Head Injury
Table of Contents
What is a Head injury?
- Head injuries are damage to the scalp, skull, or brain, & one of the most common causes of disability and death in adults.
- The injury can be as mild as a bump, bruise, or cut on the head, or can be moderate to severe in nature due to a concussion, deep cut, fractured skull bone & open wound.
- An open, or penetrating, head injury means you were hit with an object that broke the skull and entered the brain, or from internal bleeding and damage to the brain.
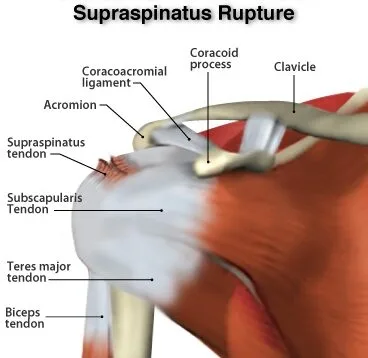
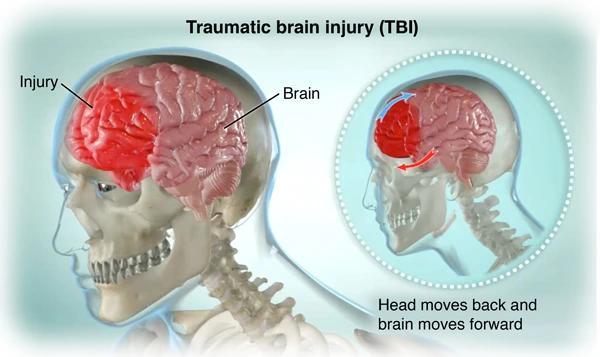
- Head injuries are also commonly by as brain injury, or traumatic brain injury (TBI), depending on the head trauma.
- traumatic brain injury (TBI) is commonly referred to as a head injury that involves damage to the brain causing difficulties with communication & movement such as poor coordination and balance.
- A head injury is considered an acceptable risk when engaging in sports and other activities. They can lead to mental impairment, permanent disability, and even death.
- the describes a vast array of injuries that occur to the skull, brain, scalp, & underlying tissue, and blood vessels in the head.
- Head injuries are rising about 1.7 million people have a TBI per year.
- Physiotherapy can help in their physical recovery following a brain injury.
Types of Head Injuries
There are different types of head injuries.
- Concussion
- Intracranial hematoma(ICH)
- Contusion or intracerebral hematoma
- Epidural hematoma
- Subdural hematoma
- Diffuse axonal injury (DAI)
- Skull fracture:
- Linear skull fracture
- Depressed skull fracture
- Diastatic skull fracture
- Basilar skull fracture
- Concussion:- The most common type of head injury. the brain is shaken, or the most common type of traumatic brain injury. a concussion is an injury to the head area that may cause loss of awareness or alertness for a few minutes up to a few hours after the traumatic event. It can range from mild to severe. An impact on the body can create enough force on the brain.
- Intracranial hematoma (ICH):- There are several types of ICH, or blood clots & bleeding under the skull in the brain. intracranial hematoma causes bleeding and swelling inside the brain area. Intracranial hematoma is a collection, or clotting, of blood outside the blood vessels.
- Contusion:- A bruise on the actual brain called a contusion. It can cause bleeding & swelling inside the brain around the area where the head was struck. Bruises may do with cranium fractures or other blood clots analogous to a subdural or epidural hematoma. Bleeding that occurs inside the brain itself (also called intraparenchymal hemorrhage) can sometimes do spontaneously. When trauma isn’t the cause, the most common causes are long-standing, high blood pressure in aged adults, bleeding disorders in either children or adults, or the use of specifics that cause blood thinning or certain illicit medicines.
- Epidural hematoma: Epidural hematomas occur when a blood clot forms underneath the cranium, but on top of the dura, the tough covering that surrounds the brain. They generally come from a tear in an artery that runs just under the cranium called the middle meningeal artery. Epidural hematomas are usually associated with a cranium fracture.
