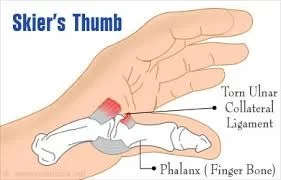
Skier’s thumb (Ulnar collateral ligament injury of the thumb)
Table of Contents
Introduction
Gamekeeper’s thumb is the other name for Skier’s thumb, also understood as a typical injury to the ulnar collateral ligament (UCL) of the thumb. It is typically caused by a sudden, forceful, and outward bending of the thumb, such as during a fall while holding a ski pole or a basketball.
The UCL is responsible for stabilizing the joint at the base of the thumb, and an injury to this ligament can cause pain, swelling, and instability of the joint. In severe cases, the ligament may be completely torn, requiring surgical intervention. Treatment for a skier’s thumb typically involves immobilizing the thumb with a splint or cast and may also involve physical therapy to restore strength and mobility to the joint. Early diagnosis and treatment are important for preventing long-term complications and ensuring a full recovery.
Definition
Injury to the ulnar collateral ligament (UCL) of the thumb (metacarpophalangeal joint (MCPJ) which has a greater danger of injuring chronic instability if not treated well. The lesion most generally happens in skiers when the ski pole forces the thumb to turn radially. a true rupture of the UCL.
Whilst both terminologies are frequently used interchangeably, the skier’s thumb determined the reason as being acute injury. Gamekeeper’s thumb is especially dictated as the reason accompanying a prolonged injury to the UCL in which it became attenuated via repetitious stress.
Damage to UCL induced by Chronic injury may retain a severe threat of incapacitating instability, pinch grip strength, and pain-free motion if not treated in the proper way.
Clinical Anatomy
The metacarpophalangeal joint of the thumb is a diarthrodial joint that permits free movement of the joints, substantiated by a capsule and by the other soft tissue structures. The neighbouring soft tissue shows both dynamic and static stability.
Passive stability is supplied by the structures given below:
- Proper collateral ligament
- Supplementary collateral ligament
- Volar plate
- Posterior capsule
The proper collateral ligament lengthens from a point just posterior to the mid-axis of the metacarpal head to the proximal phalanx of the palmar part. It resists palmar subluxation of the proximal phalanx and acts as the preliminary restriction to valgus stress with the metacarpophalangeal joint in the flexion direction. The complementary collateral ligament distribution is palmary to insert into the anterior plate. The accessory collateral ligament is adjacent to the proper collateral ligament proximally. The anterior plate and the supplemental collateral ligament role as the main restraints to valgus stress with the metacarpophalangeal joint in the extension direction.
Active stabilizers to valgus stress possess the intrinsic and extrinsic muscles of the thumb:
- Extensor pollicis brevis
- Extensor pollicis longus
- Flexor pollicis longus
- Adductor pollicis
- Flexor pollicis brevis
The superficial insertion of the adductor mechanism is the extensor expansion through the adductor aponeurosis while the deep insertion stretches to the palmar side of the proximal phalanx through the ulnar sesamoid of the metacarpophalangeal joint. There are 2 major supportive ligaments traversing the MCPJ of the thumb:
- The ulnar collateral ligament (UCL)
- The radial collateral ligament (RCL)
The UCL and RCL originate from the medial and lateral tubercles of the metacarpal condyles and insert into the base of the proximal phalanx on their respective aspects, beneath the adductor aponeurosis. The UCL prevents the thumb from pointing too distant away from the hand.
Cause of Skier’s thumb
It occurs by excessive abduction and hyperextension of the thumb. The UCL tears for the most part find a place at the distal attachment of the proximal phalange.
Trauma-provoking hyperextension of thumb
Typically associated with falls, particularly while carrying something in the hand for example a ski pole
Chronic instability may occur from overuse syndrome injuries
Mechanism of Injury
It is necessary to point out that this injury is not only to skiers and can happen to anybody where there is an excessive valgus stress force applied to the thumb in abduction and extension or a little repetitious valgus stress force. This kind of injury is also found in other sports, especially those that use a stick or ball, for example, hockey or basketball.
An acute UCL injury happens next to a sudden, hyper-abduction and hyper-extension force at the MCP joint, whereas a forced abduction movement would cause injury to the RCL. With respect to skiing, the trauma oftentimes happens when a person lands on an extended hand while keeping a ski pole, which results in forced abduction of the thumb with extension. It is known as a skier’s thumb but can also happen in football, handball, basketball, rugby, soccer, and even a handshake. If the trauma to the UCL is treated improperly this can result in chronic laxity, joint instability, pain, weakness, and arthritis in the MCPJ.
