Traumatic Brain Injury
Table of Contents
What is The Traumatic Brain Injury?
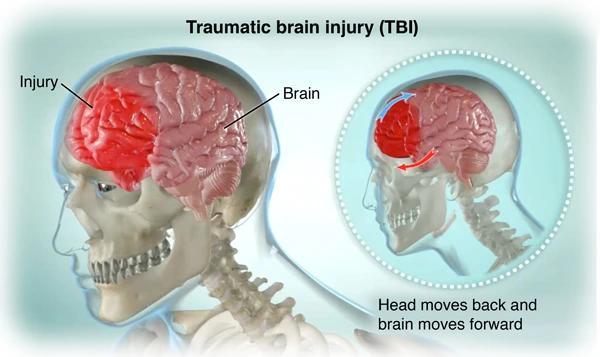
- Traumatic brain injury(TBI) commonly results from a violent blow to the head or body. An object that is targeted toward the head or brain, such as a bullet or shattered piece of skull, also can cause traumatic brain injury(TBI).
- Mild traumatic brain injury might affect your brain cells temporarily. Many serious traumatic brain injuries can result in bruising, torn tissues, bleeding, and other physical damage to the brain. This injury can result in long-term death.
- Few injuries are considered primary, meaning the damage is immediate.
- Other outcomes of traumatic brain injury(TBI) can be secondary, meaning they can occur gradually over the course of hours, or days, or appear weeks later.
- These secondary brain injuries are the result of reactive processes that do so after the initial head trauma.
Two broad types of Traumatic brain injury(TBI): Penetrating and non-penetrating
- Penetrating Traumatic brain injury(open TBI) happens when an object pierces the skull (e.g., a bullet, bone fragment, or by a weapon such as a hammer or a knife) and enters the brain tissue. Penetrating Traumatic brain injury normally damages only part of the brain.
- Non-penetrating Traumatic brain injury(closed head injury or blunt TBI) is caused by an external force strong enough to move the brain within the skull. Causes involve falls, sports injuries, motor vehicle crashes, blast injuries, or being struck by an object. Few accidents such as explosions, natural disasters, or other extreme events can cause both penetrating and non-penetrating Traumatic brain injury in the same person.
What are the types of traumatic brain injuries?
The severity of the head injury is determined by several different factors, such as loss of consciousness, some neurological symptoms that came at the time of the injury, loss of memory for the injury and time compassing it, and abnormalities on head CT or brain MRI.
There are different types of traumatic brain injuries(TBIs):
- Mild concussion (mTBI):- Concussions are a very common type of traumatic brain injury. Three out of four traumatic brain injuries every year are concussions. These mild traumatic brain injuries can involve brief alterations of consciousness also as feeling “dazed” or loss of consciousness for less than 30 minutes. People who have a mild traumatic brain injury can experience confusion for about one day, which is different from difficulties with attention or memory.
- Moderate traumatic brain injuries:– this type of head damage is associated with loss of consciousness for over 30 minutes but less than one day. Confusion can last for over one week.
- Severe traumatic brain injuries:– individuals with this type of head damage lose consciousness for over one full day. These damages are typically associated with changes in head CT or brain MRI.
- Uncomplicated traumatic brain injuries:– Head CT or brain MRI is normal, regardless of mild, moderate, or severe grade.
- Complicated traumatic brain injuries:– Head CT or brain MRI shows changes, such as bleeding.
- Closed:- Most traumatic brain injuries are closed. A closed traumatic brain injury means an outside force causes a blow to the head that did not penetrate the skull. This impact damages the brain, causing it to swell.
- Open:- Healthcare providers might call open traumatic brain injuries penetrating traumatic brain injuries. This damage occurs when a bullet, knife, or something else goes through the skull. If the thing goes into the brain, it directly injures brain tissue.
- Nontraumatic:- Also known as a hypoxic or anoxic brain injury. Few traumatic brain injuries aren’t from trauma. They can perform from strokes, seizures, and events like choking and near-fatal drownings. These things can deprive the brain of oxygen (cerebral hypoxia).
