Latrogenic Nerve Injury
Table of Contents
What is a Latrogenic Nerve Injury?
Latrogenic nerve wounds can result from direct careful injury, strain or foothold during sedation, needle cut, tension by outside discharge, tourniquet, projects or orthotic gadgets, and different causes. Among these, the most regular reason for iatrogenic nerve wounds is immediate harm during a medical procedure.
Latrogenic peripheral nerve injury is an extensive social and monetary concern and most cases are preventable. Complexities ought to be alluded to, and managed speedily by experienced specialists, to guarantee the best opportunities for an ideal useful recuperation. Their anticipation ought to be stressed. Their administration ought to incorporate guaranteeing an early conclusion, regulating a proper treatment with restoration, delivering mental help, and giving control of agony. We will address the aetiology, inclining factors, demonstrative methodologies, and the executives’ systems to lessen the frequency of iatrogenic fringe nerve wounds.
Iatrogenic peripheral nerve wounds are to a great extent avoidable. They are a possible wellspring of significant handicaps for the patient and address possibly horrendous complexities, which can influence patients in any careful claim to fame. Furthermore, they are related to significant trouble to the clinical group, extended suit and force a tremendous monetary weight on medical services frameworks. The frequency of fringe nerve injury stays unsure and can go from 0.03% to 0.11%. These sorts of wounds are seldom detailed, and subsequently, there is meagre writing with respect to the variables deciding the result.
Surgeries that are the expected reasons for iatrogenic nerve wounds, for example, carpal tunnel reconstruction (CTR) and bone break-fix, are broadly performed. Notwithstanding, on the off chance that iatrogenic nerve wounds really do result from such methods, the treatment of these wounds can be performed exclusively at a specific place. Subsequently, iatrogenic nerve wounds are typically analyzed and treated just following a critical postponement. Early analysis and treatment of such wounds are emphatically suggested. Thusly, all doctors ought to know about the gamble elements and methods that should be followed while treating patients with iatrogenic nerve wounds.
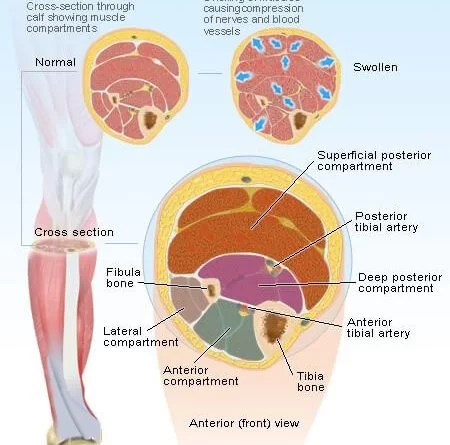
Peripheral nerve wounds are ordinarily credited to inappropriate patient situating and extended medical procedures. Inclining elements, for example, diabetes mellitus, smoking, and a high weight record add to the gamble of a PNI. Peripheral nerve injury can happen whenever pre-operatively and is remembered to emerge from a ceaseless stretch or potential pressure of the weak fringe nerves in constrained positions. The systems that cause the injury are in some cases hard to recognize yet all are by and large preventable and can be immediate, because of prolongation, ischaemia, or potentially delayed pressure. Ischaemia optional to tissue pressure can be the consequence of unfortunate perfusion because of blood vessel impediment and interference of the blood supply of the nerve.
Causes of Latrogenic Nerve Injury
Nerves can become severed, crushed, tied off, pierced, and twisted by screws, or even injured when osteosynthetic devices are removed during surgery. Additionally, they may be thermally harmed by the hardening of bone cement or during coagulation. They may also be stretched by retractor forces. High-risk operations.
The following surgical procedures frequently result in nerve damage:
- Osteotomy and osteosynthesis
- Arthrodesis
- Biopsy of a lymph node in the neck’s posterior triangle
- Surgery for carpal tunnel syndrome
- Surgery for varicose veins
- Removal of the Baker cyst
- Herniorrhaphy of the inguinal region.
Etiology and Inclining Factors:
There are different potential manners by which nerves can be harmed in the perioperative period. PNIs may result from the following events and mechanisms:
- Direct nerve injury;
- Mechanical factors like compression or stretching caused by the retractor;
- Ischaemia;
- Injection solution toxicity;
- Twofold pulverize disorder; or,
- A combination of the aforementioned elements.
