ribcage. Your body conducts time to heal the irritation inside your costochondral joint. Over-the-counter NSAIDs can reduce your pain and reduce swelling. Talk to your provider about previously taking NSAIDs for more than 10 days in a row.
- It is rare, but if your symptoms are not improving after a few weeks, your provider might inject a corticosteroid into your joint to reduce the inflammation.
- Some people with Tietze syndrome get better without treatment but do not assume you do not need treatment. Visit your provider as soon as you notice swelling on or around your chest, especially if you are in pain.
Physical Therapy Management
- The treatment of Tietze’s syndrome is not perfect. It is not called whether the disease is dealt definitely or not. So the treatment of Tietze syndrome is mostly symptomatic. At the current, trustworthy clinical studies on the treatment of Tietze’s syndrome are lacking.
The physiotherapist can:
- Reassure the patient by explaining the condition.
- Instruct a good body position and give exercise advice. Patients require a good balance between exercise and rest. It is important that the physiotherapist gives the best information about the posture of the patient during sitting and during daily activities. It is also important that the patient avoids repetitive movements/ activities.
- Exercises in the range of motion (ROM) should be induced as soon as possible. The patient may not be having pain when he is doing the exercises. If powerful exercises exacerbate the symptoms, you require to stop and avoid this kind of exercise.
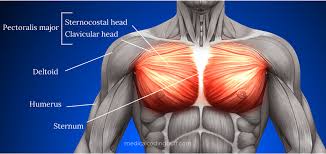
- Stretching of the M. pectoralis major can be assisted. You can stretch the M. pectoralis major when you stand in a corner for 10 (ten) sec with both of your hands against the wall (like when you do a push-up). You require to repeat it a few times a day for 1 or 2 minutes.
- Use heat/ cold pads and massage to assist against the overloading of muscles and to lessen the pain. Heat and cold pads are both similarly effective. So the patient can choose which one he such as the most. Instead of using cold pads, the patient can also utilize Vapocoolant spray on the involved parts. This spray can release pain in the chest.
- Mobilize the spine and ribs to avoid the rigidity of the thorax and to decrease complaints.
- Learn the patient copes with pain.
- Exercise for the shoulder and back can be provocative, therefore only when the complaints have disappeared, they can be applied.
- On the painful part, they can use transcutaneous electrical stimulation and electroacupuncture. The acupuncture needle is placed within the included spinal segment. Then decrease-frequency electrical currents are applied to the inserted needle.
- Dry needling: Musculoskeletal chest wall pain has traditionally been a difficult part to evaluate and treat. Injection
- therapy with local anesthetics or corticosteroids has been only described as a treatment method for costochondral-related chest wall pain. Results of previous research studies have indicated that dry needling may be as effective as injection therapy for different conditions.
How long does Tietze syndrome last?
- Tietze syndrome commonly lasts for a few weeks, but it depends on how long it takes the inflammation in your costochondral joint to heal. Certain people’s bodies take longer to repair the damage inside their joints, but Tietze syndrome should not last more than a few months.
- Talk to your provider if you are still experiencing pain and other Tietze syndrome symptoms after a few weeks.
How can I prevent Tietze syndrome?
- Because experts are not sure what causes Tietze syndrome, it is hard to say for sure how you can prevent it.
- In common, avoid putting too much stress on your chest and ribs. Make sure to rest later through intense physical activity to give your body time to recover.
What can I expect if I have Tietze syndrome?
- You should expect to create a full recovery from Tietze syndrome. Once the inflammation is healed, you should be able to return to all your common activities with no long-term effects.
- The worst part of Tietze syndrome is usually the chest pain that makes people think they are having issues with their hearts. Get new symptoms examined right away to rule out something more severe.
Will I need to miss work or school while I am recovering from Tietze syndrome?
- You should not have to miss work or school while you are recovering if you can do your job or studies without putting too much stress on your ribs.
- Talk to your provider previous resuming any intense physical activity, especially if you are recovering from a sports injury.
When should I see my healthcare provider?
- Visit your provider (doctor) right away if you notice any new symptoms in or around your chest, especially pain or swelling. Tietze syndrome is not usually a dangerous condition, but it is important to rule out other, more serious issues as soon as possible.
When should I go to ER?
Call 911 or your local emergency services phone number if you think you are experiencing heart attack symptoms, including:
- Shortness of breath or trouble breathing,
- Nausea or stomach discomfort,
- Heart palpitations,
- A feeling of anxiety or “impending doom,
- Sweating,
- Feeling lightheaded or dizzy.
What questions should I ask my doctor?
- Do I have Tietze syndrome or costochondritis?
- Which tests will I need?
- How long will it take to heal?
- Which activities should I avoid while I am recovering?
- When can I resume physical activities like sports?
Which conditions have similar symptoms to Tietze syndrome?
In addition to costochondritis, Tietze syndrome has symptoms that are similar to lots of other conditions. Some of the most usual conditions that can also cause pain in your chest or around your ribs to include:
- Rib fractures,
- GERD (chronic acid reflux),
- Fibromyalgia,
- Lupus.
Visit your provider (doctor) if you have new symptoms in your ribs or chest. Tietze syndrome does not usually cause breast pain or muscle pain.
NOTE
- It is scary to experience chest pain, especially if it happens suddenly. But Tietze syndrome is not a sign of anything wrong with your heart. It is temporary inflammation that will get better.
- Because Tietze syndrome is rare and shares symptoms with so many other conditions, do not ignore pain or swelling near your ribs. The sooner you look at your Doctor, the faster you can get back to your regular routine pain-free.
FAQs
No one knows exactly what causes Tietze syndrome. Certain experts believe that it is caused by many tiny traumas to the chest wall. You might also get the condition if you have had a lot of respiratory infections, bad coughing fits, or strain from exercise or other physical activity.
Tietze syndrome is commonly treated by resting your chest and ribcage. Your body requires time to heal the irritation inside your costochondral joint. Over-the-counter NSAIDs can lower your pain and decrease swelling. Talk to your provider previously taking NSAIDs for more than 10 days in a row.
Tietze syndrome is an infrequent, inflammatory disorder characterized by chest pain and swelling of the cartilage of one or more of the upper ribs (costochondral junction), specifically where the ribs attach to the breastbone (sternum). The onset of pain may be gradual or sudden and may spread to harm the arms and/or shoulders.
Diagnosis of Tietze’s syndrome is based on physical examination (an increase of palpation tenderness in the affected joint), laboratory tests (an increase of inflammatory parameters), and imaging studies (USG, MRI).
Tietze syndrome is a self-limiting disease with the best prognosis. Most patients report complete resolution of symptoms within 1 to 2 weeks with conservative management, yet there have been reports of the characteristic swelling lasting for up to one year. Reoccurrences are also possible.
Radiographic features
bone marrow edema in the subchondral bone. intense gadolinium enhancement in the parts of thickened cartilage, in the subchondral bone marrow, and/or in the capsule and ligaments.
Primary care doctors, involving family medicine doctors, general practitioners, and internists, as well as rheumatologists (medical specialists in musculoskeletal disease and systemic autoimmune conditions) & orthopedists (medical specialists in disorders of the musculoskeletal system).
Physiotherapy for Tietze’s syndrome may include breathing exercises and electrotherapy such as ultrasound and cryotherapy (ice). You may be provided with other strengthening and stretching exercises and soft tissue massage.