Signs and symptoms of Traumatic Brain Injury
Seek immediate medical attention if you experience any of the following Physical, Behavioral/Cognitive, or Sensory symptoms, especially after a TBI:
Physical
- Headache
- Convulsions or seizures
- Blurred or double vision
- Unequal eye pupil size or dilation
- Clear fluids draining from the ears
- Nausea and vomiting
- The new neurologic deficit, such as slurred speech; weakness of arms, legs, or face; loss of balance
Behavioral/Cognitive
- Loss of change in consciousness anywhere from a few seconds to a few hours
- Reduce the level of consciousness (e.g., hard to awaken)
- Mild to profound confusion or disorientation
- Problems remembering, concentrating, or making decisions
- Changes in sleep patterns (e.g., difficulty falling, sleeping more, or staying asleep); inability to waken from sleep
- Frustration, irritability
Perception/sensation
- Dizziness, vertigo, Light-headedness, or loss of coordination or balance
- Blurred vision
- Hearing problems, also as ringing in the ears
- Bad taste in the mouth
- Sensitivity to light or sound
- Agitation, combativeness, Mood changes or swings, or other unusual behavior
- Feeling anxious or depressed
- Fatigue or drowsiness; a lack of energy and motivation
Headache, dizziness, confusion, and fatigue tend to start immediately after traumatic brain injury but resolve over time. Emotional symptoms suchlike as frustration and irritability tend to develop during recovery.
Traumatic Brain Injury in Children
Children might be unable to let some know that they feel different following a blow to the head. A child with a Traumatic brain injury might display the following signs or symptoms:
- Changes in eating or nursing habits
- Persistent crying, crankiness, or irritability; inability to be consoled
- Changes in ability to pay attention
- Lack of interest in a favorite activity or toy
- Changes in sleep patterns
- Seizures
- Sadness or depression
- Loss of skill, as well as a toilet training
- Loss of balance or unsteady walking
- Vomiting
Effects on Consciousness
A Traumatic brain injury(TBI) can cause problems with awareness, consciousness, and responsiveness. Commonly, there are 4 abnormal states that can result from a severe Traumatic brain injury(TBI):
- Minimally conscious state: People with severely altered consciousness who still display some evidence of self-awareness or awareness of one’s environment (such as following simple commands, and yes/no responses).
- Vegetative state: A result of widespread damage to the brain, some people in a vegetative state are unconscious and unaware of their surroundings. Still, they can have periods of unresponsive alertness and might groan, move, or show reflex responses. If this state lasts longer than some weeks, it is referred to as a persistent vegetative state.
- Coma: A person in a coma is unaware, unconscious, and unable to respond to external stimuli suchlike as pain or light. A coma normally lasts a few days or weeks after which the person might regain consciousness, die, or move into a vegetative state.
- Brain death: The lack of measurable brain activity and function after an extended period of time is called brain death and might be confirmed by studies that show no blood flow to the brain.
How Traumatic brain injury(TBI) affects the brain
Traumatic brain injury-related damage can be confined to one area of the brain, known as a focal injury, or it can so over a more widespread area, known as a diffuse injury. The type of injury also affects the brain is damaged.
Primary effects on the brain include many types of bleeding and tearing forces that injure nerve fibers and cause inflammation, metabolic changes, and brain swelling.
- Diffuse axonal injury (DAI), one of the very common types of brain injuries, refers to widespread damage to the brain’s white matter. White matter is composed of bundles of axons (the projections of nerve cells that carry electrical impulses and connect many areas of the brain to one another). Diffuse axonal injury(DAI) commonly results from rotational forces or sudden forceful stopping that stretches or tears these axon bundles. This damage normally occurs in auto accidents, falls, or sports injuries. Diffuse axonal injury(DAI) can disrupt and break down communication among nerve cells in the brain. It also leads to the release of brain chemicals that can cause some damage. The brain damage might be temporary or permanent and recovery can be prolonged.
- A concussion is a type of mild Traumatic brain injury(TBI) that might be considered a temporary injury to the brain but could take minutes to several months to heal. A concussion can be caused by a number of things involving a bump, blow to the head, sports injury or fall, motor vehicle accident, weapons blast, or a rapid acceleration or deceleration of the brain within the skull, suchlike as the person having been violently shaken. The individual either suddenly loses consciousness or has suddenly altered the state of awareness or consciousness. A second concussion closely following the first one causes some damage to the brain the so-called “second hit” phenomenon and can lead to permanent damage or even death in a few instances. The post-concussion syndrome includes symptoms that last for weeks or longer.
