Achillis Tendon Rupture
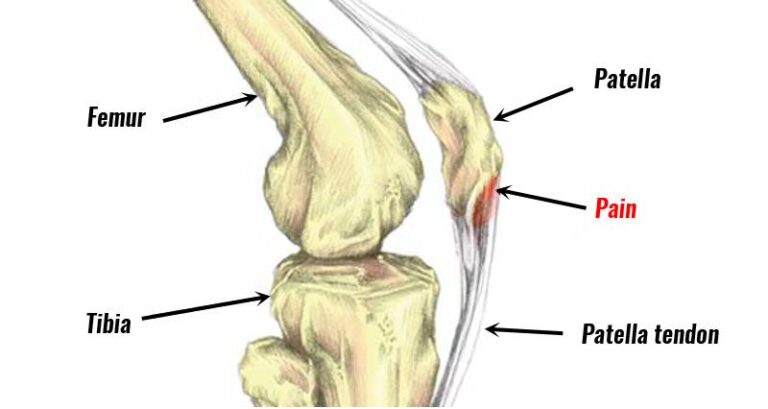
Achilles tendon rupture is a condition where the Achilles tendon, which connects the calf muscles to the heel bone, tears partially or completely. It is a relatively common injury, particularly among athletes and individuals involved in sports that require sudden bursts of acceleration or jumping.
- The Achilles tendon is a thick band of tissue that joins your calf muscle to your heel bone. It is the greatest and longest tendon in your body and is built to handle a lot of stress. Yet you can rupture your Achilles tendon under extreme stress — such as during a sudden start or stop, or if you fall. Sometimes it heals with rest and bracing, yet many people need surgery to repair it.
Table of Contents
What is an Achilles tendon rupture?
- An Achilles tendon links the calf muscle to the heel bone. This thick belt of tissue is very strong. In fact, the Achilles tendon is the highest and strongest tendon in the body. The Achilles tendon supplies your leg strength to walk, run and jump.
- An Achilles tendon rupture is a full and partial tear of the Achilles tendon. This acute (sudden) injury happens when the tendon stretches to its breaking point. It occurs most frequently during playing sports. Tripping, falling, or twisting your ankle can cause an Achilles tear.
How common are ruptured Achilles tendons?
- Achilles tendon ruptures are very usual sports injuries. They happen most often in people ages 30 to 40 and are very common in men than in women.
- People who are “weekend warriors” (usually adults who do not train regularly, then exercise at a high intensity) are more such as to tear an Achilles tendon than younger, well-trained athletes.
What causes an Achilles tendon rupture?
- The sudden movement that puts stress on the Achilles tendon can conduct in a rupture. Usually, people tear the Achilles tendon during playing sports. The large suspects are sports with quick stops, initiate, and pivots, like football, soccer, basketball, tennis, or squash. Achilles tendon tears are not always a sports injury. You can rip your Achilles tendon by tripping, missing a step when going downwards, and accidentally stepping into a hole and turning your ankle. Definite medications involving definite antibiotics and steroid injections in the part can weaken the Achilles tendon. This can put you at a greater risk of a tear.
What are the Sign and Symptoms of an Achilles Tendon Tear?
- The definitive sign and symptom of a cracked Achilles tendon is the impression and sometimes hearing of a pop and snap at the behind of your ankle. People sometimes mistakenly think something has struck them, but they are actually feeling the tendon clinch.
Other common symptoms involve:
- Sharp, sudden pain in the back of the ankle close to the heel,
- Swelling or bruising in the back of the ankle,
- Pain when walking, especially upstairs and uphill,
- Tenderness in the mark where the tendon is torn.
What are the complications of an Achilles tendon tear?
- A torn Achilles tendon is a traumatic injury that needs medical attention. Without treatment, an Achilles tendon tear may not heal correctly. This can improve your risk of rupturing it again.
How is a ruptured Achilles tendon diagnosed?
- Your healthcare provider (doctor) will physically diagnose your foot and ankle. They will detect your ability to move it in various directions and look at how you behave to pressure in the area. They will feel for a gap in the tendon that suggests it is torn.
- Your provider may also utilize imaging tests — such as ultrasound and MRI — to determine the extent of the Achilles tear.