Due to preexisting predisposing factors, nerves may be excessively vulnerable to trauma. The median sternotomy in cardiothoracic surgery is associated with a relatively high risk of perioperative injury to nerves of the brachial plexus, with the reported incidence ranging from 6 to 38%. It is shown that specific surgical procedures were associated with a higher incidence of nerve injury (i.e., neurosurgical [8.9%], cardiac [7.1%], general [18%], and orthopaedic [21%] surgeries).
It has been suggested that nerves may become more vulnerable to injury when blood flow is reduced in hypertensive patients. Microvascular changes caused by patient-related factors, such as hypertension, diabetes, and smoking, may make these patients more susceptible to PNI. In a series, it is found that a weight file more noteworthy than 30 is essentially connected with peripheral nerve injury. Prior peripheral neuropathies might incline toward PNI and the ‘twofold squash’ condition, through a change in neuronal homeostasis, may likewise assume a part in these patients. Physical irregularities particularly in the thoracic outlet and at the elbow may likewise incline patients toward PNI. It has been reported that the use of physical restraints indirectly contributed to the injury to the brachial plexus that occurred as a result of traction. Perioperative factors like hypovolaemia, lack of hydration, hypotension, hypoxia, electrolyte aggravations, and hypothermia have been ensnared in the improvement of PNI.
Symptoms of Latrogenic Nerve Injury
- Numbness, whether momentary or ongoing prickling,
- Burning, or tingling sensation
- Pain that is more sensitive to Touch
- Muscle atrophy or deterioration
- Paralysis
- Malfunction of glands or organs
- Impairment of sexual and urinative function
- Sharp, jabbing, throbbing, freezing, or burning pain
- Extreme sensitivity to touch
- Lack of coordination and falling
- Neuromatous or causalgia pain.
Diagnosis:
An exhaustive history combined with a quick definite neurological assessment is the most critical stage in getting an exact finding and afterward in forming a procedure for additional administration. The neurological assessment perceives the kind of injury, the site of the sore, and the seriousness of the engine, tangible or both engine tactile hindrance, which is of prognostic worth.
On the off chance that a deficiency is found, electrophysiological tests are performed to exactly recognize the level of the sore and to survey the potential for recovery. In such a manner, an early meeting with a nervous system specialist is prudent.
Neurapraxia generally has a good prognosis; however, if the diagnosis is unsure, delaying treatment may result in ongoing ischemia or compression, which may worsen the nerve lesion to axonotmesis or even neurotmesis. The choice in regards to careful or moderate treatment is generally accomplished with the guide of clinical assessment and electrodiagnostic tests. Conservative treatment trials are frequently initiated. On the off chance that the nerve doesn’t show recuperation on follow-up assessments, a medical procedure is performed.
Treatment of Latrogenic Nerve Injury
The majority of cases of iatrogenic peripheral nerve injury are avoidable, and they constitute a significant social and economic problem. To ensure the best prospects for an ideal functional recovery, complications should be quickly reported to and treated by skilled surgeons. It’s crucial to concentrate on stopping them. In order to effectively manage them, it is important to ensure early diagnosis, give an effective course of therapy that includes rehabilitation, offer psychological support, and manage pain.
When treating traumatic peripheral nerve injuries, it is crucial to combine morphological examination (neuro sonography) with functional assessment (nerve conduction tests). Intraoperative nerve conduction examines the nerve’s functionality if the nerve appears to be healthy on sonography. Nerve grafting is done if conduction is hindered (which indicates the presence of a neuroma-in-continuity). Neurolysis is carried out if some conduction is retained.
If a severed nerve is discovered during surgery, it should be repaired either right away (primary repair) or within two to three weeks (early secondary repair).
The same is true if a nerve is injured but not completely severed. For every other nerve injury, the same surgical technique is performed. In a perfect world, the repair would be carried out using microsurgical instruments and magnifying equipment to provide maximum visibility.
Once more, this ideal scenario with prompt repair is rarely realized. The damage’s origin is typically unknown. According to our observations, the operative report rarely offers insightful data. We prefer to wait three months with monthly neurological exams when the cause of the lesion is unknown but there is cause to believe that the nerve may repair itself. The nerve should be surgically probed within the following month if the deficiency has not changed or has only slightly improved as of this point. If a neuroma is found during the neurosonographic assessment following nerve exposure, action should be taken immediately. The ideal time for the procedure is three weeks.