- Hematomas are bleeding in and around the brain caused by a rupture of a blood vessel. Many different types of hematomas form depending on where the blood collects relative to the meninges, the protective membranes surrounding the brain, which consist of three layers: dura mater (outermost), pia mater (innermost), and arachnoid mater (middle).
- Epidural hematomas include bleeding into the area between the skull and the dura mater. These can so within minutes to hours after damage to a brain vessel under the skull and are particularly dangerous.
- Subdural hematomas include bleeding between the dura and the arachnoid mater, and, like epidural hematomas, exert pressure on the outside of the brain. They are most common in the elderly after a fall.
- Subarachnoid hemorrhage is bleeding between the pia mater(innermost) and the arachnoid mater(middle).
- Bleeding into the brain is called an intracerebral hematoma and damages the surrounding tissue.
- Contusions are bruising or swelling of the brain that so when very small blood vessels bleed into brain tissue. Contusions can so directly under the impact site (a coup injury) or, more oft, on the complete opposite side of the brain from the impact (a contrecoup injury). They can appear after a prolongation of hours to a day. Coup and contrecoup lesions normally so when the head abruptly decelerates, which causes the brain to bounce back and forth within the skull (suchlike as in a high-speed car crash or in shaken baby syndrome).
- Skull fractures are breaks or cracks in one or more of the bones that form the Cranium. They are a result of blunt force trauma and can cause damage to the blood vessels, membranes, and brain under the fracture. One main benefit of helmets is to prevent Cranium fractures.
- Chronic traumatic encephalopathy (CTE) is a progressive neurological disorder associated with symptoms that might involve problems with understanding, thinking, and communicating; motor disorders (affecting movement); problems with impulse depression and control; confusion; and irritability. Chronic traumatic encephalopathy is so in those with extraordinary exposure to multiple blows to the head and as a delayed consequence after many more years. Studies of retired boxers have shown that repeated blows to the head can cause issues involving memory problems, tremors, lack of coordination, and dementia. Recent studies have demonstrated rare cases of Chronic traumatic encephalopathy in further sports with repetitive mild head impacts (e.g., soccer, wrestling, football).
- A single, severe Traumatic brain injury also may lead to a disorder called post-traumatic dementia (PTD), which may be progressive and share few features with Chronic traumatic encephalopathy. Studies assessing patterns among large populations of people with Traumatic brain injury indicate that moderate or severe Traumatic brain injury in early or mid-life may be associated with an increased risk of dementia later in life.
Examples of secondary damage:
- Hemorrhagic progression of a contusion (HPC) is an injury that so when an initial contusion from the primary injury continues to bleed in and around the brain and expand over time. This creates a new or larger lesion an area of tissue that has been injured through injury or disease. This increased exposure to blood, which is toxic to brain cells, leads to swelling and more brain cell loss.
- A breakdown in the blood-brain wall refers to the disruption of the network of cells that controls the movement of cells and molecules between the blood and fluid that surrounds the brain’s nerve cells. Once the blood-brain wall is disrupted, blood, plasma proteins, and other foreign substances leak into the space between neurons in the brain and activate a chain reaction that causes brain swelling. It also causes multiple biological systems to come into overdrive, including inflammatory responses which can be dangerous to the body if they continue for an extended period of time. It also permits the release of neurotransmitters, or chemicals used by brain cells to communicate, which can injure or kill nerve cells when depleted or over-expressed.
- Increased intracranial pressure is normally caused by brain swelling inside the confined area of the skull as a result of the injury. This pressure can injure brain tissue and can prevent blood flow to the brain and deprive it of the oxygen it needs to function.
- Other secondary damage can be caused by infections to the brain, low blood pressure or oxygen flow as a result of the damage, hydrocephalus, and seizures.
Cause of Traumatic Brain Injury
Adults aged 60 and older are at the greatest risk of being hospitalized and dying from a traumatic brain injury(TBI), very commonly from a fall. In every age group, serious traumatic brain injury(TBI) rates are higher for men than for women. Men are also likely to be hospitalized and are nearly three times more likely to die from a traumatic brain injury(TBI) than women.