- Subdural hematoma: Subdural hematomas occur when a blood clot forms underneath the cranium and underneath the dura, but outside of the brain. These can form from a tear in the modes that go from the brain to the dura, or from a cut on the brain itself. They’re occasionally, but not always, associated with a cranium fracture.
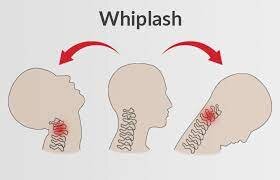
- Diffuse axonal injury (DAI): These injuries are fairly common and are generally caused by shaking of the brain back and forth, which can be in car accidents, falls, or shaken baby syndrome. Diffuse injuries can be mild, analogous to a concussion, or maybe veritably severe, as in diffuse axonal injury (DAI). In DAI, the patient is generally in a coma for a prolonged period of time, with injury to numerous different parts of the brain.
- Skull fracture:- This type of fracture is a break in the cranium bone. The broken of bone can cut into the brain and cause bleeding and other types of injury.
- Linear skull fractures:- Very common type of skull fracture. In a linear fracture, there is a break in the bone, but it does not move the bone. The Patient may be observed in the hospital for a brief amount of time, and generally normal activities in a few days.
- Depressed skull fractures:- Depressed cranium fractures may be seen with or without a cut in the scalp. this fracture, Also the part of the skull is actually sunken in from the trauma. This type of skull fracture may require surgical depending, intervention on the severity, it helps correct the deformity.
- Diastatic skull fractures:- These are fractures along suture lines in the cranium. The sutures are the areas between the bones in the head when we are children. In this type of fracture, the normal suture lines are wide. These fractures are generally seen in newborns and older infants.
- Basilar skull fracture:- The most serious type of skull fracture. This type of fracture involves a break in the bone at the base of the cranium. This type of fracture constantly has bruises around their eyes and a bruise behind their observance.
What causes bruising and internal damage to the brain?
- There is a direct blow to the head, shaking of the child, or as seen in motor vehicle accidents, the bruising of the brain and damage to the internal tissue and blood vessels due to a medium called coup-contrecoup. A bruise directly related to trauma, at the point of impact, is called a coup lesion. As the brain jolts backward, it can hit the cranium on the opposite side and cause a bruise called a countercoup lesion. The jarring of the brain against the sides of the cranium can cause tearing of the internal filling, tissues, and blood vessels that may cause internal bleeding, bruising, or swelling of the brain.
What are the symptoms of a head injury?
In a head injury, many different symptoms present depending on its severity.
Mild head injury Symptoms include:
- Mild headache
- Some bleeding
- Bruising
- Feeling sick or nauseated
- Mild dizziness
Moderate head injury Symptoms include:
- Passing out for a short time
- Vomiting
- Memory problems
- A lasting headache
- Confusion or distraction
- Temporary changes in behavior
- Loss of balance
Severe head injury Symptoms include:
- Significant bleeding
- Weakness or numbness
- Difficulty speaking
- Problems with vision, taste, or smell
- Difficulty staying alert or awake
- Passing out and not waking up
- Bruises behind the ears
- Having a seizure
- Bleeding out of the Nose or Ears
Key symptoms of a concussion include:
- Confusion
- A headache
- Balance problems
- Dislike of noise or light
- Nausea
- Difficulty concentrating
- Feeling groggy
- Blurred vision
Children’s symptoms:
- A child with traumatic brain injury, you may observe:
- Change in eating or nursing habits
- Change in sleep habits
- Persistent crying and inability to be consoled
- Sad or depressed mood
- easy irritability
- Seizures
- Change in ability to pay attention
- Drowsiness
- Loss of interest in favorite activities
What causes a head injury?
- Common causes of head injury include:
- Accidents at the workplace, at home, while playing outdoor sports
- Falls
- Violence assault
- Traffic accidents
- Accidents at the workplace, home, playing outdoor sports:- Including soccer, boxing, football, baseball, lacrosse, skateboarding, hockey, and home activities.