If at all possible, a severed nerve should be repaired. Typically, nerve grafting is needed for this. Typically, a source is the lateral calf’s sural nerve. It is also possible to use other cutaneous nerves, such as the saphenous nerve and the medial antebrachial cutaneous nerve. Nerve function in the damaged area is evaluated by intraoperative nerve conduction investigations if the nerve appears to be unharmed.
If conductivity is compromised, the thickened, typically described as a neuroma in continuity, damaged segment of the nerve surrounded by scar tissue is removed and replaced by a transplant. In other circumstances, where conductivity investigations are more encouraging, nerve lysis (the release of the nerve from the reactive tissues around it) is sufficient. Intraoperative neuro sonography has been used recently, making it easier to assess individual nerve fascicles and tell the difference between a complete neuroma in continuity that has no remaining fascicles and a partial lesion that still has functioning fascicles.
Intraoperative neuro sonography has been used recently, making it easier to assess individual nerve fascicles and tell the difference between a complete neuroma in continuity that has no remaining fascicles and a partial lesion that still has functioning fascicles.
Physical therapy is crucial for enhancing the prognosis, both during and after surgery until the damaged muscles have recovered from the deficit. In our opinion, electric stimulation therapy is also beneficial. The muscular architecture can be better preserved in this fashion until nerve regeneration has taken place.
Physiotherapy Management:
Management is directed towards:
The goals of physiotherapy management include:
- Pain Control:
The quality of life is impacted by neuropathic pain, which is a common result of nerve injury. The management of pain must be prioritized. Complete alleviation is uncommon, and 40–60% manage to get some partial relief. A multidisciplinary approach is used, with the pharmacologist(s) contributing the majority of ideas. The drugs that are most frequently prescribed for neuropathic pain include anticonvulsants and tricyclic antidepressants. Other techniques that have been proven useful in trials as supplementary medicine for pain reduction can be used by a physiotherapist. These consist of
Studies have indicated that massage, such as aromatherapy massage, can assist control neuropathic pain and enhance quality of life. Numerous massage treatments have been used, and studies have shown benefits for QOL and pain management.
- TENS: TENS stands for transcutaneous electrical nerve stimulation. TENS application has been reported to help with neuropathic pain relief. It was discovered to be advantageous when employed in continuous mode at 100 Hz.
- (LLLT) Low-Level Laser Therapy: According to studies, this is an effective adjuvant therapy for treating neuropathic pain and neurological impairments since it reduces pain and speeds up the healing process.
- Restorative Practices
- Acupuncture
- Muscle Weakness:
Atrophy of the muscles and functional impairments are side effects of denervation. For the neurological system to govern muscles, the neuromuscular junction (NMJ) must be in good shape. Numerous studies have shown that TENS is effective in preserving the health of the NMJ and in preventing muscular atrophy.
According to the study, TENS therapy was most effective if started one week after the incident and used at a frequency of 100 hertz.
To avoid damaging muscle units, it is crucial to take care of your muscles. In particular, avoid contractures of the muscles as well as heat or cold stress, overstretching caused by gravity, and improper lifting or transfer procedures. The video segments below serve as a solid primer on how to handle passive ROM properly.
To accomplish the aforementioned objectives, physiotherapists use massage, US, hydrotherapy, splints, passive ROM stretches, and accurate transfer skill instruction.
It’s crucial to protect the recovering neural tissue when beginning muscle-strengthening activities; if you experience greater pain, numbness, or pins and needles, the activity is too strenuous and could have an adverse effect on healing.
- Muscle strengthening:
When necessary, muscle-strengthening exercises like isometric, graded weight progression, open-close chains, and the use of support slings to facilitate mobility and support the weight of the limb are used. Additionally, splinting techniques, such as postoperative splinting and casting, as well as splints to prevent deformities from developing, or even to overcome established contractures and improve function, frequently have a place in the treatment of nerve injuries. In order to prevent overstretching and/or contractures, static and dynamic splints might aid to rest paralyzed muscles in the best possible position. They also help unaffected muscles function from the proper posture.
According to a new study, exercise affects adult dorsal root ganglion neurons through a neurotrophin-dependent mechanism, which increases axonal development. For its well-known health benefits, aerobic exercise should also be promoted (aiming for 30 minutes four times per week).