The leading causes of traumatic brain injury involve:
- Falls: According to data from the Centers for Disease Control and Prevention (CDC), falls are the most common cause of traumatic brain injury(TBI) and occur most frequently among the youngest and oldest age groups.
- Blunt trauma accidents: Accidents that involve being struck by or against an object, particularly sports-related injuries, are a major cause of traumatic brain injury(TBI).
- Vehicle-related injuries: Pedestrian-involved accidents, as well as accidents involving motor vehicles and bicycles, are the third most common cause of traumatic brain injury(TBI).
- Assaults/violence Assaults: Abuse-related traumatic brain injury(TBI) are head injuries that result from shaken baby syndrome, and gunshot wounds to the head. Traumatic brain injury(TBI) related deaths in children aged 3 and younger are most likely the results of the assault.
- Explosions/blasts: Traumatic brain injury(TBI) caused by blast trauma from roadside bombs became the most common injury to service members in military conflicts. The majority of these traumatic brain injuries(TBI) are classified as mild head injuries.
Risk factors
The people most at risk of traumatic brain injury involve:
- Children, especially newborns to 4-year-olds
- Young adults, especially those between ages 14 and 25
- Adults age 60 and older
- Males in any age group
How is a traumatic brain injury (TBI) diagnosed?
Diagnosing traumatic brain injury(TBI)
- All traumatic brain injuries (TBIs) require immediate assessment by a professional who has experience assessing head injuries. A neurological exam will result from motor and sensitive skills and test hearing and speech, coordination and balance, mental status, and changes in mood or behavior, among other abilities. Screening tools for trainers and athletic trainers can identify the most concerning concussions for medical evaluation.
- Initial assessments may rely on standardized instruments similar to the Acute Concussion Evaluation (ACE) form from the Centers for Disease Control and Prevention (CDC) or the Sports Concussion Assessment Tool 2, which gives a systematic way to assess a person who has suffered a mild traumatic brain injury(TBI). Reviewers collect information about the characteristics of the injury, the presence of amnesia (loss of memory) and seizures, as well as the presence of physical, cognitive, emotional, and sleep-related symptoms.
- Acute Concussion Evaluation (ACE) is also used to track symptom recovery over time. It also takes into account risk factors (involving concussion, headache, and psychiatric history) that can impact how long it takes to recover from a traumatic brain injury(TBI).
- Diagnostic imaging. When important, medical providers will use brain scans to estimate the extent of the primary brain injuries and determine if surgery will be demanded to help repair any damage to the brain. The need for imaging is based on a physical exam by a doctor and a person’s symptoms.
- Computed tomography (CT) is the very commonly used imaging technology to assess people with suspected moderate to severe Traumatic brain injury(TBI). Computed tomography(CT) creates a two-dimensional picture of organs, bones, and tissues and can show a skull fracture or any brain bruising, swelling, or bleeding.
- Magnetic resonance imaging (MRI) produces thorough images of body tissue. It might be used after the initial assessment and treatment as it is a more sensitive test and picks up subtle changes in the brain that the Computed tomography(CT) scan may have missed.
- Significant advances have been made in the last decade to image milder Traumatic brain injury(TBI) damage. For example, diffusion tensor imaging can image white matter tracts, more sensitive tests like fluid-attenuated inversion recovery can detect small areas of damage, and susceptibility-weighted imaging more sensitively identifies bleeding.
- Despite these improvements, presently available imaging technologies, blood tests, and other measures remain deficient for detecting these changes in a way that can help diagnose mild concussive injuries.
- Neuropsychological exams to gauge brain functioning are oft used along with imaging in people who have suffered mild Traumatic brain injury(TBI). Such tests involve performing specific cognitive tasks that help assess memory, concentration, executive functioning, information processing, response time, and problem-solving.
- The Glasgow Coma Scale is a very widely used tool for assessing the level of consciousness after Traumatic brain injury(TBI). The standardized 15-point test measures a person’s ability to open their eyes and respond to spoken questions or physical prompts for movement.