How is a ruptured Achilles tendon treated?
Even with previous you require medical help, you can decrease pain and swelling to the injured tendon by following the RICE (Rest, Ice, Compression, Elevation) method:
- Rest, by staying off the harmed leg,
- Apply ice to the harmed area,
- Wrap your ankle to compress the harmed area and prevent more swelling,
- Elevate your leg at or above the level of your heart to decrease swelling.
- Full healing of a torn Achilles tendon typically takes about 4 (four) to 6 (six) months. Medical treatment for a torn Achilles tendon may involve:
- The injured foot and ankle must be immobilized as part of nonsurgical therapy for a torn Achilles tendon with a brace or walking cast. Your provider (doctor) will place your foot, ankle, and calf in a brace and walking cast. Your foot or ankle flexes downward so that the Achilles tendon can heal.
- Surgery: The majority of healthcare professionals (doctors) advise middle-aged or younger individuals who are active to have a torn Achilles tendon surgically repaired. During surgery, a surgeon stitches the 2 (two) ends of the torn tendon back together. Later surgery, you will require a cast on your lower limb to immobilize the tendon while it heals.
- Physical Therapy(PT): Whether you underwent surgery or not, you will need physical therapy (PT) to regain strength and movement in your Achilles tendon.
- An Achilles tendon rupture is a usual sports injury. People who play sports that include running, frequent stopping and starting, and changing directions are most at risk. You can tear your Achilles tendon at tripping and missing a step going down the stairs or twisting your ankle. With proper treatment, most torn Achilles tendon injuries heal in 4 (four) to 6 (six) months.
Physiotherapy Treatment
- Regardless of the depth and size of the tear, if the patient is compliant and agrees to come after early mobilization strictly conservative treatment is advisable.
- Despite the improving support for accelerated rehabilitation regimes both in surgical and non-surgical situations, there is still no consensus regarding the most preferable protocol, time of beginning, and type of exercises.
- Physiotherapy interventions should be avoided for the 1st two weeks while the patient is asked to avoid any kind of dorsiflexion and immobilize their foot in a boot or plaster of Paris in 30 ° plantar flexion. Weight-bearing is advised to be avoided in the 1st two weeks.
- However, in certain cases, depending on the condition of the surgical treatment, the patient may start to lose approximately five kg of weight with a 25 to 30-degree plantar flexion boot within 24 hours later surgery. This weight is carried out by pressing on the scale below the supervision of a doctor. Afterward, the patient can obtain ready for physical therapy with crutches and boots, with enough support to ‘balance’.
- Quadriceps isometric exercises from the 24-hour period later surgery (due to the tendency of the quadriceps muscle to lose tone fastly). This period is managed along with ankle pumping exercises (to cure edema formation or reduce the resulting edema) & 10 to 15 minutes of cold applications every 2 (two) hours.
Plantar flexion on a step
Later 2 (two) weeks, the patients are encouraged to take their boots off for 3 to 5 minutes every hour or two to do specific exercises. The emphasis is on increasing plantar flexion mobility and Slowly improving the strength of plantarflexion at this stage. Dorsi-flexion stretches, and neutral positions are still not allowed.
Week 4-week 8: Slowly lower the wedge of the boot inserted until the foot reaches neutral at week ten turning on the surgical technique and the presence of co-morbidities.
Early rehabilitation principles:
- Strengthening the foot core
- Avoiding Achilles Tendon stretch: a slightly tight tendon at the end of weeks 9-10 is very much better than an overlengthened tendon that does not create sufficient energy and can probably put the patient at risk of re-rupture.
2. Single leg plantar flexion
- Gait re-education; looking through all the Lower limb joints and correcting any incorrect pattern such as knee hyperextension and decreased Gluteal activation.
- Plantar flexion Strengthening: by isometric and sustained heel raises beginning on both legs and then steadily progressing on a single leg. Holding on one leg and lowering under on the other. One time the patient is satisfactory to proper heel raises on one leg throughout the Range Of Motion (ROM) in a guided manner you can begin working on endurance by doing four sets of six (6) up to 24 repetitions or up to twenty (20) repetitions in a minute. Progress inside eccentric loading by doing heel raises off the border of a box. This can assist to create tension and strength In the tendon.
