Costoclavicular Syndrome
Table of Contents
What is a Costoclavicular Syndrome?
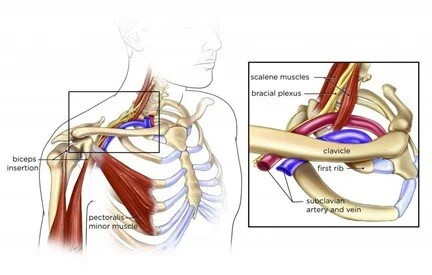
Costoclavicular syndrome, also known as thoracic outlet syndrome (TOS), is a condition characterized by the compression or irritation of the nerves, blood vessels, or both in the thoracic outlet area. The thoracic outlet refers to the space between your collarbone (clavicle) and your first rib.
The superior thoracic outlet and the costoscalene hiatus are the other two passages that make up the thoracic outlet, along with the costoclavicular passage. The clavicle medially, the first rib medially, and the scapula posteriorly make up the costo-clavicular passage. The costoclavicular gap between the first rib and the clavicle contains the brachial nerve plexus, subclavian artery, and subclavian vein. In this location, the neurovascular bundle is susceptible to compression.
When blood vessels or nerves in the area known as the thoracic outlet, which is located between the collarbone and the first rib, are squeezed, a series of illnesses known as thoracic outlet syndrome (TOS) can develop. This may result in achy shoulders, a stiff neck, and numb fingers.
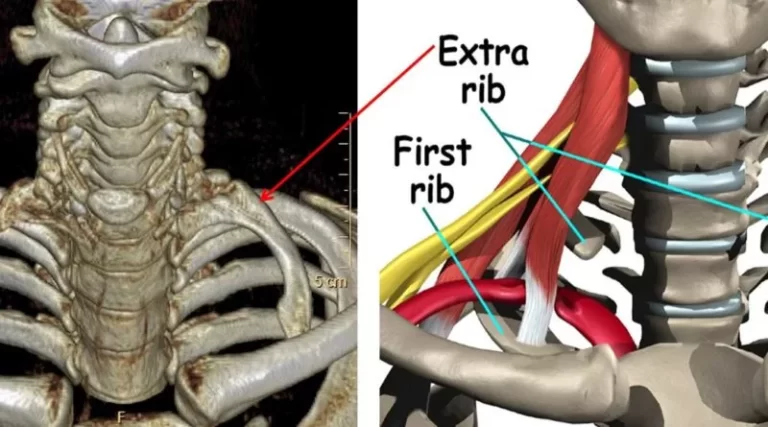
Physical damage from a vehicle accident, recurrent injuries from work or sports, some structural anomalies (such as having an additional rib), and pregnancy are common causes of thoracic outlet syndrome. Thoracic outlet syndrome occasionally has no known aetiology, according to specialists.
The normal course of treatment for thoracic outlet syndrome is physical therapy and painkillers. With these therapies, most patients become well. But occasionally, your doctor could advise surgery.
Mechanism:
As they stood at attention with loaded knapsacks, troops with costoclavicular syndrome experienced pain, numbness, and weariness in their arms. The first rib was compressed by the clavicle moving lower on it, which caused the neurovascular bundle to have a tendency to shear.
Three things could lead to this:
The first rib is depressed by the clavicle. This is evident in the typical postural flaw of rounding and sagging shoulders. Forcing the scapula forward constricts the costoclavicular channel.
This can also happen if your subclavius is too tight. Similar mechanisms are at work in middle-aged or elderly women who are typically obese.
Tight, narrow brassiere straps that support large breasts press directly downward on the clavicles, typically near the intersection of the mid and lateral thirds, and cut into the soft tissues surrounding the shoulders. The neurovascular bundle is severed and the costoclavicular passage is made smaller as a result of the clavicle’s scissor motion against the first rib.
The first rib rises up either toward or away from the clavicle. This frequently happens in patients who have difficulty breathing. This can also happen when the subclavius and anterior and middle scalenes are tight.
The first rib rises as the clavicle descends.
Symptoms of Costoclavicular Syndrome
The main presenting complaints are :
- Discomfort or aching,
- Occasionally stiffness in the neck and shoulders,
- Pain,
- Paraesthesia
- Fatiguability of the upper limbs.
- While often bilateral, the dominant side typically exhibits more pronounced symptoms.
- Work and exercise, especially lifting heavy shopping bags, worsen them.
- Rest and sleep alleviate the symptoms, which are mild or nonexistent in the morning and worsen throughout the day.
- Blue-purple hands can cause patients to complain.