- Functional and sensory deficiencies:
The brain is used to restore visuo-tactile and audio-tactile connections during relearning functional tasks. The development of fine motor skills is prioritized in the upper limb. Balance and coordination are key factors in the lower limb.
Sensitivity can be restored through sensory reeducation. Pinching, tapping, brushing, and icing are frequently utilized in sensory stimulation.
- Proprioception:
Exercise balls, balancing pads for WB exercises, juggling balls for the upper limbs, yoga, and Tai chi can all be used to overcome proprioception impairments.
- Joint Stiffness:
If left in shortened positions, the soft tissues of the area and surrounding regions supplied by the injured nerve are susceptible to contractures. Daily PROM exercises can help prevent these issues, and contracture prevention can also benefit from the use of protective detachable static splints. Ultrasound and laser treatments have been reported to be beneficial for tight joints.
- Emotional tension:
Life-limiting effects of chronic neuropathic pain include emotional stress and a decline in quality of life (QOL). This needs to be respected in order to treat a client with neuropathic pain effectively. The ultimate objective is to improve QOL rather than only relieve pain. Only by addressing sleep, anxiety, and mental health issues can this be accomplished.
Prevention of Injuries to Peripheral Nerve:
- Surgeons and anesthetists’ biggest obstacle in their daily work is positioning patients on the operating table, which necessitates knowledge of the risks associated with the various surgical postures used. Each position has unique dangers that should be weighed against the advantages.
- Careful attention to body alignment is required in situations where pressure or strain on the neurovascular systems is conceivable.
In order to avoid iatrogenic peripheral nerve damage, patients must be positioned for surgery with the appropriate cushioning of bony prominences. - To allow for the best exposure of the surgical site, to protect the nearby structures during surgery, and to maintain the patient’s airway and other vital functions, the torso and limbs must frequently adopt a strained posture.
- Understanding how each patient’s placement may affect them is essential, and a thorough understanding of anatomy, physiology, and body dynamics is essential to establishing a safe positioning. Every patient should be positioned carefully on the operating table to minimize, but not completely eliminate, damage to the peripheral nerves.
- Knowing safe limb positions, being familiar with the local anatomy, and being aware of the most frequent injury sites can all help prevent injuries.
- Both the surgeon and the anesthesiologist are in charge of positioning for surgery, which calls for meticulous planning and open communication between the two teams. The possibility of nerve damage should be known to the anesthetist, and measures to reduce the risk should be taken.
Haemodynamic stability should be preserved, and hypotension should be avoided. The presence of a prior coagulopathy needs to be determined and treated. Patients who already have neuropathy should undergo a cautious evaluation, and the results should be recorded. Reduce the tourniquet pressure and the time it is applied for. - The posterior fossa approach frequently results in the park bench posture, which increases pressure on the ulnar nerve at the level of the elbow due to excessive elbow flexion (>90°).
In order to prevent self-inflicted injuries, psychiatric patients and agitated patients with head injuries are frequently kept immobile during their stay. PNI can result from their improper location. Medical professionals view shackles as a necessary evil and believe that using behavioral therapy and pharmacological restraints instead of restraints should be promoted.
FAQs:
Direct surgical trauma, mechanical stress on a nerve as a result of improper positioning under anaesthesia, the injection of neurotoxic chemicals into a nerve, and other processes can cause iatrogenic nerve damage.
Neuropathy, or nerve damage, can be the outcome of a variety of illnesses like diabetes and even medical procedures like chemotherapy.
There are three different types of nerve injuries: transection (neurotmesis), crush (axonotmesis), and contusions (neuropraxic). Type 1 or 2 nerve injuries are typically linked to closed fractures, dislocations, and forceful trauma. It is rare for a closed injury to cause nerve transection.
Symptoms. Iatrogenic nerve injury is one of the top differential diagnoses when a patient reports tingling (spontaneous discharges in big myelinated fibres), pins and needles (small myelinated fibres), cramping, and burning (unmyelinated fibres) in the area of the surgical treatment.
Functional illnesses such as migraines, epilepsy, vertigo, and neuralgia. Degeneration, including conditions like Parkinson’s disease, lupus, ALS, Huntington chorea, and Alzheimer’s disease.