Epidemiology
It involves 86 percent per injury to the base of the thumb and merely approximately 200,000 patients per year in the USA. Skier’s thumb is the 2nd most common ski-related injury next to knee trauma, and more frequent in men than ladies. The generality of this trauma during skiing alters from 7 percent up to as high as 32 percent of all skiing injuries and is the most common injury of the upper limb that skiers experience. Only an evaluated ten percent of the patients interpreted with a skier’s thumb had developed this injury skiing.
The most considerably common cause for a skier’s thumb is a fall on the extended hand, usually from a cycle or motorcycle (that is the thumb gets adhered down the handlebars), which is found in near to forty percent of patients. Other sports for instance soccer or fighting are accountable for another estimated 30 percent of the reasons.
In children, who still have an adolescent skeleton, hyperabduction trauma greatly results in a Salter-Harris III avulsion of the UCL insertion and constantly a true rupture of the UCL.
Symptoms of Skier’s thumb
The most typical demonstration is pain over the ulnar side of the MCPJ of the thumb. If the damage is resent there will be the presence of bruising and inflammation. There may be the presence of tenderness with palpation, which confines the damage to the ulnar side of the thumb where the UCL is lesioned. In more long-lasting situations the patients generally complain of pain and weakness in the pincer grip, and instability of the thumb with doing these ADLs. In the example of a Stener lesion, there is a presence of a palpable mass located proximal to the adductor aponeurosis.
These symptoms can happen from minutes to hours next to the fall that created the injury:
- Pain is present at the base of the thumb in the webspace among thumb and index digits.
- Swelling of your thumb.
- difficulty to hold an object or weakness of grasp between your thumb and index digits.
- Tenderness to the palpation along the index digits side of your thumb.
- Discolouration (blue or black) appearance of the skin over the thumb.
- Thumb pain that worsens with activity in almost all directions.
- Pain inside the wrist (which may be referred pain that originates from your thumb).
Grades of thumb sprains
Thumb sprains are graded by how much the ligament is drawn or torn away from the insertion. Classification of UCL damage according to Hintermann et al is given below:
Type Injury Examination
- I Displaced fracture Stable in flexion (<30°)
- II Displaced fracture No special test
- III No fracture Stable in flexion (<30°)
- IV No fracture Unstable in flexion (>30°)
- V Avulsion fracture of the volar plate Stable in flexion
Differential Diagnosis
The injury can affect other structures for example adductor aponeurosis, the accessory collateral ligament, bony structures, tendons, and neurological tissues. The injuries have common complaints of weakness of the pincer grasp. Nevertheless, they may be determined by the area of tenderness.
- Stener lesion: A sterner lesion happens in the history of forceful abduction of the thumb, resulting in the avulsion of the distal ulnar collateral ligament from the bone underneath the proximal phalanx of the thumb.
- Bennett or Rolando fracture: is an intra-articular fracture luxation at the bottom of metacarpals I in the carpometacarpal joint.
- Avulsion fracture: In youngsters, who yet carry an immature skeleton, excessive abduction concussion mostly oversees a Salter-Harris III avulsion of the UCL insertion and infrequently to a true rupture of the UCL.
- Wrist sprain: when a wrist sprain injury happens, the ligaments of the wrist are extended past their standard boundaries.
- Wrist fracture.
- Dislocation of the first metacarpophalangeal joint.
- Chronic instability of the 1st MCP joint: Damages to the two major assistive ligaments traversing the metacarpophalangeal (MCP) joint of the thumb can result in symptomatic joint fluctuation with the following pain, weakness, and arthritis if neglected.
- Lunate dislocation.
- Neuropraxia of the radial nerve occurs secondary to traction, swelling, or stiffness.
- Rheumatoid arthritis or osteoarthritis.
Outcome Measure
Michigan Hand Outcomes Questionnaire (MHQ).
Dynamometer(Which measured power grip and key pinch strength).
Visual analog scale or pain follow-up.
Stability of the MCP joint as examined by stress testing as performed in the assessment.
Complication
If the UCL is damaged is present then it is expected that the distal end may turn interrupted by the adductor aponeurosis, which is mentioned as a Stener lesion. A Stener lesion is challenging to diagnose but leads to inadequate recovery and commonly used operative treatment. If left untreated, a torn UCL can result in joint instability and weakness in the pinch grip.