- Many more athletic organizations recommend establishing a baseline image of an athlete’s brain function at the beginning of each season, immaculately before any head injuries occur.
- Baseline testing should commence as soon as a child begins a competitive sport. Brain function tests yield information about an individual’s attention, memory, and capability to concentrate and solve problems. Brain function tests can be repeated regularly every one to two years and also after a suspected concussion.
- The results may help healthcare providers identify any effects of an injury and allow them to make more informed decisions about whether a person is ready to return to their normal activities.
How is a traumatic brain injury (TBI) Treated?
Treating traumatic brain injury(TBI)
- Many more factors involving the size, severity, and location of the brain injury influence how a traumatic brain injury is treated and how quickly a person might recover. One of the critical elements of a person’s prognosis is the severity of the injury. Although brain injury often so at the moment of head impact, much of the injury related to severe traumatic brain injury develops from secondary injuries which happen days or weeks after the initial trauma. In this case, people who receive immediate medical attention at a certified trauma center tend to have the best health results.
Mild traumatic brain injury(TBI)
- Few people with mild traumatic brain injury such as concussion might not require treatment other than rest and over-the-counter pain relievers. Treatment should concentrate on symptom relief and “brain rest.” Monitoring by a healthcare practitioner is important to note the worsening of symptoms or new ones.
- Teens and Children who have a sports-related concussion should stop playing immediately and return to play just after being approved by a concussion injury specialist.
- Preventing future concussions is critical. While most people recover fully from a first concussion within some weeks, the rate of recovery from a second or third concussion is normally slower.
- Even after symptoms resolve entirely, people should return to their daily activities gradationally onetime they are given permission by a doctor. There is no clear timeline for a safe return to normal exercise although there are guidelines such as those from the American Academy of Neurology and the American Medical Society for Sports Medicine to support determining when athletes can return to practice or competition. other research is needed to better understand the effects of mild traumatic brain injury on the brain and to determine when it is safe to resume normal activities.
People with a mild traumatic brain injury(TBI) should:
- Make an appointment for a follow-up visit with their healthcare provider to certify the progress of their recovery
- Inquire about new or persevering symptoms and how to treat them
- Pay attention to any new signs or symptoms indeed if they feel unrelated to the injury (for example, mood swings, unusual feelings of irritability)
- These symptoms may be related indeed if they occurred several weeks after the injury.
Medications to treat some of the symptoms of traumatic brain injury might include:
- Over-the-counter or prescribed pain medicines
- Anticonvulsant drugs to treat seizures
- Anticoagulants to prevent blood clots
- Diuretics to support reduce fluid buildup and reduce pressure in the brain
- Stimulants to increase alertness
- Antidepressants and anti-anxiety drugs to treat depression and feelings of fear and nervousness
Severe traumatic brain injury(TBI)
- Immediate treatment for those who have suffered a severe traumatic brain injury focuses on preventing death; stabilizing the person’s spinal cord, heart, lung, and other vital organ functions; ensuring proper oxygen breathing and supply; controlling blood pressure; and preventing further brain injury.
- Emergency care staff will watch the flow of blood to the brain, brain temperature, pressure inside the skull, and the brain’s oxygen supply.
Surgery might be needed for emergency medical care and to treat a secondary injury, involving:
- Relieving pressure inside the skull (inserting a catheter through a hole drilled into the skull to drain fluids)
- Removing dead brain tissue (especially for penetrating traumatic brain injury)
- Removing hematomas
- Repairing skull fractures
In-hospital strategies for managing people with severe traumatic brain injury goals to prevent conditions involve:
- Infection, particularly pneumonia
- Deep vein thrombosis (blood clots that are so deep within a vein; risk increases during long periods of inactivity)
People with traumatic brain injuries may need nutritional supplements to minimize the effects that minerals, vitamins, and other dietary deficiencies might cause over time. Many individuals may even require tube feeding to maintain the proper balance of nutrients.
Rehabilitation
- After the acute care period of in-hospital treatment, people with severe traumatic brain injury are oft transferred to a rehabilitation center where a multidisciplinary team of healthcare providers helps with recovery.
- The rehabilitation team involves neurologists, nurses, psychologists, and nutritionists, as well as physical, occupational, vocational, speech, and respiratory therapists.
