Transient Ischaemic Attack (TIA)
Table of Contents
What is a Transient Ischaemic attack (TIA)?
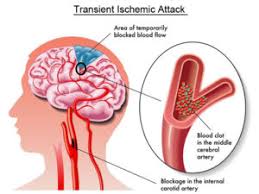
A transient ischemic attack (TIA) is a temporary neurologic dysfunction due to a temporary blockage in the blood supply to part of the brain. It is also called a ministroke, a TIA may be a warning sign of a future stroke and a chance to prevent it.
It resolves within a few minutes to hours, However, it requires immediate medical treatment to avoid an actual stroke.
The clinical definitions of Transient Ischemic Attack (TIA) and ischemic stroke are dependent on focal neurologic signs or symptoms referable to recognizing cerebral arterial distributions without direct measurement of blood flow or cerebral infarction. It is necessary to record that TIA and stroke represent various ends of an ischemic continuum from the physiologic perspective, but clinical management is alike.
The definition of a TIA has turned from time-based to tissue-based. A TIA Typically lasts less than 1 hour, more frequently minutes. It may be thought about as a serious warning for an impending ischemic stroke – the risk is greater in the first few hours following a TIA.
Differentiating TIA from other mimicking conditions is important. Generally connected with a focal neurologic deficit and/or speech disturbance in a vascular territory because of underlying cerebrovascular disease. Usually sudden in onset. Diagnosis should be done quickly with imaging and laboratory studies to reduce the risk of upcoming strokes.
The following risk of TIA or ischemic stroke may be stratified with a simple clinical measure. Quick multimodality therapeutic interventions should be started. The concept of TIA was established in the 1950s, with the observation by C Miller Fisher, and others, that ischemic stroke frequently followed transient neurological symptoms in the same arterial territory.
Difference between stroke and Transient ischemic attack
- In the 1960s, transient ischemic attacks were allowed to be sudden, focal neurological deficits of vascular origin lasting less than twenty-four hours (an arbitrarily assigned endpoint).
- A stroke was considered to have taken place if a neurological deficit remained for more than 7 days.
- Those neurological events that lasted between twenty-four hours and the 7 stroke threshold were classified as a reversible ischemic neurological deficit – a term now rendered obsolete.
- Its removal definitions came when it was proven that most incidents lasting twenty-four hours to 7 days were connected with cerebral infarction and thus should take the diagnosis of stroke.
Mechanism of Injury
- Like ischemic strokes, TIAs are because of locally reduce blood flow to the brain, causing focal neurological symptoms.
- Reduced blood flow results from one of two embolisms into a cerebral supply artery (from the heart, or the great proximal vessels, extracranial or intracranial arteries, usually affected by atherosclerosis), or in situation occlusion of small perforating arteries.
- Aspiration of symptoms mostly happens by spontaneous lysis or distal passage of the occluding thrombus or embolus, or by recompense through collateral circulation restoring perfusion into the ischemic brain area.
Causes of Transient Ischaemic Attack
TIA subtypes, classified elicited from the pathophysiological mechanisms are similar to ischemic stroke subtypes. They involve
- Large artery atherothrombosis
- Cardiac embolism
- Small vessel (lacunar)
- Cryptogenic (obscure or unknown origin)
- Uncommon subtypes like vascular dissection, vasculitis, etc.
- The usual risk factors for all TIA involve diabetes, hypertension, age, smoking, obesity, alcoholism, unhealthy diet, psychosocial stress, and irregular physical activity.
- A past history of stroke or TIA will improve substantially the subsequent risk of recurrent
- stroke or TIA.
- Of all risk factors, High blood pressure(hypertension) is the most crucial one for people as well as for people.
Epidemiology
- TIA incidence in a population is difficult to approximate because of other mimicking disorders.
- Internationally, the probability of a 1st TIA is around 0.42 per 1000 population in expanded countries.
- TIA incidence in America could be around half a million per year and approximately are about 1.1 per 1000 American individuals.
- The approximate overall prevalence of TIA among adults in America is estimated at 2%. It occur in about 150,000 patients every year in the United Kingdom.
- It has been shown that past stroke history improves the prevalence of TIA.
- Few studies have shown that the majority of individuals who presented with prior stroke had prior TIA symptoms.