Diagnostic Procedures
The kind of lesion can be poorly derivative by way of X-ray, ultrasound, or MRI.
X-rays
Antero-posterior and lateral X-ray films of the thumb are interpreted to eliminate any related bony involvement. Related to bony avulsion fractures are found in 20 percent–30 percent of UCL injuries. The point of an avulsed bony piece commonly shows the place of the distal end of the UCL. Indications for surgical treatment supported by imaging exclude avulsion fractures with displacement of more than 5 mm or any fracture regarding 25 percent or more of the MCP joint surface. Stress X-ray films of the thumb MCP joint have even been utilized for diagnosis.
MRI
MRI may be found as a gold standard with a sensitivity of 96 percent-100 percent and specificity of 95-100 percent. Another alternative can be an ultrasound of the thumb. It is advised by many as the best modality for diagnosing UCL trauma, particularly for chronic UCL injuries.
Ultrasound
Ultrasound (US) is an optimum and cost-effective choice for diagnosing UCL trauma due to it permits direct imaging of the complete UCL and nearby structures. It determines the torn end of the UCL in nearly 90 percent of situations. The diagnosis must be done by the US prior to conservative therapy being done with a glove spica cast. There are several limitations when applying, for instance, the ultrasound cant be indicated after one week next to the initial trauma due to shrinking of the torn ligament, and scar tissue can be contradictory when making a diagnosis or for chronic UCL injuries.
The sensitivity of the US was 95.4 percent with a specificity of 80 percent for sensing Stener lesions.
Arthrography
Arthrography is described as the enlargement of the metacarpophalangeal joint by inserting direct distinction material and is observed by imagining the joint by X-ray or MRI (MR-arthrography).
Clinical and anatomical findings and the perceptive of the trauma mechanics display that stability testing (performed with the joint in full flexion) and extra standard radiographs remain the backbone in determination-making in almost all MCPJ sprains
Examination
About perceiving malformation with the measurement of the hand at rest and flexion. Then test the to check the sensation of the hand after this active range of motion (AROM) followed by passive range of motion (PROM) and resisted movement is performed to evaluate tendon integrity, if manageable. The clinical investigation may on occasion uncover a tender swelling and a hematoma at the ulnar aspect of the base of the thumb. If there is a fracture indicated to the first metacarpal or proximal phalanx of the thumb, evident radiography is used prior to stress testing of the UCL.
Clinical investigation and X-rays are delicate to detect UCL injuries. If there is no related fracture of the shaft, the thumb MCP joint stability is tested by the stress test, and discover the steady endpoint is given below;
- The metacarpal is stabilized with the help of another hand to support the proximal phalanges of the thumb to avoid any strain.
- With the proximal phalanges in 30-degree flexion radial emphasis is practical and repeated in the extended place to detect the steady endpoint.
- The degree of divergence contrast with the other hand, a variation of 15 degrees between the affected and alternate sides in flexion, or the degree greater than 35 degree denotes a tear of the particular UCL and in extension a tear of the adjunct portion of the UCL.
- If it is impaired sensation is present it indicates a complete UCL tear, the absence of a firm end feel during examination is a greater dependable standard when clinically diagnosis a total rupture of the UCL
- If there is a stener lesion the tester will sense a ligamentous lump.
A stress test may be uncomfortable and the tester may be essential to use local anaesthesia to may do the test and prevent tension of the nearby muscles. It is just to say we can find laxity or instability of the thumb MCP joint in situations of chronic UCL injuries.
An examination by Cooper et al “Local anaesthetic incursion enhanced the accuracy of assessment of ulnar collateral ligament injuries” Represented how Oberst anaesthesia (in which 1–2 ml of lidocaine is injected in the MCP joint) increases the clinical accuracy from 28 percent to 98 percent after an average of one week next to the early trauma.
In much of the literature, the following standard has been followed for laxity of the metacarpophalangeal joint.
Treatment
A UCL injury may be treated conservatively or medical procedures rely on the respective components that chiefly possess:
- Timing of presentation (acute or chronic)
- Grade (severity of injury)
- Displacement (Stener lesion), and it is crucial for management to separate between displaced and non-displaced UCL traumas
- Area of trauma (mid-substance or peripheral) Associated or concurrent vast tissue concussions like bone, anterior or volar plate, etc. Patient-linked element (job environment demands, etc.)
