Superior Rectus Palsy
Table of Contents
What is Superior rectus palsy?
Superior rectus palsy is a disorder associated with dysfunction of the cranial nerve 3rd (oculomotor nerve), which is responsible for causing contraction of the superior rectus muscle’s to perform the primary action of elevating the eye, causing the cornea to roll superiorly (i.e., turn upward).
The inability of an eye to turn upward results in convergent strabismus or esotropia of which the primary symptom is diplopia (commonly known as double vision) in which the two images appear side-by-side.
Introduction of superior rectus muscles:
The superior rectus muscle is a muscle in orbit in the eyes. It is one of the extraocular muscles. It is innervated by the superior division of the oculomotor nerve the 3rd nerve. In the primary position looking straight ahead, its primary function is elevation, although it also contributes to intorsion and adduction action. It is associated with many medical conditions and might be weak, paralyzed, overreactive, or even congenitally absent in many people.
Origin and insertion of superior rectus muscles.
- Common tendinous ring of Zinn (Annulus tendinous communis).
- Superior rectus muscles (Musculus rectus superior).
- Common tendinous ring (of Zinn).
- Anulus tendineus communis.
- Synonyms: Annulus of Zinn, Anuluar tendinous ring.
What is the function of the superior rectus muscle?
The superior rectus muscles elevate, adduct, and asses in tort (rotate upward) the eye. The superior rectus muscles have a primary action of elevating the eye, causing the cornea to move superiorly. The superior rectus muscles originate from the annulus of Zinn and course anteriorly and superiorly over the globe, making an angle of 23 degrees with the visual axis in the eyes.
What are the symptoms of superior rectus palsy?
- common features of superior rectus palsy include the Sudden onset of horizontal double vision in the eyes, which is worse when the patient looks to the affected side.
- Limited upward movement of the affected eye. Convergent strabismus is large when the patient tries to look at an object in the distance.
- The inability of an eye to turn upward results in convergent strabismus or esotropia of which the primary symptom is diplopia (commonly known as double vision in the eyes).
- Double vision: Double vision or diplopia when looking upwards is the most common symptom of superior rectus palsy. The patient might notice this vision impairment when both eyes are open or when the patient is looking at something in the distance. Sometimes, double vision worsens when looking in the direction of the damaged eye. It is also possible to have superior rectus palsy without double vision.
- Poor eye alignment or strabismus: Also called crossed eyes, poor eye alignment is when the patient eyes do not look in the same direction at the same time.
- Head movement to maintain vision: Sometimes, individuals with superior palsy might make a constant turning motion with their heads in order to reduce their double vision.
Double vision problems and strabismus are typical with superior rectus palsy. But you might have other symptoms.
- Other symptoms may include:
- headache
- nausea
- vomiting
- papilledema or swelling of the optic nerve
- vision loss
- hearing loss
When superior rectus palsy occurs without other symptoms, it is known as isolated superior rectus palsy. The addition of other symptoms might suggest the involvement of more than just the 3rd nerve.
What are the causes of superior rectus palsy?
There are several causes of superior rectus palsy. The condition could affect a person from birth. This is sometimes due to an injury to the 3rd cranial nerve during the time of labor or delivery. Various circumstances and illnesses could also cause the disorder. This involves a head injury or skull fracture that damages the superior rectus. The disorder might also develop as a result of inflammation in the third cranial nerve. But sometimes the cause of superior rectus palsy is unknown.
Conditions known to cause superior rectus palsy damage or inflammation could include:
- head injury
- skull fracture
- injury during birth
- stroke
- brain aneurysm
- infection, known as Lyme disease, syphilis, tuberculosis, or meningitis
- inflammatory lesions, known as sarcoidosis or lupus
- abnormal growth or brain tumor of tissue in the brain
- diabetic neuropathy
- multiple sclerosis
- injury during a procedure, known as spinal anesthesia or postlumbar puncture
- cavernous sinus thrombosis, a condition caused by a blood clot behind the patient’s eye sockets
- mastoiditis, an infection in the bone behind the ear area.
- temporal arteritis is inflammation of the blood vessels around your scalp
The most common cause of superior rectus palsy in children is trauma, such as an accident and a head injury. In adults, the more common cause is stroke.
What are the possible complications of third nerve palsy?
superior rectus muscle palsy itself does not usually cause complications. But some of the possible causes of superior rectus palsy might have complications. Like any procedure, surgery for superior rectus palsy carries a risk of complications further in superior rectus palsy.
Key points about superior rectus palsy
Superior rectus palsy worsens when the third cranial nerve is damaged or does not work right. This causes problems with eye movement. The affected eye might not be able to move upward normally.
Sometimes, only the third cranial nerve has problems. But issues in other parts of the body could worsen, too. There are some other possible causes of superior rectus palsy. In children, trauma is one of the most common causes of superior rectus palsy. Treatment for superior rectus palsy depends on its cause and its symptoms.
Symptoms of superior rectus palsy often go away and the movement of the eye improves within several months. If the symptoms do not completely go away of superior rectus palsy, you might need other treatments and possibly surgery for the superior rectus palsy.
What is the diagnosis of superior rectus palsy?
Your doctor will probably prescribe you brain imaging tests because the nerve often becomes compressed as it leaves the brain. Brain imaging is also vital to make sure a brain tumor is not causing symptoms. Possible imaging tests involve computed tomography (CT) and magnetic resonance imaging (MRI).
Differential diagnosis of superior rectus palsy?
Differential diagnosis is rarely difficult in adults. In starting is typically sudden with symptoms of the horizontal side of diplopia. Limitations of the eye movements are confined to the superior of the affected eye or abduction of both eyes if bilateral and the size of the resulting convergent squint or esotropia is always greater on distance fixation – where the lateral recti muscles are more active than on near fixation – where the medial recti are dominant. upward movement limitations that mimic superior rectus palsy might result secondary to surgery, trauma, or as a result of other conditions known as myasthenia gravis or thyroid eye conditions.
In the child, differential diagnosis is more difficult because of the issues inherent in getting infants to cooperate with a full-eye motion investigation. Possible alternative diagnoses for an abduction deficit would include:
- Mobius syndrome – a rare congenital disease in which both VIth and VIIth nerves are bilaterally affected giving rise to a typically ‘expressionless’ face.
- Duane syndrome – A condition in which both abduction and adduction are affected arising as a result of limited innervation of the lateral rectus by branches from the 3rd oculomotor cranial nerve.
- Cross fixation- which develops in the existence of infantile esotropia or nystagmus blockage syndrome and results in habitual weakness of lateral recti muscles.
- Iatrogenic injury- Abducens nerve palsy is also called as occurs with halo orthosis placement. The resultant palsy is identified through loss of the lateral side of gaze after application of the orthosis and is the most common cranial nerve injury associated with this device.
Treatment of superior rectus palsy.
Physiotherapy treatment of superior rectus palsy.
Blinking exercises
It is like a rest for your eyes it asses to keep them fresh and focused for a longer time. Blinking improves symptoms of digital eyes strain, dry eyes, and blinking habits, a ten-second blinking exercise every 20 minutes would be with the asses.
Eye movement slowly moves your eyes up and down the side and repeat three times then again move your eyes slowly from right to left side and repeat three times then rest the eyes.
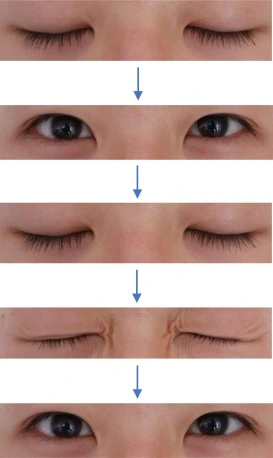
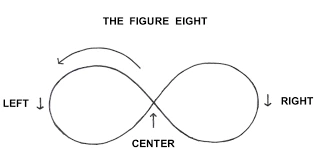
Figure-Eight-Improved-Vision
The figure of 8, is another exercise for eye movement, imagine there is a large figure of 8 away 8-9 feet from you, then move the eye in the direction of this infinity loop for about 20 to 30 seconds then switch the direction.
Focus change, hold your finger a few inches away from your eyes and focus the gaze on it then focus on another thing away from you, now return the gaze to your finger.
Pencil pushups
The patient holds a pencil or the patient’s thumb on the outstretched arm midway between the eyes, instruct the patient to try to keep a single picture of the pencil while slowly moving the pencil toward the nose till it is not possible to see the pencil in a single picture anymore, now ask the patient to move it slowly away to the closest point where there is a single image of pencil achieved—this exercise asses patients with symptomatic convergence insufficiency for superior rectus palsy.