Age
- The incidence of TIAs improves with age, from 1-3 cases per 100,000 in those younger than thirty-five years to as many as 1500 cases per 100,000 in those older than eighty-five years.
- Fewer than three percent of all major cerebral infarcts happen in children.
- Pediatric strokes frequently may have quite different causes from those of adult strokes and tend to happen with minimal frequency.
Gender
- The incidence of TIAs in males (101 cases per 100,000 population) is significantly greater than that in females (70 per 100,000).
Signs and symptoms of a Transient Ischaemic Attack
- Clinical manifestations will be different, based on the vessel include and the cerebral territory it supplies.
- The vital rule here is that symptoms of TIA should mimic known stroke syndromes, and so based on the arterial territory include;
- A TIA can last only minutes, therefore symptoms have frequently resolved prior to the patient’s presents to a clinician.
- Thus, historical questions should be picked out not just for the patient but also for family members or friends who were present at the time of TIA.
- Witnesses frequently perceive abnormalities that the patient may not, like changes in behavior, speech, gait, memory, and movement.
Diagnostic Procedures
The main diagnostic challenge of TIA is that the symptoms and signs have generally resolved by the time of assessment.
National Stroke Association accepted guidelines for TIA evaluation as follows in 2006:
- CBC = complete blood count
- CEA = carotid endarterectomy
- TCD = Transcranial Doppler
- TEE = Transesophageal echocardiogram
- TTE = Transthoracic echocardiogram
The ABCD2 score is very necessary for predicting subsequent risks of TIA or stroke. It gives a more robust prediction standard. The ABCD2 score involves factors involving age, blood pressure, clinical symptoms, duration, and diabetes.
- Age: older than 60 years (1 point)
- Blood pressure more than or equal to 140/90 mmHg on first evaluation (1 point)
- Clinical signs: a focal weakness with the spell (2 points) or speech impairment without weakness (1 point)
- Duration more than 60 min (2 points), or 10 min to 59 min (1 point)
- Diabetes mellitus (1 point).
- The two-day risk of stroke was 0% for scores of 0 or 1, 1.3% for 2 or 3, 4.1% for 4 or 5, and 8.1% for 6 or 7.
- Most stroke clinics will admit patients with TIA to the hospital for expedited management and observation if the score is four or five or higher.
- For those patients who have a minimum score, expedited evaluation and management are still warranted.
- This expedited approach has been proven to increase the result.
Differential Diagnosis
- Differential diagnosis of TIA involves but is not limited to
- Vertigo or dizziness
- Seizures
- Headaches, migraine Aura
- Bells palsy
- Drug withdrawal
- dementia
- Electrolyte disorders
- Acute infections
- Alcoholism.
- Stroke
- Meningitis
- Multiple Sclerosis
- Syncope
Treatment of Transient Ischaemic Attack
Once a doctor has identified the cause of the TIA, the goal of treatment is to correct the issue and prevent a stroke. Based on the cause of the TIA, the doctor can prescribe medication to decrease the tendency for blood to clot or can suggest surgery or a balloon procedure (angioplasty).
Medications
Anti-platelet drugs
- These medications make the platelets, one of the circulating blood cell types, less likely to swing together.
- When blood vessels are injured, sticky platelets start to form clots, a process completed by clotting proteins in blood plasma.
- The most often used anti-platelet medication is aspirin.
- Aspirin is also the low expensive treatment with the fewest potential side effects.
- A difference to aspirin is the anti-platelet drug clopidogrel (Plavix).
- The doctor can prescribe aspirin and clopidogrel to be taken combined for about a month after the TIA.
- Research shows that taking these 2 drugs together in particular situations decreases the risk of a future stroke more than taking aspirin alone.
- There can be particular situations when the duration of taking both medications together can be extended, like when the cause of the TIA is a narrowing of a blood vessel located in the head.
- Alternatively, a doctor can prescribe ticagrelor (Brilinta) and aspirin for 30 days to reduce the risk of recurrent stroke.
- A doctor considers prescribing Aggrenox, a combination of lower-dose aspirin and the anti-platelet drug dipyridamole, to decrease blood clotting.
- The way dipyridamole works is slightly various from aspirin.
Anticoagulants
- These drugs involve heparin and warfarin (Jantoven).
- They affect clotting-system proteins alternatively of platelet function.