The management of UCL injuries depending upon Hintermann’s classification recommended is given below:
- Type I injuries necessitate cast immobilization for around four weeks.
- Types III and V injuries necessitate cast immobilization for around three weeks.
- Types II and IV injuries necessitate surgical care.
Surgical Treatment
Operative treatment relies on a timely diagnosis of the traumas, prolonged lesions become much more challenging to fix with enhanced duration since injury since leftover tissue becomes decreased not robust adequate to give adequate help to the joint. Operative consideration is taken out if the trauma is grade 1 or 2 and united with a Stener lesion or displaced avulsion fracture is there, grossly, a current unstable joint, and cases of volar subluxation found on radiographs. There are various methods of repair, which can be classified into dynamic or static.
Dynamic Static
- Extensor indicis proprius tendon transfer
- Extensor pollicis brevis tendon transfer
- Adductor pollicis brevis tendon transfer
Dynamic procedures are more likely to loosen with a period of time normally conserving better mobility of the MCP joint.
Static
- Figure-of-eight grafting
- Parallel configuration graft
- Triangular configuration with proximal apex graft
- Triangular configuration with distal apex graft
- Tendon graft weaves
- Hybrid technique
- Free tendon graft
There is a broad variety of static operations and there are still many arguments about which treatment method is the best. Many management provides positive outcomes which result in a lot of arguments.
Provided the operation has been done timely ( choice of outcome drops when surgery is delayed, a better outcome can still be achieved after three–four weeks. A time period of mostly six weeks of immobilization is required, later which a new radiography is made and physiotherapy can be started. When the pain has lessened and the range of motion has started improving, the hand can be used over again for absolute results. Normally, this takes approximately three months. Patients with the worsened result are largely patients with a delay in display. When repaired in a timely manner, complications are infrequent.
Not sufficient info is accessible on the chances for repetition with this kind of injury. Also, no trials have even been set up to look into whether surgical intercession is truly superior to non-operative care.
Follow up.
The operating surgeon will see the patient after a surgical fix or after a time period of immobilization in a cast. The patient’s thumb will be reexamined again. The doctor will determine if the patient is required to carry on to immobilize the thumb or if physiotherapy is required to recover movement.
Conservative treatment
Incomplete UCL traumas for example ligament strains, in complete tears, low-demand patients, and inadequate-operative nominee, regard patients with degenerative MCP joint disease are efficaciously managed conservatively.
Arguments also present around managing a bony skier’s thumb without surgery. The profession all the same displays that if the MCP joint is stable during testing and there is no dislocation of the segment, this injury can be managed conservatively without account for concern. For patients with:
- <30 degrees of valgus laxity of straightening of the Metacarpophalangeal joint.
- <15 degrees distinct between sides and no signal of avulsion fracture on X-ray.
Immobilization
From 10 days up to 6 weeks, relying on the degree of laxity during the early examination. Investigator convinced on four to six weeks through with up to twelve weeks relay on the degree of the lesion, suggestions are given below:
- A short-arm thumb spica cast
- Thermoplastic splint: permits the patient to start the activity of the interphalangeal joint.
- A hand-based dismissible thumb spica orthosis. The MCP joint is immobilized, with the MCP fixed and the IP joint leftover free to avoid any unneeded stiffness.
- Wearing a splint will prevent putting radial stress on the thumb and provide the ligament time to recover.
- The best orientation for the splint respect retention is the MCPJ in slight flexion with a little ulnar deviation that imparts the torn ligament fragments closer and helps in the recovery, the interphalangeal joints must not be immobilized in the cast.
Physical Therapy Treatment
The management of a skier’s thumb is variable depending on the level of injury such as incomplete and complete ruptures. Incomplete ruptures are managed conservatively. The MCP joint is immobilized, with the MCP set and the IP joint leftover free to keep unneeded stiffness. A navicular cast or brace is normally indicated. Swelling can be managed with raised above heart level while supine and the use of cold compresses as needed.
The chief purpose of rehabilitation is improving the patients’ function and reducing the time of functional recovery, the reported treatment presents potential advantages in the management of this common acute hand injury.