Diagnosis of Costoclavicular Syndrome
Examination:
The deep grooves on both shoulders caused by tight, thin bra straps deeply slicing into the underlying soft tissues are the most crucial diagnostic cues.
A forefinger placed directly downward in the groove causes symptoms to return.
- Tenderness over the acromioclavicular joint is a given. The neck and shoulder can move freely. The latter is painless, however, due to osteoarthritis in the acromioclavicular joint, shoulder movements may be marginally unpleasant.
- There is no weakening or muscle atrophy.
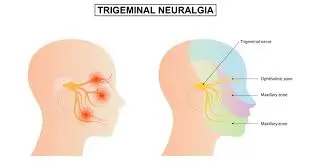
- When present, paresthesia is likely to affect the thumb, all of the fingers, and occasionally the entire leg. In terms of distribution and time, they differ from the paraesthesia caused by carpal tunnel compression.
- Tinel’s Test and Phalen’s Test are not present.
- Puffy blue hands are a complaint from some patients. They are unaffected by cold and do not exhibit the typical Raynaud’s phenomenon of colour changes. The shoulder-hand syndrome is distinguished from the costoclavicular syndrome by the normal appearance of the hand, as opposed to the latter’s glossy, bloated, heated, and hyperaesthetic aspect.
- Patients who suffer from this type of costoclavicular syndrome are typically younger than those who suffer from polymyalgia rheumatic, a condition typically affecting people in their sixties and older. Shoulder stiffness is pronounced and bilateral in polymyalgia rheumatica and may be accompanied by signs of systemic upset or arteritis, such as headache, vision problems, etc. To rule out any further reasons for arm, shoulder, and neck discomfort, great attention must be taken.
- Costoclavicular, military brace, and Eden’s test are positive.
Investigations:
- Regular blood tests, a thorough blood count, an erythrocyte sedimentation rate, and immunological tests for inflammatory arthritis reveal no anomalies.
- Most other illnesses cannot be included in the differential diagnosis due to the lengthy duration of symptoms, normal blood tests, and X-rays typically showing only minor degenerative changes of the acromioclavicular joint and cervical spine.
- It is challenging to show radiologically that the clavicle approaches the first rib when direct downward pressure is applied to the shoulder grooves or during loading. This is because it is technically challenging to place markers on the first rib and acquire radiographs of equivalent quality.
- Acromioclavicular joint subluxation may occasionally be observed.
Treatment of Costoclavicular Syndrome
Medical treatment:
- Medication: To lessen inflammation, lessen discomfort, and promote muscular relaxation, your doctor may give anti-inflammatory drugs, pain relievers, or muscle relaxants. Your doctor may advise taking a blood-thinning medicine if there is a blood clot.
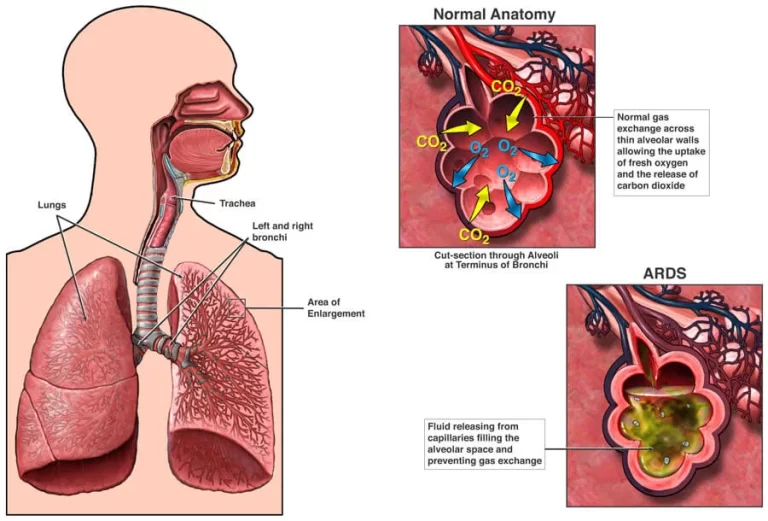
- Medicine to dissolve blood clots: If you have arterial or venous thoracic outlet syndrome with blood clots, your doctor may inject thrombolytics (medicine to dissolve blood clots) into your veins or arteries. Following the administration of thrombolytics, your doctor may recommend anticoagulants, which prevent blood clots.
- Thrombolytic treatment benefits patients with arterial or venous TOS. An IV line or catheter is used to provide medicine that breaks blood clots that have already formed and stop them from growing. Anticoagulant drugs may also be recommended by your doctor.