- Falls:- Falls from bed, or downstairs, in the bath, and other falls are common causes of traumatic brain injury.
- Violence assault:- Gunshot wounds, domestic violence, and Shaken baby syndrome are traumatic brain injuries caused by a violent assault.
- Traffic accidents:- Involving cars, motorcycles, or bicycles.
- Most of these injuries are minor because the cranium protects the brain, but Some injuries are severe enough to require a stay in the hospital.
Risk factors
- Most people are at risk of traumatic brain injury include:-
- Children, especially newborns to 4-year-olds
- youthful grown-ups, especially those between ages 15 and 24
- Males in any age group
- Adults aged 60 and older
How to Prevent Head Injury?
- Follow these tips:-
- Seat belts and airbags
- Helmets
- Alcohol and drug use
- Pay attention to your surroundings
- Seat belts and airbags:- Always wear a seat belt in a motor vehicle and a small child should always sit in the back seat or booster seat that is applicable for his or her size and weight.
- Helmets:- Wear a helmet while riding a bicycle, motorcycle, snowmobile, or all-terrain vehicle, and also head protection when playing baseball or contact sports, skating, snowboarding, or riding a horse.
- Alcohol and drug use:- Don’t drive under the influence of alcohol or drugs.
- Pay attention to your surroundings:- Don’t drive, walk or cross the road while using your phone, tablet, or any smart device.
Preventing head injuries in children
- Follow these tips:-
- Install a safety gate at the top of a stairway
- Keep stairs clear of clutter
- Install window guards to prevent falls
- Put a non-slip mat in the shower or bathtub
- Use playgrounds that have shock-absorbing accouterments on the ground
- Make sure area rugs are secure
- Don’t let children play on sundecks or fire escapes
Clinical Rating System
- Glasgow coma scale
- Rappaport disability rating scale
Diagnosis
- Traumatic brain injuries may be emergencies, In the case of more-severe TBIs, consequences can worsen rapidly without treatment.
- Doctor responders need to assess the situation quickly following:-
- Glasgow Coma Scale
- Intracranial pressure monitor
- Imaging tests
- Computerized tomography (CT) scan,
- Magnetic resonance imaging (MRI)
- Glasgow Coma Scale:- This 15-point test helps a doctor, and the initial severity of a brain injury by checking a person’s ability to follow directions and move their eyes and limbs. Capacities are scored from three to 15 on the Glasgow Coma Scale. Advanced scores mean less severe injuries.
- Intracranial pressure examiner:- Tissue swelling from a traumatic brain injury can increase pressure inside the skull and cause additional damage to the brain. Doctors may insert a probe through the skull to cover this pressure.
- Imaging tests:-
- Computerized tomography (CT) scan:- This test is usually the first performed in an emergency for traumatic brain injury. A CT scan uses a series of X-rays to produce a detailed view of the brain. A CT scan can quickly visualize fractures and uncover evidence of bleeding in the brain, blood clots, contusions, and brain tissue swelling.
- Magnetic resonance imaging (MRI):- An MRI uses powerful radio waves & magnets to create a detailed view of the brain. This test may be used after the patient’s condition stabilizes, or if symptoms don’t improve soon after the injury.
Physical examination
- Glasgow coma scale
- Pupil size and response
- Signs of skull fracture
- Full neurological examination: Tone, Power, Sensation, and Reflexes
Treatment of Head Injury
- The treatment for head injuries depends on the severity and location of the injury. Mostly Mild injuries do not require treatment. still, you should know the signs and symptoms that require medical attention.
- still, call the ambulance immediately, If the head injury is severe.
- still, try to stop the bleeding by using a reek, or a clean cloth, If the injured person is bleeding.
- still, don’t touch or apply pressure on it, If the crack is open. Cover or wrap the crack with a clean piece of reek( bandage) rather.
- Still, help them to lean forward If the person is vomiting while sitting. However, roll their body to the side to help to choke, If the person is vomiting while lying down.