- Running and rapid walking can be introduced when the patient can easily do a single heel raise.
- Tibialis Posterior works along with Tibialis Anterior and the Peroneal muscles to help the foot core power when progressing into a single-leg stance during the gait. If they are not working correctly, the Achilles tendon and the calf muscle will be overloaded.
- With conservative management, it is recommended to look at your patient once a week to follow up & encourage commitment to fast recuperation and exercises for better results. Unlike surgical treatment where the patient obtains six (6) to 12 weeks follow-ups to off the boot.
- Rehabilitation does not end the minute the patient can obtain their heel off the ground. An assessment of the patient’s function, return to work, and going back to sports if applicable should follow. It is recommended to check out with your patient for 12 months
- The re-rupture is highly evident in the first year yet it can happen later so you want to make sure your patient is fit and integrated into his usual lifestyle.
- Post-surgical protocols which encourage before weight-bearing and mobilization have been developed by Brumannetal and Braunsteinetal.
Look at the following protocols:
- Fowler Kennedy,
- Indiana Total Therapy,
- Ballarat orthopedics.
3. Traditional Approach
- Rehabilitation turns on the initial management approach taken – surgical or non-surgical. However, the patient will usually wear a plaster cast for immobilization or a below-knee dorsal brace which allows the ankle to make a plantar flexion to begin early mobilization. Later the cast or brace is replaced recuperation is important and focused on organically improving the range of movement (ROM) of the ankle, after it is focused on increasing muscle strength and muscle coordination. A return to activities should be anticipated at 4 to 6 months of therapy, yet the rate of rehabilitation considerably turns on the quality of the treatment and the motivation of the patient.
general physical therapy can start immediately with the usual exercises for the affected lower limb:
- Hip abduction,
- Straight leg raise,
- Standing hamstring curl,
- Core exercises such as Plank.
- Once the cast or brace is removed, begin with gentle passive mobilization of the ankle and the subtalar joints and active range of motion (ROM) exercises. After 2 weeks of physiotherapy, progressive resistance exercises are added.
Possible exercises for the patient are:
- Active flexion or extension of the ankle,
- Ankle circles (clockwise and counterclockwise),
- Hip abduction,
- Straight leg raise,
- Standing hamstring curl,
- Cycling upon a stationary bicycle.
8-12 Weeks later Surgery
- Gait training exercises can be begun, come after by activity-specific movements. The patient can begin with Theraband exercises by starting from the lowest resistance and working up from there for regaining strength. The patient should continue with the previous exercises:
Ankle range of motion: plantarflexion or dorsiflexion to 90°: 2 x 8 repetitions,
Ankle range of motion: inversion or eversion,
Ankle range of motion: pronation or supination: 2 x 8 repetitions,
One leg standing balance exercise : 3 × 30 seconds,
Standing heel-rise (2 × 3 seconds tempo) : 3 × 10 repetitions.
12-24 Weeks later Surgery
- The 1st set of exercises can now be executed with ankle weights. The following exercises can be added to the training program, yet basic exercises (described above) should still be executed :
Calf stretch,
Heel raises,
Single-leg balancing,
Walk on your toes with support, to begin with (if needed): 2 × 5 meters,
Standing heel-rise is performed with improved weight on the injured leg: 5 × 10 repetitions,
Heel-rise in a supine position with flexed legs (with increased weight on the injured leg): 2 × 15 repetitions,
Leg press with one leg at a time (10 repetitions maximum): 2 × 10 repetitions,
Balance exercises on a trampoline: 2 × 45 seconds,
Walk or jog on a trampoline: 2 × 45 seconds,
Cross trainer: 1 min and 45 seconds,
Lunges (only with injured leg in front): 2 × 10 repetitions.
Beginning From Week 14 Up to the End of the Therapy
- The patient is able to run approximately 14 weeks later the injury or surgery (always consider the guidance of the surgeon!).
- Jogging upwards on stairs is allowed if the patient can walk five meters on their toes without the heel falling down.
- The last step later in surgery is eccentric exercise. Through the eccentric area (lowering the heel), the patient has full weight on the injured foot, and during the concentric part (raising on tiptoe) only the non-injured foot is utilized.