- Therapy is goals at improving the person’s capability to handle activities of daily living and address cognitive, physical, occupational, and emotional difficulties. Treatment might be demanded on a short-term basis or throughout a person’s life. Few therapies are provided through outpatient services.
- Cognitive rehabilitation therapy (CRT) is a strategic goal of helping individuals regain their normal brain function through an individualized training program. Using this strategy, people might also learn compensatory strategies for coping with persistent deficiencies including memory, problem-solving, and thinking skills to get things done. Cognitive rehabilitation therapy programs tend to be highly subjective and their success varies. A 2011 Institute of Medicine report concluded that cognitive rehabilitation interventions require to be developed and assessed more completely.
- Other factors that influence recovery involve genes and age.
- Genes:– Genetics might play a role in how quickly and fully a person recovers from a traumatic brain injury. For example, investigators have found that apolipoprotein E ε4 (ApoE4) a genetic variant associated with higher risks for Alzheimer’s disease is associated with worse health issues following a traumatic brain injury. Important work remains to be done to decide how genetic factors, as well as types of head injuries, affect recovery. This research might lead to new treatment strategies and improved issues for people with traumatic brain injury.
- Age:– Studies suggest that age and the number of head injuries a person has suffered over those lifetimes are two critical factors that impact recovery. For example, traumatic brain injury-related brain swelling in children can be many different from the equal condition in adults, indeed when the primary injuries are suchlike. Brain swelling in newborns, young infants, and teenagers oft so much further quickly than it does in older individuals. Evidence from many limited CTE studies suggests that younger people (ages 19 to 41) tend to have behavioral and mood changes associated with CTE, while those who are older (ages 45+) have also cognitive difficulties.
- Compared with younger adults with equal traumatic brain injury severity, aged adults are likely to have less complete recovery. Aged people also have more medical issues and are oft taking multiple medications that might complicate treatment (e.g., blood-thinning agents when there is a risk of bleeding into the head). Further research is demanded to determine if and how treatment strategies might require to be adjusted based on a person’s age.
Medications
Medications to limit secondary damage to the brain instantly after an injury might involve:
- Anti-seizure medicines:– People who’ve had a moderate to severe traumatic brain injury are in danger of having seizures during the first week after their injury.
- An anti-seizure drug might be given during the first week to avoid any additional brain injury that might be caused by a seizure. Remained anti-seizure treatments are used only if seizures occur.
- Coma-inducing medicines:– Doctors sometimes use medicines to put people into temporary comas because a comatose brain needs less oxygen to function. This is particularly helpful if blood vessels, compressed by increased pressure in the brain, are unable to supply brain cells with normal volumes of nutrients and oxygen.
- Diuretics:- These medicines reduce the volume of fluid in tissues and increase urine output. Diuretics, given intravenously to people with traumatic brain injury, assist reduce pressure inside the brain.
Surgery
Emergency surgery might be demanded to minimize additional damage to brain tissues. Surgery might be used to address the following problems:
- Removing clotted blood (hematomas):– Bleeding outside or within the brain can result in a collection of clotted blood that puts pressure on the brain and injures brain tissue.
- Repairing skull fractures:– Surgery might be demanded to repair severe skull fractures or to remove pieces of the skull in the brain.
- Bleeding in the brain:- Head injuries that cause bleeding in the brain might demand surgery to stop the bleeding.
- Opening a window in the skull:- Surgery might be used to relieve pressure inside the skull by draining accumulated cerebrospinal fluid or creating a window in the skull that provides more room for swollen tissues.
