ALZHEIMER’S DISEASES AND PHYSIOTHERAPY
Table of Contents
ALZHEIMER’S DISEASE:
Alzheimer’s disease (AD), also referred to simply as Alzheimer’s, is a chronic neurodegenerative disease that usually starts slowly and gradually worsens over time. It is the cause of 60–70% of cases of dementia.
NEUROPHYSIOLOGY:
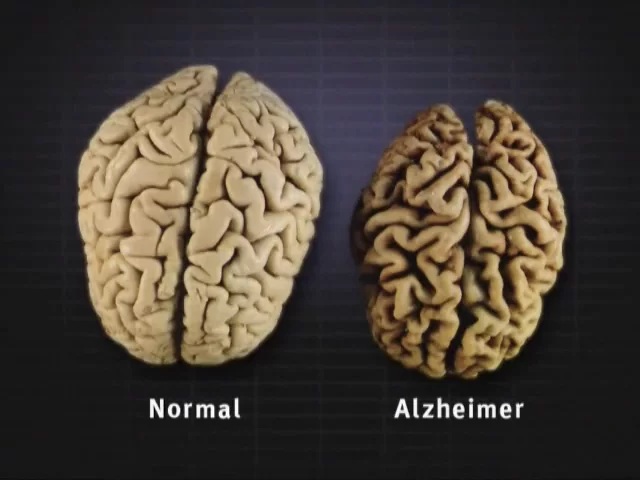
Alzheimer’s disease is characterized by the loss of neurons and synapses in the cerebral cortex and certain subcortical regions. This loss results in gross atrophy of the affected regions, including degeneration in the temporal lobe and parietal lobe, and parts of the frontal cortex and cingulate gyrus. Degeneration is also present in brainstem nuclei like the locus coeruleus. Alzheimer’s disease has been identified as a protein misfolding disease (proteopathy), caused by plaque accumulation of abnormally folded amyloid beta protein and tau protein in the brain.
PRIMARY RISK FACTORS:
-Advancing age
-Direct family member with the disease (mother, father, brother or sister) Risk genes that increase the likelihood of developing the disease.
-Cardiovascular risk factors: mid-life obesity, mid-life hypertension, hyperlipidemia, diabetes mellitus.
POSSIBLE RISK FACTORS:
-Head trauma – older adults with moderate traumatic brain injury (TBI) increases risk.
-History of depression
-Progression of Parkinson-like signs in older adults
-Hyperhomocysteinemia
-Folate deficiency
-Hyperinsulinemia
-Lower educational attainment
-Sleep disturbances
-High blood pressure in midlife
-Hyper/hypothyroidism
STAGES OF ALZHEIMER’S DISEASE:
1. Mild Alzheimer’s Disease (early stage):
-May Function Independently: may drive, work, or maybe be a part of social activities
-Memory Lapses: familiar words, location of objects, names of new people, recently read material
-Difficulties noticed by family, friends, and doctors: challenges performing activities at home or work, difficulty planning
-Lack of spontaneity
-Subtle personality changes
-Disorientation to time and date
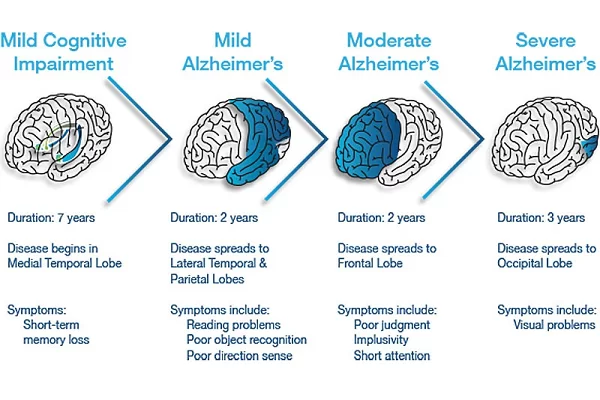
2. Moderate Alzheimer’s Disease (middle-stage) :
-Longest stage, may last for years
-Personality changes: moody or withdrawn, suspiciousness, delusions, compulsive, repetitive behavior
-Increased memory loss: forgetfulness regarding personal history, unable to recall address, phone number
-Decreased independence: trouble controlling bowel and bladder, increased risk of wandering or becoming lost, dependence on choosing -appropriate clothes for event or season, increased Confusion
-Impaired cognition and abstract thinking
-Restlessness and agitation
-Wandering, “sundown syndrome”
-Inability to carry out activities of daily living
-Impaired judgment
-Inappropriate social behavior
-Lack of insight, abstract thinking
-Repetitive behavior
-Voracious appetite
3. Severe Alzheimer’s Disease (late stage):
-Decreased response to the environment: decreased ability to communicate and may speak in small phrases