- still, instruct them not to move their head and neck, If the person is awake. This can help further damage their spine and brain.
- still, try to stabilize their body, If the person is unconscious and breathing.
- still, begin the process of CPR( cardiopulmonary reanimation), If the person is unconscious and not breathing.
- Treatment is personalized, depending on the extent of the condition and the presence of other injuries. If the patient has a severe head injury, may require monitoring for increased intracranial pressure inside the cranium. Since the brain is covered by the cranium, there is only a small quantum of room for it to swell. This causes pressure inside the cranium to increase, which can lead to brain damage.
The following treatment
- Medical Treatment
- Surgical Treatment
- Physiotherapy Treatment and Rehabilitation
Medical Treatment
- Medical can help treat symptoms of head injury and lower the risk of some conditions. Some medicals are useful immediately after a traumatic brain injury, while others treat symptoms and problems related to recovery from traumatic brain injury sometime after the initial injury. These medical treatments may include:-
- Anti-seizure drugs:- An anti-seizure drug may be given during the first week to avoid any additional brain damage caused by a seizure.
- Coma-inducing drugs:- Doctors sometimes use medicines to put people into temporary comas because a comatose brain needs lower oxygen to serve. This is helpful if blood vessels, compressed by increased pressure in the brain, are unfit to supply brain cells with normal quantities of nutrients and oxygen.
- Diuretics:- These medicines reduce the amount of fluid in tissues and increase urine output. Diuretics help reduce pressure inside the brain.
Surgical Treatment
- Surgical Treatment:- Emergency surgery may be demanded to minimize additional damage to brain tissues. Surgery may be used for the following problems:-
- Removing clotted blood:- Bleeding outside or within the brain can affect a collection of clotted blood that puts pressure on the brain and damages brain tissue.
- Repairing skull fractures:- Surgery may be demanded to repair severe skull fractures or to remove pieces of skull in the brain.
- Bleeding in the brain:- Head injuries that cause bleeding in the brain may demand surgery to stop the bleeding.
- Opening a window in the skull:– Surgery may be used to relieve pressure inside the cranium by draining accumulated cerebrospinal fluid or creating a window in the cranium that provides more room for swollen tissues.
Physiotherapy Treatment and Rehabilitation
- Physiotherapy Treatment: The patient was treated first in side lying on one side, then in supine lying, and then side lying on the other side. In side lying the patient was percussed well over the lateral costal and posterior basal areas. Thereafter the chest wall was firmly vibrated as the patient breathed out and the chest was suctioned during the period of expiration, through the tracheostomy tube. Passive movements of the arm and leg were carried out as fully as possible, but great difficulty was experienced due to the spasm. The passive movements of the arm were done to maintain the mobility of the chest wall as well as the mobility of the limb itself. In supine lying the patient was vibrated first in the lower coastal and then in the apical region, suctioning in between as well as at the end. When the patient was turned on to the other side, percussion, vibration, and suctioning were repeated, as well as passive movements of the arm and leg. As soon as the patient recovered consciousness he was taught to cough. When the above physiotherapy assessment was done by the writer, the chest was clear and the breathing was good. However, the passive movements of the arm and leg had not been entirely successful due to the difficulties caused by the hypertonia and potential flexor contractures developing in the left elbow, shoulder, and knee. The mobility of the spine was very poor.
- They may need to relearn introductory skills, such as walking or talking. The thing is to improve their capacities to perform daily activities. Very few people who have had a significant brain injury will bear rehabilitation. The type and duration of rehabilitation are different for everyone, depending on the inflexibility of the brain injury and what part of the brain was injured.