- The patient takes place on a step, standing with whole body weight on the forefoot of both feet, and the knees are extended. Then he is asked to go stand on his or her toes and to raise the non-injured leg so that his or her body weight is on his injured leg. Now the patient is slowly under the heel. In this way, the calf muscle eccentrically guides the movement and is eccentrically trained.
- When the patient can perform this exercise without discomfort, he or she can increase the load by adding books or other weights to a backpack or perform the exercise with a flexed knee.
- When managed with an eccentric training program, the patient is more likely to be able to return quicker to sport. The eccentric exercises should decrease pain and tendon thickness and should increase the function of the tendon (and muscles). The eccentric calf-muscle exercises, as described under, should be executed two times daily for 12 weeks. The exercise program consists of 1-3 sets of 15 repetitions per exercise, coinciding with the improvement of the patient.
- Yet not all patients benefit similarly from an eccentric exercise program. It is also been proven that these exercises are decreased effective in sedentary people in comparison to athletes.
- Later completing the rehabilitation program, the latest examination of the tendon healing and functions is required
- If required, the latest referral for further physiotherapy sessions can be provided to the patient.
- A slow return to sports is recommended. For example, previous participating to contact sports, the patient should wait at least 6 to 9 months later the injury.
How can I prevent a torn Achilles tendon?
You can not always prevent an accidental injury such as tearing your Achilles tendon. Yet you can take steps to reduce the risk of an Achilles tendon tear, involving:
- Doing warm-up exercises previous a workout or game,
- Improving the intensity of workouts gradually,
- Usually stretching your calf muscles and Achilles’ tendons.
What is the prognosis for people with an Achilles tendon rupture?
- With proper treatment, most Achilles tendon ruptures fully heal within 4 (four) to (six) months.
- Having surgery to repair a torn Achilles tendon is commonly the best option for younger, active people. Later surgical recovery, you can regain your Achilles tendon’s full strength or function.
When should I call the doctor?
You should call your healthcare provider (doctor) if you occur:
- A snap and pop at the back of your ankle during activity,
- Unexpected sharp pain at the back of your ankle,
- Difficulty walking later an injury.
What questions should I ask my doctor?
You may want to tell your healthcare provider (doctor):
- Do I require surgery to repair my Achilles tendon?
- How long will I require to wear a brace or cast?
- When can I begin exercising or playing sports again?
- Am I at risk of tearing my Achilles again later it heals?
Summary
- An Achilles tendon rupture is a usual sports injury. People who play sports that include running, frequent stopping and starting, and changing directions are most at risk. If you trip, miss a step going down the stairs, or twist your ankle, you could tear your Achilles tendon. With proper treatment, most torn Achilles tendon injuries heal in 4 (four) to 6 (six) months.
FAQs
A torn Achilles tendon is a traumatic injury that needs medical attention. Without treatment, an Achilles tendon tear may not heal properly. This can improve your risk of rupturing it again.
If a completely torn Achilles tendon is not treated properly, it may not heal or heal with scar tissue in an elongated position, and the person will not repair enough strength in the leg for normal daily activities such as walking, do alone running, or other athletic activities.
Pain, possibly severe, and swelling close to the heel. An inability to twist the foot downward or “push off” the harmed leg when walking. An inability to stand on the toes of the harmed leg. A popping or snapping sound when the harm happens.
The term called “heal on its own” is a small problem in an Achilles tendon tear. While partial ruptures sometimes “heal on their own,” a physician should be consulted for diagnosis and guidance during rehabilitation. Perfectly, complete tears or ruptures should be evaluated and treated by a physician.
With the assistance of physical therapy, most people can return to normal activity in 4 to 6 months. In physical therapy, you will learn exercises to create your calf muscles stronger or your Achilles tendon more flexible.
Whether managed surgically or nonsurgically, release from a torn Achilles typically takes a certain month. This involves rehab, which is crucial to a whole recovery. Most people who have sustained a torn Achilles tendon and get medical treatment have a very best chance of a positive outcome.
If you rupture your Achilles tendon, you can expect a long recovery. Yet our team of foot and ankle specialists, orthopedic surgeons, and physical therapists will work with you to obtain on your feet and back in the game as soon as possible.