Brock’s string is shown to improve convergence and eye coordination.
Effect of superior rectus palsy. Digital eye strain, as in people who work on a computer for a long time, might cause dry eyes, eye strain, blurred vision, and headaches.

It increased light sensitivity.
A surgery that needs strengthening of the muscles for superior rectus palsy. Suppose there is a problem in focusing your eyes to read. Convergence insufficiency.
surgical treatment of superior rectus palsy.
Superior oblique palsy known as an incidental finding in a patient without torticollis or symptoms does not require any treatment.
Prisms have a limited role in the management of superior rectus palsy and their role is limited to
• Very small comitant deviations, usually vascular
• Non-surgical candidates.
Most patients presenting to the ophthalmologist with superior rectus palsy do so because of troubling symptoms and are usually surgical candidates.
In the presence of superior rectus palsy, the preferred pro- cedure is a Knapp transposition. Knapp reported in 15 patients for whom correction of hypotropia ranged from 21 to 55 PD, with a mean of 38 PD. Good results are obtained in 14 of 15 patients. Other authors have found similar rates of correction (4-9).
FAQ
The most known symptom of superior rectus nerve palsy is double vision when both eyes are open. This is more known when looking at a distant side or when looking in the direction of the involved eye. But not everyone with superior rectus palsy has this manifestation. The eyes might also be out of alignment symptom known as strabismus.
The palsy of the 3rd cranial nerve damages the capacity to turn the eye upward side. third cranial nerve palsy has some causes, involving trauma to small blood vessels by diabetes, but the cause is frequently unknown. The involved eye cannot turn completely upward and might turn normal when a person looks straight forward.
emotional pressure is an unusual cause of vasculopathy cranial nerve palsy. Furthermore, we can see 112 and 91 patients of vasculopathy 6th and 3rd nerve palsy, lastly in which pressure wasn’t an obvious factor.
In some individuals, 3rd cranial nerve palsy decides once the underlying disease is treated. Treatment of inflammation, infection, or tumor when present might result in progress. Idiopathic palsy and ischemic palsy generally decrease within two months.
Yes, Depends upon the cause and severityt of the condition, in Normal condition Regular Treatment might be required, and the disease might disappear within two months. In an analysis of 213 patients with this disease, 78.4% healed with proper treatment. Of those who did not recover, 40% had severe underlying disease.



One Comment