-Dependence on caregiver: decreased physical functioning: walking, sitting & swallowing; increased vulnerability to infections
-Inability to communicate
-Urinary and fecal incontinence
-Seizures
MEDICAL MANAGEMENT:
There is currently no cure for Alzheimer’s Disease, so medical management is focused on maintaining the quality of life, maximizing function, enhancing cognition, fostering a safe environment, and promoting self-engagement. Maximizing dementia functioning involves monitoring the patient’s health and cognition, patient and family education, and initiation of pharmacological and nonpharmacological treatments.
drugs are:
-Donepezil
-Rivastigmine
-Galantamine
-Tacrine
– Memantine
-Selegiline
PHYSIOTHERAPY MANAGEMENT:
although medication has no proven neuroprotective effect on dementia, a study proves the significant effect of exercise on cognition, dementia risk, and dementia progression.
-A community-based exercise program has been shown to improve multiple domains of life for individuals with Alzheimer’s.
-It has been suggested that aerobic exercise in the form of walking and upper limb cycle ergometer in particular helps to improve exercise tolerance as well as quality of life in individuals with Alzheimer’s.
-Strength training in addition to aerobic training has been supported in the research. The combination of both activities has shown greater improvements in cognition than aerobic training alone.
– Group therapy is also successful with patients with Alzheimer’s disease, but the session must not provide more stimulation than the patient is able to tolerate. Repetition and encouragement are also very important to help keep the patient’s confidence high and to help with remembering the exercises.
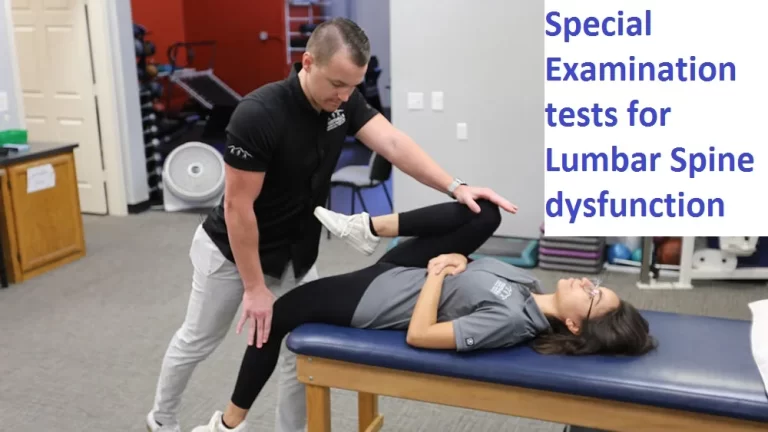
BALANCE TRAINING:

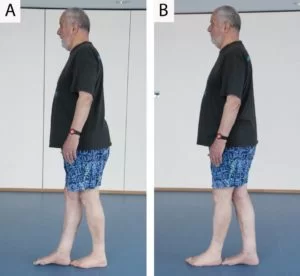
- sideway walking:
A. Stand with your feet together, knees slightly bent.
B. Step sideways in a slow and controlled manner, moving one foot to the side first.
C. Move the other to join it.
Avoid dropping your hips as you step. Perform 10 steps each way or step from one side of the room to the other.

2. cross-leg walking
A. Start by crossing your right foot over your left.
B. Bring your left foot to join it.
Attempt 5 cross-steps on each side. If necessary, put your fingers against a wall for stability. The smaller the step, the more you work on your balance.
3. heel to toe walk:
A. Standing upright, place your right heel on the floor directly in front of your left toe.
B. Then do the same with your left heel. Make sure you keep looking forward at all times. If necessary, put your fingers against a wall for stability.
Try to perform at least 5 steps. As you progress, move away from the wall.
4. one leg stand
5. step up and down


PAIN MANAGEMENT:
Various electrotherapy is used for pain management such as TENS, IFT, Ultrasound Therapy, and Infrared therapy.




18 Comments