Surgical treatment:
Options for surgery: If non-invasive therapies have failed if your symptoms are persistent or getting worse, or if you have progressive neurological issues, your doctor may advise surgery.
Surgery is usually necessary for those who have arterial or venous TOS. Surgery may be required for certain sufferers of neurogenic TOS if other therapies are ineffective. Depending on the kind of TOS and your anatomy, the surgeon employs a variety of techniques. For instance, during decompression surgery, aberrant bone or tissue that is compressing the body is removed. To increase blood flow, other operations fix structural issues with your blood arteries. If surgery is necessary, your doctor will let you know what to expect from it. They will also describe any potential hazards.
The operation will be carried out by a surgeon with training in vascular or thoracic (chest) surgery.
Surgery for thoracic outlet syndrome has a risk of side effects, including damage to the brachial plexus. Additionally, surgery may not completely resolve your problems, and they may return.
Thoracic outlet decompression, a surgical procedure used to treat thoracic outlet syndrome, can be carried out in a number of ways. To alleviate compression, these methods require removing a muscle and a part of the first rib. Additionally, to fix constricted blood arteries, surgery can be required.
Your surgeon may use drugs to break blood clots before compressing the thoracic outlet in venous or arterial thoracic outlet syndrome. Before doing a thoracic outlet decompression, your surgeon may in some circumstances perform a treatment to remove a clot from the vein or artery or to repair the vein or artery.
Your surgeon might need to use an artificial graft or a segment of an artery from another region of your body to replace the damaged artery if you have arterial thoracic outlet syndrome. This treatment could be carried out concurrently with the removal of your first rib.
Medical Administration:
- The primary aim is to widen the gap between the clavicle and the first rib.
- Start by working inside the costoclavicular space after applying moist heat to the area for five to ten minutes. This area contains the subclavius muscle, which, when contracted, can constrict the gap by drawing the clavicle and first rib inward. In case fascial adhesions are present, the entire costoclavicular space should be treated in addition to the subclavius. Passively raising the client’s arm up and back into abduction will now passively stretch the tissues of the costoclavicular region. It is simplest to conduct this stretch on a client who is seated or standing. If the client is lying at the side of the table, it can be done with them in a supine position.
- Second, you should exercise any other muscles that can raise the first rib over the clavicle or lower the clavicle into the first rib. Scalenes, pectoralis minor, and pectoralis major are among them.
- The next step is to get rid of the symptoms’ underlying source. Patients must be instructed to wear strapless brassieres or brassieres with wide straps and a pad positioned on the shoulders and strung through the strap. These precautions aid in dispersing the downward force that the straps provide. The straps shouldn’t be overly restricted. Patients should refrain from carrying large shopping bags. The solution to this issue is the usage of a shopping cart.
- Exercises for the shoulder girdle and awareness of posture to prevent stooping are helpful.
Even though it is rare for weight loss to significantly reduce the weight of the breasts, it still helps to feel better overall.
The acromioclavicular joint’s pain and tenderness typically subside with a decrease in the distracting stresses those actions have on the joint. Some people may benefit from mild analgesics, localized ice or heat, or both.
On rare occasions, an injection of a corticosteroid and local anaesthetic may be needed in the acromioclavicular joint. In extreme circumstances, mammoplasty surgery to surgically reduce breast size yields good outcomes.
FAQs:
The CCJ is a synovial aberrant junction that connects the superior side of the first rib, also known as the first costal cartilage, to the inferior surface of the sternal end of the clavicle.
Symptoms and causes of thoracic outlet syndrome from the Mayo Clinic
When blood vessels or nerves in the area known as the thoracic outlet, which is located between the collarbone and the first rib, are compressed, a series of illnesses known as thoracic outlet syndrome (TOS) can develop. This may result in achy shoulders, a stiff neck, and numb fingers.
The principal restriction for the SC joint is provided by the costoclavicular ligament’s orientation to the joint, which anchors the inferior surface of the sternal end of the clavicle to the first rib. The subclavius muscle also helps to stabilize joints.
Encouragement of diaphragmatic breathing aids in lowering these muscles’ level of activity and enlarging the costoclavicular gap. A cautious use of aerobic exercises may help minimize symptoms, especially early in the rehabilitation phase. Vigorous aerobic exercises may elevate the first rib and promote scalene activity.
Costoclavicular, Military Brace, and Eden’s Test
The patient lifts their chest in an exaggerated “at attention” stance as the examiner drags their shoulders back and down to palpate the radial pulse. If the pulse is absent or weakens, the test is positive and could indicate costoclavicular syndrome.