Rehabilitation specialists may include:
- Physiatrist:- A doctor trained in physical medicine and rehabilitation, who oversees the entire recovery process, manages medical rehabilitation problems and prescribes medication as needed
- Occupational therapist:- helps the person learn, relearn or improve skills to perform everyday activities
- Physical therapist:– who supports with mobility and relearning movement patterns, balance, and walking
- Speech and language therapist:– who supports the person’s better communication skills and uses assistive communication devices if necessary
- Neuropsychologist:– who assesses cognitive impairment and performance, supports the person manage behaviors or learn coping strategies, and provides psychotherapy as needed for emotional and psychological well-being
- The social worker or case manager facilitates access to service agencies, supports with care decisions and planning, and facilitates communication among various professionals, care providers, and family members
- Rehabilitation nurse:– who provides ongoing rehabilitation care and services and who supports discharge planning from the hospital or rehabilitation facility
- Traumatic brain injury nurse specialist:– who supports coordinates care and educates the family about the injury and recovery process
- Recreational therapist:– who supports time management and leisure activities
- A vocational counselor:– assesses the ability to return to work and appropriate vocational opportunities and provides resources for addressing common challenges in the workplace
Physiotherapy Treatment
Just as two people are not exactly similar, no two brain injuries are exactly alike. thus, the approach to neurological rehabilitation and physiotherapy after traumatic brain injury should observe neuroplasticity, motor learning, and motor control principles as well as take a patient-centered approach with individual involvement in goal setting and choice of treatment procedures.
- Initial treatment during the acute phase focuses on advancing respiratory health and prevention of secondary adaptive changes to the musculoskeletal system.
- Subacute physiotherapy management focuses on the provision of an appropriate environment to support functional recovery and on the supported practice of meaningful tasks, relevant to the capability of the individual, using a full range of treatment modalities.
- Post-acute physiotherapy management focuses on reversing secondary adaptive changes and improving specific motor skills with a focus on functional goals for day-to-day activities and is dependent on skilled sensorimotor assessment and a collaborative approach with other team members, the individual, and the family. This stage can involve inpatient, outpatient, and community-based settings and for a few individuals might require lifelong access to services involving planned reviews.
Preventing Traumatic Brain Injury(TBI)
The best treatment for traumatic brain damage is prevention. Unlike most neurological diseases, head injuries can be prevented. According to the CDC, the following actions can support prevent traumatic brain injuries:
- Wear a seatbelt when you drive a car during a ride in a motor vehicle
- Wear the correct helmet and make sure it fits suitably when riding a bicycle, skateboarding, and playing sports like hockey and football
- Install window guards and stair protection gates at home for young children
- Noway drive under the influence of medicines or alcohol
- Perfect lighting and remove rugs, clutter, and different trip hazards in the hallway
- Use non-slip mats and install grab bars next to the restroom and in the tub or shower for aged adults
- Install handrails on stairways
- Improve balance and strength with a regular physical exercise program
- Ensure children’s playgrounds are produced of shock-absorbing material, such as hardwood mulch or sand
FAQ
Traumatic brain injury is sudden damage that causes injury to the brain. It might happen when there is a blow, or bump to the head. This is a closed head injury. A traumatic brain injury can also be when an object penetrates the skull.
A traumatic brain injury is damage that affects how the brain works. Traumatic brain injury is the most cause of death.
A new study has found that many people with moderate to severe traumatic brain injury achieve favorable outcomes over the course of their first year of recovery, moving from a deep coma to being suitable to live independently for at least eight hours per day within a year.
Moderate and severe traumatic brain injury can lead to a lifetime of physical, emotional, and behavioral changes. These changes might affect a person’s ability to function in their everyday life.
the risk of having a traumatic brain injury is substantial among all age groups, this risk is highest among adolescents, young adults, and persons aged over 70 years. The risk of traumatic brain injury among males is twice the risk among females.
These changes might affect a person’s ability to function in their everyday life. Despite initial hospitalization and inpatient rehabilitation services, about 50% of people with traumatic brain injury will experience further decline in their daily lives or die within 4 to 5 years of their injury.
Yes, it can, but it can also improve. Causes of decline after brain injury might vary, but there are certain approaches you can take to encourage recovery.
Many patients can and do live a full life after a traumatic brain injury.
Traumatic brain injury(TBI) is a major cause of death & disability.
Brain injury may be deathless or temporary and recovery can be prolonged.
During the first 24 hours, acetaminophen can be used for pain relief. After the first 24 hours, ibuprofen (Advil) and naproxen sodium (Naprosyn, Aleve) are normally more effective for pain relief and are safe.
Avoid activities that are physically demanding (e.g., housecleaning, weightlifting, or working out) or require a lot of concentration (e.g., balancing).



8 Comments