- Neurological Traumatic brain injury(TBI) physiotherapy can help:
- Improve balance and walking
- Increase ability to roll/move in bed/sit/stand
- Reduce muscle spasms, contractures, stiff joints, and associated pain
- Restoring muscle strength and joint stability
- Retrain normal patterns of movement
- Increase arm and leg function
- Increase energy levels
- Restoring the quality of life
- Reducing the risk of falls
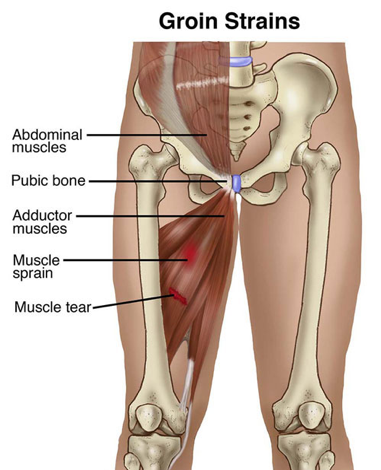
- The injuries sustained can frequently be severe and may take longer to recover from than other types of neurological conditions. the nature of the injury may have caused other physical problems similar to fractures and soft tissue damage, to occur alongside the brain injury. Improvements are frequently rapid-fire the immediate few weeks post-injury, followed by a slower period of recovery over the coming months into years.
- The maturity of a person’s recovery is achieved within the first 12 months post-injury, there’s substantiation to show that improvements can continue, given the applicable therapy and rehabilitation, for up to 10 years.
- During treatment sessions, our physiotherapists will lead you through a progressive program of functional exercises to increase your mobility and muscle control.
- Determined by the condition of the patient.
- Patient level of consciousness, alertness, and capability to comprehend as well as learn teaching skills.
- for practical purposes, patients are classified into the following two treatment purposes as
- Patient totally unconscious
- The patient has regained consciousness.
- Patient totally unconscious
- Respiratory care
- Preventing contractures and deformity
- Prevention and treatment of pressure sores
- Sensory stimulation
- Respiratory care
- The need for chest care is directly proportional to the extent of unconsciousness.
- Generally, chest physiotherapy is given every 4 to 6 hours. This is necessary to maintain bronchial hygiene.
- Proper positioning of the patient with regular suctioning and nebulization enables the patient to have a relatively clear lung.
- Head low position should never be given to the head injury case as it may cause a severe increase in the intracranial pressure that may prove to be dangerous.
- Preventing contracture and deformity
- Passive movements should be given to the patient for all the joints including all the movements at that particular joint passive movements may be repeated 8 to 12 times.
- Gentle rhythmic stretching is veritably essential especially for bi-articular muscles as they come veritably prone to develop tightness.
- The use of applicable splints and proper positioning is also desirable to help the chances of the patient developing any contracture.
- The patient should be kept clean and the clothes should be regularly changed.
- Prevention and treatment of pressure sores
- The patient’s position should be changed from supine to side lying on either side every 2 to 3 hours at least.
- The patient should be made to lie on a water bed or air bed which helps in evenly distributing the weight throughout the body, therefore, relieving some pressure.
- Regular massage of pressure-prone areas helps in increasing the circulation of these areas preventing pressure sores.
- Regular sponge bath helps in maintaining the proper hygienic condition of the patient’s skin.
- Sensory stimulation
- Auditory,
- Tactile and
- Proprioceptive stimulation
- Respiratory care
- Patients have regained their consciousness
- The patient is conscious, and active participation of the patient should be encouraged which in turn will speed up the rehabilitation process.
- Improve alertness or arousal through sensory stimulation
- Prevention of spasticity
- Maximize the patient’s functional capacity
- Development of high-level skillful functioning
- Improve alertness or arousal through sensory stimulation
- The main aim is to stimulate the reticular activating system by making the patient sit or indeed stand on the tilt table.
- The therapist should provide tactile, visual, auditory, and proprioceptive stimulation to the patient that will send facilitator signals to the brain and will enable the alert response to incite.
- Audile stimulation can be given by speaking to the patient during the course of treatment.
- Visual stimulation is given by showing familiar faces, objects, or movements in the visual field of the case.
- Tactile stimulation is provided by the therapist’s touch for carrying out multifarious functional tasks. The touch of the patient also stimulates the receptors in the muscles and can be used for inhibiting the contraction of muscles.