- Heparin is used for a short time and is infrequently used in the management of TIAs.
- These drugs need careful monitoring.
- If atrial fibrillation is present, a doctor can prescribe a direct oral anticoagulant like apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa), or dabigatran (Pradaxa), which can be safer than warfarin.
Physiotherapy treatment in Transient Ischaemic Attack
- Studies addressing the physiotherapist’s role in lifestyle behavior changes in the TIA population are still lacking.
- Longitudinal studies are needed to give a more detailed and specific understanding of how to help people with stroke/TIA make lifestyle behavior changes.
- There is a requirement to further explore what interventions are beneficial.
- Physiotherapists play a vital role in educating this group of TIA survivors by increasing awareness and discussing lifestyle behavior changes.
- The people should be educated about the importance of physical activity, blood pressure control, smoking cessation, a healthy diet, identifying a stroke, and when to look for immediate medical assistance.
- As compared to healthy individuals, people with TIA in general lower levels of physical activity.
- There are higher chances of repetitive stroke in individuals with stroke or TIA. As inadequate or reduce levels of physical activity are one of the modifiable risk factors, individuals with stroke or TIA require additional interventions to increase their physical activity level.
- In a recent systematic review, it was revealed that lifestyle interventions that specifically encourage improving physical activity have been proven to be more successful.
- The inclusion of physicians in physical activity and exercise, like physiotherapists, can be a crucial element for success since a specialized focus on physical activity and/or adding an exercise component to lifestyle management could be advantageous.
- A TIA can mimic a stroke and up to ten percent of first-time sufferers frequently experience full-blown strokes within as little as ninety days.
- Despite the well-known statistics, no post-TIA regimen exists to help prevent future strokes — but this can be changing.
- The most usual risk factors for stroke — hypertension, physical inactivity, elevated lipids, and diabetes — also are leading risk factors for heart disease.
- scientists found that a modified version of cardiac rehabilitation was effective at decreasing some symptoms of stroke in just 6 weeks following a transient ischemic attack (TIA) frequently referred to as “mini-strokes.”
- No post-TIA regimen exists to help prevent future strokes but researchers say that requires change.
- The study showed that participating in a modified version of the 2nd phase of cardiac rehabilitation is a well-established program nationwide.
- This includes 1.5-hour sessions three times a week for 6 weeks.
- They concluded that all individuals following TIA should be offered a few rehabilitation (and to see their GPs before commencing an exercise program).
Surgical treatment
Carotid endarterectomy
- If a person has a moderately or severely narrowed neck (carotid) artery, a doctor can recommend carotid endarterectomy (end-ahr-tur-EK-tuh-me).
- This preventive surgery clears carotid arteries of fatty deposits (atherosclerotic plaques) prior to another TIA or stroke may happen.
- An incision is assembled to open the artery, the plaques are removed and the artery is closed.
Angioplasty
- In particular cases, a procedure known as carotid angioplasty, or stenting, is an option.
- This procedure involves utilizing a balloon-like device to open up a clogged artery and placing a small wire tube (stent) into the artery to keep it open.
FAQ
Transient ischemic attack: frequently referred to as a “mini-stroke” or TIA, where the blood flow to the brain is temporarily disturbed and as a result causes temporary signs and symptoms of a stroke that resolved quickly.
Calm the individual and place them in a lying-down position. Call 112 if any of these symptoms happen. While waiting for help to come, see the state of the person (consciousness, breathing), and report any changes to the Emergency Response Centre.
Immediate treatment with aspirin may substantially decrease the risk and severity of early coming stroke. This report has implications for physicians, who should give aspirin immediately if a TIA or minor stroke is suspected, rather than waiting for specialist assessment and investigations. ‘
Antiplatelet medication
Antiplatelet medicines stop small blood cells called platelets from sticking together and forming a blood clot. They are also known as platelet aggregation inhibitors. They involve aspirin, a combination of aspirin and dipyridamole, and clopidogrel.
Introduction. Brain magnetic resonance imaging (MRI) is the preferred and most sensitive modality after a transient ischemic attack (TIA) or minor stroke. It should involve diffusion-weighted imaging (DWI) and should be completed within twenty-four hours of symptom onset1,2; its use is 3-fold.



2 Comments