Exercise therapy
After the period of time of immobilization is ended, the therapy can be initiated. Most probable the patient will do exercises that assist strengthen and lengthening the joint in command to recover complete function in the thumb. The patient must start supervised hand therapy during the time period of immobilization. Slowly and gently flexion and extension range of motion exercises can be initiated later approximately four weeks, with the patient persisting to wear the splint between therapy sessions. After 8 weeks advanced strengthening exercises may start, but unrestricted activity is not permitted until after 12 weeks. Gripping and pinching movement must not begin until 10-12 weeks and must be advanced as tolerated; forceful gripping activities are typically not bearable until about week
Post-surgical treatment
The content of the physiotherapy afterwards operation is identical to those of the conservative management, in any case:
- Duration of Immobilization: usually 6 weeks is applied
- Control radiography after immobilization Following surgery a splint is usually worn for four to six weeks. The contiguous post-surgical motion of the operated joint produced quicker and finer functional outcomes. Consequently, the usage of a functional splint is advisable, as well as the early advancing start with moving within the boundaries of pain. Sportsmen whose injuries necessitate operation can commonly come back to play in approximately three to four months. The written report of Derkash, considering pain, stability, muscular power (tweezers grip), and functionality in ADL, reveals that < 5 percent of the patients face a weakened tweezers grip and stiffness. The pain was not present or mild in 99 percent of the circumstance. 96 percent of the treated patients were satisfied with the outcome of the operation. When a secondary operation is requisite outcomes were less successful. When the pain has lessened and the range of motion has entirely returned, the hand can be totally utilized over again. Commonly, this takes approximately 3 months.
Exercises
Thumb active range of motion
- With your palm plane on a table or different surface, take your thumb away from your palm as far as possible. Grasping this place for five seconds and take it back to the initial place. Then rest your hand on the table in a handshaking gesture.
- Grab your thumb out to the side away from your palm as far as possible.
- Grip for 5 seconds. Return to the starting position.
- Side by side, take your thumb crossways your palm toward your little digit.
- Hold this position for 5 seconds. Return to the starting position. Repeat this entire sequence 15 times. Do 2 sets of 15.
Wrist range of motion
- Flexion: Gently bend your wrist forward. Hold for 5 seconds. Do 2 sets of 15.
- Extension: Gently bend your wrist backward. Hold this position for 5 seconds. Do 2 sets of 15.
- Side to side: Lightly move your wrist from side to side (a handshaking gesture). Hold for 5 seconds in each direction. Do 2 sets of 15.
- Thumb strengthening: Picking up little items, for instance, paper clips, pens, and coins, utilizing your thumb and each of your different fingers, one at a time. Do this exercise for around 5-10 minutes.
- Finger spring: Place a big rubber band just about the outside of your thumb and digits. Open your digit to expand the rubber band. Do 2 sets of 15 repetitions.
- Grip strengthening: Squeeze a soft ball and keep squeezing and count for five seconds. Repeat 2 sets of 15 repetitions.
- Wrist flexion: Keep a light bottle or handle of the hammer in your hand with your palm upward. Bend your wrist upward. Slowly down the load and return to the initial place. Do 2 sets of 15. Step by step slowly adds the load of the can or load you are keeping.
- Wrist extension: Grasp a soup can or striker handle in your hand with your palm facing downward. Slowly bend your wrist up. Slowly take down the load into the initial place. Do 2 sets of 15. Bit by bit enhanced the load of the items you are keeping.
FAQ
1. Put your forearm and hand on a flat surface. Your involved thumb must point upward direction.
2. With your other hand, keep your thumb steady slightly below the joint closest to your thumbnail.
3. Bend the tip of your thumb down. Then straighten it.
4. Repeat 8 to 12 times.
5. Do this exercise several times a day.
Since the ligament has been totally torn and thrust away from its original anchored place, it cannot recover decently. When this happens, a surgical operation is needed to return the ligament to its original anatomical place. Other than that, permanent loss of thumb stability and pinch strength may consequence.
Symptoms:
Presence of pain at the base of the thumb in the web space between thumb and index digit.
Presence of swelling around your thumb.
Difficulty to grasp or weakness of grasp between your thumb and index digits.
Tenderness to palpate along the index digits side of your thumb.
Discolouration of the skin over the thumb.
At some point as you heal, your helper will instruct you to start exercises to regain movement and strength in your thumb. This may be as soon as three weeks or as long as eight weeks afterward your injury. When you re-start an activity next to a sprain, builds up gradually. If your thumb set is about to hurt, stop using it for a while.
Rest, ice, compression, and elevation (RICE). RICE can do useful for a thumb injury.
Non-steroidal anti-inflammatory drugs (NSAIDs).
Prescription painkillers.
Immobilization with a splint, cast, or brace
Physiotherapy.
Operation.