- Proprioceptive stimulation by giving traction and approximation at joint structures is veritably helpful in stimulating the arousal response in the patient.
- Prevention of spasticity
- Generally passive movement
- Gradual rhythmic sustained stretch
- Proper positioning
- Maximize the patient’s functional capacity
- The main aim of this management is to:-
- Improve the ROM
- Improve the control of voluntary movement
- strengthening paretic muscles
- Improve the coordination
- Balance and educate various safety measures which will enable the patient to return back to the community
- Neuromuscular training
- Activities like:-
- Bridging
- Prone on elbow
- Side-lying o sitting
- Sitting
- Kneeling
- Half kneeling
- Standing
- Walking
- The use of a vestibular ball while training the patient for crawling, bridging, and sitting balance helps in erecting the proprioceptive stimulation and teaches proper control to the patient.
- Which needs to be mastered by the patient so that he learns the actual activity using normal movement combinations and performs it.
- Repetition of activities
- Functional electrical stimulation
- Reversing tasks: For instance, lowering a glass of water on the table may help the patient in getting the glass close to the mouth by perfecting motor control of the biceps during compression.
- The main aim of this management is to:-
- Development of high-level skillful functioning
- The safety awareness of the patient needs to be bettered because he is already in the ambulatory stage.
- Balance and postural control training are veritably essential some patients may have good balance and postural control during normal walking but will have problems while trying to perform speedy conduct.
- The therapist should encourage those components of the activities that best address the deficits in the patient and plan out pleasurable activities that give specific training for the deficits in balance, gait, and upper extremity functions.
Rehabilitation specialists may include
- Physiatrist:- A doctor trained in physical drugs and rehabilitation, who oversees the entire rehabilitation process, manages medical rehabilitation problems and prescribes drugs as demanded.
- Occupational therapist:- This therapy helps the person learn, relearn or improve skills to perform everyday activities.
- Speech and language therapist:- This therapy helps the person improve communication skills and use assistive communication devices if necessary.
- Traumatic brain injury nurse specialist:- This helps coordinate care and educates the family about the injury and recovery process.
- Recreational therapist:- This assists with time management and leisure activities.
Lifelong thought for a person with a head injury
- The key is to promote a safe environment for children and adults and to help head injuries from being in the first place. The use of seat belts when riding in the car and a helmet in riding a motorbike, bicycle, in-line skating, and skateboarding may cover the head from sustaining severe injuries.
- Persons who suffer a severe brain injury may lose muscle strength, motor skills, speech, vision, hearing, or taste function, depending on the brain region involved and the inflexibility of brain damage. Long- or short-term changes in personality or behavior may also do. These persons require long-term medical and rehabilitative management.
- The extent of the patient’s recovery depends on the type and severity of the injury and other medical problems that may be present. It is important to concentrate on maximizing the person’s capabilities at home and in the community. Positive underpinning will encourage the patient to strengthen his/her tone of regard and promote independence.
FAQ
The most common short-term difficulties associated with TBIs involve cognitive impairment, difficulties with sensory processing and communication, instant seizures, hydrocephalus, cerebrospinal fluid (CSF) leakage, vascular or cranial nerve damage, tinnitus, organ default, and polytrauma.
You can hold a cold compress to their head – try a bag of ice or frozen peas banded in a tea tissue. Seek instant medical advice if symptoms similar to mild dizziness and a headache get worse.
feel a provider within 1 to 2 days of a significant head injury with ongoing symptoms, indeed if emergency care isn’t required. Seek emergency medical immersion if your child experiences: Unconsciousness, distraction, or disorientation after a head injury.
After having a concussion, careful monitoring is needed. This is generally for 48 hours. This is because the symptoms of concussion could also be symptoms of a more serious condition, similar to subdural hematoma – bleeding between the skull and the brain.
An untreated head injury can lead to unrecoverable brain damage due to brain cell loss or death that instant medical care may have prevented. complicated brain damage can lead to cognitive and motor function disability or even death.




18 Comments